Coping with the Problems of Diagnosis of Acute Colitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Twisted Bowels: Intestinal Obstruction Blake Briggs, MD Mechanical
Twisted Bowels: Intestinal obstruction Blake Briggs, MD Objectives: define bowel obstructions and their types, pathophysiology, causes, presenting signs/symptoms, diagnosis, and treatment options, as well as the complications associated with them. Bowel Obstruction: the prevention of the normal digestive process as well as intestinal motility. 2 overarching categories: Mechanical obstruction: More common. physical blockage of the GI tract. Can be complete or incomplete. Complete obstruction typically is more severe and more likely requires surgical intervention. Functional obstruction: diffuse loss of intestinal motility and digestion throughout the intestine (e.g. failure of peristalsis). 2 possible locations: Small bowel: more common Large bowel All bowel obstructions have the potential risk of progressing to complete obstruction Mechanical obstruction Pathophysiology Mechanical blockage of flow à dilation of bowel proximal to obstruction à distal bowel is flattened/compressed à Bacteria and swallowed air add to the proximal dilation à loss of intestinal absorptive capacity and progressive loss of fluid across intestinal wall à dehydration and increasing electrolyte abnormalities à emesis with excessive loss of Na, K, H, and Cl à further dilation leads to compression of blood supply à intestinal segment ischemia and resultant necrosis. Signs/Symptoms: The goal of the physical exam in this case is to rule out signs of peritonitis (e.g. ruptured bowel). Colicky abdominal pain Bloating and distention: distention is worse in distal bowel obstruction. Hyperresonance on percussion. Nausea and vomiting: N/V is worse in proximal obstruction. Excessive emesis leads to hyponatremic, hypochloremic metabolic alkalosis with hypokalemia. Dehydration from emesis and fluid shifts results in dry mucus membranes and oliguria Obstipation: severe constipation or complete lack of bowel movements. -

Toxic Colonoscopy—How Investigating Active Inflammatory Bowel Disease
Images in… BMJ Case Reports: first published as 10.1136/bcr-2015-209769 on 22 July 2015. Downloaded from Toxic colonoscopy—how investigating active inflammatory bowel disease can lead to the serious complication of toxic megacolon Shohib Tariq,1 Assad Farooq,1 Ibrar Ali,2 Haren Wijesinghe3 1University Hospital of North DESCRIPTION absent. Abdominal radiograph (figure 2)showed Midlands NHS Trust, Stafford, A 15-year-old girl presented to accident and emer- dilated bowel and CT scanning confirmed toxic mega- West Midlands, UK fi 2Heart of England Foundation gency A&E unable to cope after a week-long colon ( gures 3 and 4), although no perforation. Trust, Birmingham, West history of abdominal pain with vomiting and The patient was made nil by mouth; hydrocorti- Midlands, UK blood-streaked diarrhoea. sone, intravenous cefotaxime and metronidazole 3 University Hospital The patient had been known to the gastroenter- were started as per guidelines.1 Birmingham, Queen Elizabeth, ologist for suspected inflammatory bowel disease With pain improving the following day and radi- Birmingham, West Midlands, UK and was due for an outpatient endoscopy. ology showing improvement in dilation, diet was On examination, the patient was febrile and reintroduced once bowel sounds returned. Correspondence to tachycardic. There were no mouth ulcers or skin There is evidence to suggest colonoscopy2 and Dr Shohib Tariq, changes, however, finger clubbing was present, bowel preparation3 may have caused the exacerba- [email protected] there was guarding and the patient was tender in tion of ulcerative colitis leading to toxic Accepted 9 July 2015 all quadrants. There were no palpable masses or megacolon. -

Etiology and Management of Toxic Megacolon with Human
GASTROENTEROLOGY 1994;107:898-883 Etiology and Management of Toxic Megacolon in Patients With Human lmmunodeficiency Virus Infection LAURENT BEAUGERIE,* YANN NG&* FRANCOIS GOUJARD,’ SHAHIN GHARAKHANIAN,§ FRANCK CARBONNEL,* JACQUELINE LUBOINSKI, ” MICHEL MALAFOSSE,’ WILLY ROZENBAUM,§ and YVES LE QUINTREC* Departments of *Gastroenterology, ‘Surgery, %fectious Diseases, and llPathology, Hdpital Rothschild, Paris, France We report six cases of toxic megacolon in patients with megacolon, we opted for nonsurgical treatment of colonic human immunodeficiency virus (HIV). One case, at an decompression and anti-CMV treatment with a favorable early stage of HIV infection, mimicked a severe attack short-term outcome. of Crohn’s disease, with a negative search for infec- tious agents. Subtotal colectomy was successfully per- Case Report formed with an uneventful postoperative course. The All of the cases of toxic megacolon in patients with five other cases concerned patients with acquired im- HIV seen at Rothschild Hospital between 1988 and 1992 were munodeficiency syndrome at a late stage of immunode- reviewed. During this period, 2430 patients were seen in the ficiency. They were related to Clostridium ditTcile or hospital for HIV infection. Diagnostic criteria for toxic mega- cytomegalovirus (CMV) intestinal infection in two and colon were defined as follows: (1) histologically proven colitis; three patients, respectively. One case of CMV colitis (2) radiological dilatation of the transverse colon on x-ray film presented macroscopically and histologically as pseu- of the abdomen with a colonic diameter above 6 cm at the domembranous colitis. Emergency subtotal colectomy, point of maximum dilatation’*; and (3) evidence of at least performed in the first four patients with acquired immu- two of these following signs’: tachycardia greater than 100 nodeficiency syndrome was followed by a fatal postop beats per minute, body temperature >38.6”C, leukocytosis erative outcome. -

Toxic Megacolon with Colonic Ischemia Masquerading As Diabetic Ketoacidosis: a Case Report F
Saudi Journal of Medical and Pharmaceutical Sciences Abbreviated Key Title: Saudi J Med Pharm Sci ISSN 2413-4929 (Print) |ISSN 2413-4910 (Online) Scholars Middle East Publishers, Dubai, United Arab Emirates Journal homepage: https://saudijournals.com/sjmps Case Report Toxic Megacolon with Colonic Ischemia Masquerading as Diabetic Ketoacidosis: A Case Report F. Mansouri* Department of Pediatrics, King Abdulaziz University, Jeddah, Saudi Arabia DOI: 10.36348/sjmps.2020.v06i01.010 | Received: 03.01.2020 | Accepted: 15.01.2020 | Published: 22.01.2020 *Corresponding author: Mansouri F Abstract A previously healthy 12-year-old boy presented with abdominal pain and clinical and laboratory features highly suggestive of diabetic ketoacidosis. When his blood glucose plummeted and his urinary ketones disappeared within the first hour of insulin therapy, while his abdominal pain, acidosis and hemodynamic status failed to improve despite vigorous fluid resuscitation, the diagnosis of diabetic ketoacidosis was questioned. At laparotomy, gangrenous, hugely dilated large bowel was found, requiring a subtotal colectomy from the cecum to the sigmoid colon; leaving the patient with an ileostomy. The child survived a complicated postoperative course and is currently doing well. Keywords: Ischemic bowel, toxic megacolon, diabetic ketoacidosis. Copyright @ 2020: This is an open-access article distributed under the terms of the Creative Commons Attribution license which permits unrestricted use, distribution, and reproduction in any medium for non-commercial use (NonCommercial, or CC-BY-NC) provided the original author and source are credited. NTRODUCTION never been on any treatment and had been incompliant I with dietary modifications. 4 days prior to presentation, Twenty percent to 40% of children with newly he had progressively worsening episodes of abdominal diagnosed insulin-dependent (type-I) diabetes mellitus pain, mainly in his right lower quadrant (RLQ). -

Megacolon Toxic of Idiophatic Origin: Case Report
DOI: http://dx.doi.org/10.22516/25007440.256 Case report Megacolon toxic of idiophatic origin: case report Sergio Andrés Siado,1 Héctor Conrado Jiménez,2 Carlos Mauricio Martínez Montalvo.3 1 General Surgeon at Clinica Belo Horizonte and Abstract Clinica Medilaser in Neiva, Huila, Colombia 2 Epidemiologist and second year resident in general Toxic megacolon is a pathology whose mortality rate is over 80%. A progressive inflammatory process com- surgery at Universidad Surcolombiana and the promises the colon wall, and secondary dilation of the intestinal lumen occurs due to inflammatory or in- Hospital Universitario Hernando Moncaleano fectious processes. Its clinical presentation is bizarre. but the basic pillars for management are opportune Perdomo in Neiva, Huila, Colombia 3 General Practitioner at the Universidad diagnosis and adequate medical management with antibiotics, water resuscitation, and metabolic correction. Surcolombiana in Neiva, Huila, Colombia If necessary, effective surgical management can prevent the development of complications that worsen the disease and the prognosis of a patient. In this article we present the case of a patient who died after deve- Corresponding author: Carlos Mauricio Martinez Montalvo. [email protected] loping septic shock secondary to toxic megacolon. Cholangitis grade III was suspected, but discarded after ultrasonography, and this resulted in generated distortions in approach and initial management. Due to clinical ......................................... deterioration and abdominal distension, the patient underwent diagnostic laparoscopy which revealed severe Received: 08-08-17 Accepted: 13-04-18 ischemic compromise of the entire colon but without involvement of the small intestine. For this reason, a total colectomy was performed. The pathology report and clinical history ruled out ulcerative colitis or Crohn’s disease which confirmed the diagnosis of toxic megacolon. -

Jejunoileal Diverticulitis: Big Trouble in Small Bowel
Jejunoileal Diverticulitis: Big Trouble in Small Bowel MICHAEL CARUSO DO, HAO LO MD EMERGENCY RADIOLOGY, UMASS MEMORIAL MEDICAL CENTER, WORCESTER, MA LEARNING OBJECTIVES: After excluding Meckel’s diverticulum, less than 30% of reported diverticula occurred in the CASE 1 1. Be aware of the relatively rare diagnoses of jejunoileal jejunum and ileum. HISTORY: 52 year old female with left upper quadrant pain. diverticulosis (non-Meckelian) and diverticulitis. Duodenal diverticula are approximately five times more common than jejunoileal diverticula. FINDINGS: 2.2 cm diverticulum extending from the distal ileum with adjacent induration of the mesenteric fat, consistent with an ileal diverticulitis. 2. Learn the epidemiology, pathophysiology, imaging findings and differential diagnosis of jejunoileal diverticulitis. Diverticulaare sac-like protrusions of the bowel wall, which may be composed of mucosa and submucosa only (pseudodiverticula) or of all CT Findings (2) layers of the bowel wall (true . Usually presents as a focal area of bowel wall thickening most prominent on the mesenteric side of AXIAL AXIAL CORONAL diverticula) the bowel with adjacent inflammation and/or abscess formation . Diverticulitis is the result of When abscess is present, CT findings may include relatively smooth margins, areas of low CASE 2 obstruction of the neck of the attenuation within the mass, rim enhancement after IV contrast administration, gas within the HISTORY: 62 year old female with epigastric and left upper quadrant pain. diverticulum, with subsequent mass, displacement of the surrounding structures, and edema of thickening of the surrounding fat inflammation, perforation and or fascial planes FINDINGS: 4.7 cm diameter out pouching seen arising from the proximal small bowel and associated with adjacent inflammatory stranding. -

Toxic Megacolon with Late Perforation in Campylobacter Colitis
Postgrad Med J: first published as 10.1136/pgmj.69.810.322 on 1 April 1993. Downloaded from 322 CLINICAL REPORTS To our knowledge this is the first report of angiography and surgery makes it unlikely that the recurrent anaemia without frank gastrointestinal ischaemic changes observed were due to cholesterol haemorrhage as a presentation of cholesterol embolism at aortic instrumentation. It is possible embolism. This elderly male patient, athough not that the episode of small bowel obstruction was hypertensive, had many risk factors for this disease: also a sequel of cholesterol embolism, since the he was a diabetic, an ex-smoker and had evidence healing process following an episode of extensive of generalized atherosclerosis. We cannot be cer- mucosal ischaemia can result in concentric fibrosis tain in retrospect for how long cholesterol embo- and narrowing of the bowel lumen.3 lism in the superior mesenteric axis was the source This case illustrates that cholesterol embolism ofblood loss, but right hemicolectomy appeared to should be considered as a possible cause of unex- be curative in this case and no other cause for plained gastrointestinal blood loss in an elderly bleeding was found on close examination of the patient with atherosclerosis. specimen. The interval of one month between References 1. Fine, M.J., Kapoor, W. & Falanga, V. Cholesterol crystal 8. Queen, M., Biem, H.J., Moe, G.W. & Sugar, L. Development embolization: a review of 221 cases in the English literature. of cholesterol embolization after intravenous streptokinase Angiology 1987, 38: 769-784. for acute myocardial infarction. Am J Cardiol 1990, 65: 2. -
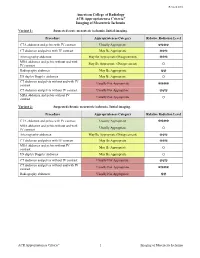
ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia Variant 1: Suspected acute mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ MRA abdomen and pelvis without and with May Be Appropriate (Disagreement) IV contrast O Radiography abdomen May Be Appropriate ☢☢ US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis without IV Usually Not Appropriate contrast O Variant 2: Suspected chronic mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ MRA abdomen and pelvis without and with Usually Appropriate IV contrast O Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ MRA abdomen and pelvis without IV May Be Appropriate contrast O US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ Radiography abdomen Usually Not Appropriate ☢☢ ACR Appropriateness Criteria® 1 Imaging of Mesenteric Ischemia IMAGING OF MESENTERIC ISCHEMIA Expert Panels on Vascular Imaging and Gastrointestinal Imaging: Michael Ginsburg, MDa; Piotr Obara, MDb; Drew L. Lambert, MDc; Michael Hanley, MDd; Michael L. Steigner, MDe; Marc A. Camacho, MD, MSf; Ankur Chandra, MDg; Kevin J. Chang, MDh; Kenneth L. -

Small Bowel Infarction by Aspergillus
short report Haematologica 1997; 82:182-183 SMALL BOWEL INFARCTION BY ASPERGILLUS LUCIO CATALANO, MARCO PICARDI, DARIO ANZIVINO,* LUIGI INSABATO,° ROSARIO NOTARO, BRUNO ROTOLI Cattedre di Ematologia, *Microbiologia e °Anatomia Patologica, Università Federico II, Naples, Italy ABSTRACT Primary gut involvement by Aspergillus is a rare for small bowel perforation. The patient died a and often fatal complication of intensive anti- week later in spite of amphotericin-B treatment leukemic therapy. We describe the case of an adult and neutrophil recovery. Anti-Aspergillus prophy- patient affected by acute leukemia who developed laxis and early introduction of amphotericin-B in a small bowel fungal thromboembolism without the treatment of febrile neutropenia is probably radiographic evidence of lung involvement during advisable in all cases of AML. the post-induction aplastic phase. The diagnosis ©1997, Ferrata Storti Foundation was made histologically at laparotomy performed Key words: Aspergillosis, small bowel, mycotic thromboembolism linical reports of gut involvement by revealed diffuse mycotic infiltration of the intestinal Aspergillus with arterial infarctions are rare.1-3 wall with fungal emboli obturating the lumen of CWe report on an adult male affected by a the superior mesenteric artery branches (Figures 1 favorable subtype of acute myeloid leukemia (AML and 2). Colonies of A. fumigatus grew from bowel M4-Eo) who succumbed to fatal intestinal asper- fragment cultures. Melena persisted despite neu- gillosis (IA) after effective induction treatment. trophil recovery (which was accelerated by adminis- tration of G-CSF at 300 µg/d for 7 days) and treat- Case report ment with 50 mg/d liposomal amphotericin, cho- AML, FAB M4-Eo with cytogenetic evidence of sen because the patient was in severe renal failure inv 16, was diagnosed in a 58-year-old male in (plasma creatinine 5 mg/dL). -

Colonic Ischemia 9/21/14, 9:02 PM
Colonic ischemia 9/21/14, 9:02 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Colonic ischemia Authors Section Editors Deputy Editor Peter Grubel, MD John F Eidt, MD Kathryn A Collins, MD, PhD, FACS J Thomas Lamont, MD Joseph L Mills, Sr, MD Martin Weiser, MD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Aug 2014. | This topic last updated: Aug 25, 2014. INTRODUCTION — Intestinal ischemia is caused by a reduction in blood flow, which can be related to acute arterial occlusion (embolic, thrombotic), venous thrombosis, or hypoperfusion of the mesenteric vasculature causing nonocclusive ischemia. Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting the elderly [1]. Approximately 15 percent of patients with colonic ischemia develop gangrene, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. The remainder develops nongangrenous ischemia, which is usually transient and resolves without sequelae [2]. However, some of these patients will have a more prolonged course or develop long-term complications, such as stricture or chronic ischemic colitis. The diagnosis and treatment of patients can be challenging since colonic ischemia often occurs in patients who are debilitated and have multiple medical problems. The clinical features, diagnosis, and treatment of ischemia affecting the colon and rectum will be reviewed here. Acute and chronic intestinal ischemia of the small intestine are discussed separately. (See "Acute mesenteric ischemia" and "Chronic mesenteric ischemia".) BLOOD SUPPLY OF THE COLON — The circulation to the large intestine and rectum is derived from the superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and internal iliac arteries (figure 1). -

Suzana Buac, PGY3 Dr. Nawar Alkhamesi October 14Th, 2015
COLITIS Suzana Buac, PGY3 Dr. Nawar Alkhamesi October 14th, 2015. Objectives ◦ Anatomy and embryology of colon ◦ Epidemiology and etiology of ulcerative colitis ◦ Differential diagnosis and investigation of ◦ Pathology and histology of ulcerative colitis acute colitis ◦ Clinical presentation, investigation and extra- intestinal manifestations of ulcerative colitis ◦ Presentation, diagnosis and ◦ Medical management of ulcerative colitis (role of management of infectious colitis steroids, 5-ASA, immuno-modulators, biologics) ◦ Presentation, diagnosis and ◦ Screening and risk of malignancy, management management of ischemic colitis of dysplasia ◦ Review of some of the most recent ◦ Elective indications for surgery in ulcerative colitis seminal papers on topic ◦ Emergent indications for surgery in ulcerative colitis ◦ Surgical options in ulcerative colitis Embryology ◦ 3 weeks ◦ Foregut ◦ Midgut ◦ Hindgut ◦ Physiologic herniation ◦ Return to the abdomen ◦ Fixation ◦ Six weeks ◦ Urogenital septum migrates caudally ◦ Separates GI and GU tracts Anatomy ◦ 150cm ◦ Terminal ileum ileocecal valve cecum ◦ Appendix ◦ 3 cm below ileocecal valve ◦ Retrocecal (65%), pelvic (31%), subcecal (2.3%), preileal (1.0%), retroileal (0.4%) ◦ Ascending colon ◦ Hepatic flexure ◦ Transverse colon ◦ Splenic flexure ◦ Descending colon ◦ Sigmoid colon ◦ Rectum Arteries ◦ SMA ◦ Ileocolic ◦ Right colic ◦ Middle colic ◦ IMA ◦ Left colic ◦ Sigmoid branches ◦ Superior rectal artery ◦ Redundancy/communication between the SMA and IMA territories ◦ Marginal artery ◦ Arc of -

An Ileal Duplication Cyst Manifested As an Ileocolic Intussusception in An
Turk J Gastroenterol 2014; 25 (Suppl.-1): 196-8 An ileal duplication cyst manifested as an ileocolic intussusception in an adult xxxxxxxxxxxxxxx Hyun-Soo Kim1, Ji-Youn Sung2, Won Seo Park3, Youn Wha Kim2 1Aerospace Medical Research Center, Republic of Korea Air Force, Chungcheongbuk-do, Republic of Korea 2Department of Pathology, Kyung Hee University Faculty of Medicine, Seoul, Republic of Korea 3Department of Surgery, Kyung Hee University Faculty of Medicine, Seoul, Republic of Korea ABSTRACT An enteric duplication cyst presenting as enterocolic intussusception is an exceptional clinical entity. We herein report a rare case of an ileal duplication cyst that manifested as an ileocolic intussusception. A 19-year-old woman was hospitalized due to right upper quadrant pain. Colonoscopy revealed a polypoid mass protruding into the co- lonic lumen. Ultrasonography demonstrated intussusception with a teardrop-shaped cystic mass at the tip. Com- puted tomography also showed ileocolic intussusception with a 2.5 cm-sized round cystic mass at the tip of intus- susceptum. Microscopically, the cystic wall consisted of a well-defined smooth muscle coat and heterotopic gastric mucosa, consistent with an enteric duplication cyst. This case highlights an ileal duplication cyst as an uncommon cause of adult ileocolic intussusception. To the best of our knowledge, this is the first case of enteric duplication cyst identified as a pathological lead point for enterocolic intussusception in an adult. Enteric duplication cysts should be included in the differential diagnosis of cystic-leading lesions for adult intussusceptions. Keywords: Enteric duplication cyst, enterocolic intussusception, adult Case Report Case INTRODUCTION of an ileal duplication cyst manifested as an ileocolic in- Intussusception occurs when a portion of the diges- tussusception in a young adult woman.