Jejunoileal Diverticulitis: Big Trouble in Small Bowel
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Twisted Bowels: Intestinal Obstruction Blake Briggs, MD Mechanical
Twisted Bowels: Intestinal obstruction Blake Briggs, MD Objectives: define bowel obstructions and their types, pathophysiology, causes, presenting signs/symptoms, diagnosis, and treatment options, as well as the complications associated with them. Bowel Obstruction: the prevention of the normal digestive process as well as intestinal motility. 2 overarching categories: Mechanical obstruction: More common. physical blockage of the GI tract. Can be complete or incomplete. Complete obstruction typically is more severe and more likely requires surgical intervention. Functional obstruction: diffuse loss of intestinal motility and digestion throughout the intestine (e.g. failure of peristalsis). 2 possible locations: Small bowel: more common Large bowel All bowel obstructions have the potential risk of progressing to complete obstruction Mechanical obstruction Pathophysiology Mechanical blockage of flow à dilation of bowel proximal to obstruction à distal bowel is flattened/compressed à Bacteria and swallowed air add to the proximal dilation à loss of intestinal absorptive capacity and progressive loss of fluid across intestinal wall à dehydration and increasing electrolyte abnormalities à emesis with excessive loss of Na, K, H, and Cl à further dilation leads to compression of blood supply à intestinal segment ischemia and resultant necrosis. Signs/Symptoms: The goal of the physical exam in this case is to rule out signs of peritonitis (e.g. ruptured bowel). Colicky abdominal pain Bloating and distention: distention is worse in distal bowel obstruction. Hyperresonance on percussion. Nausea and vomiting: N/V is worse in proximal obstruction. Excessive emesis leads to hyponatremic, hypochloremic metabolic alkalosis with hypokalemia. Dehydration from emesis and fluid shifts results in dry mucus membranes and oliguria Obstipation: severe constipation or complete lack of bowel movements. -

Diverticular Disease 1
WGO Practice Guidelines Diverticular disease 1 World Gastroenterology Organisation Practice Guidelines: Diverticular Disease Core review team: Dr. T. Murphy Prof. R.H. Hunt Prof. M. Fried Dr. J.H. Krabshuis Contents 1 Definitions 2 Epidemiology 3 Etiology 4 Pathophysiology 5 Medical and surgical management 6 Other forms of diverticular disease 7 Global aspects 8 References 9 Useful web sites 10 WGO Practice Guidelines Committee members who contributed to this guideline 11 Queries and feedback 1 Definitions Diverticulum: • A sac-like protrusion of mucosa through the muscular colonic wall [1]. • Protrusion occurs in weak areas of the bowel wall through which blood vessels can penetrate. • Typically 5–10 mm in size. • Diverticula are really pseudodiverticular (false diverticula), as they contain only mucosa and submucosa covered by serosa. Diverticular disease consists of: • Diverticulosis: the presence of diverticula within the colon • Diverticulitis: inflammation of a diverticulum • Diverticular bleeding Types of diverticular disease: © World Gastroenterology Organisation, 2007 WGO Practice Guidelines Diverticular disease 2 • Simple (75%), with no complications • Complicated (25%), with abscesses, fistula, obstruction, peritonitis, and sepsis 2 Epidemiology Prevalence by age [1]: • Age 40: 5% • Age 60: 30% • Age 80: 65% Prevalence by sex: • Age < 50: more common in males • Age 50–70: slight preponderance in women • Age > 70: more common in women Diverticular disease in the young (< 40) Diverticular disease is far more frequent in older people, with only 2–5% of cases occurring in those under 40 years of age. In this younger age group, diverticular disease occurs more frequently in males, with obesity being a major risk factor (present in 84–96% of cases) [2,3]. -

Coping with the Problems of Diagnosis of Acute Colitis
Diagnostic and Interventional Imaging (2013) 94, 793—804 . CONTINUING EDUCATION PROGRAM: FOCUS . Coping with the problems of diagnosis of acute colitis a,∗,c b a E. Delabrousse , F. Ferreira , N. Badet , a b M. Martin , M. Zins a Urinogenital and Digestive Imaging Department, hôpital Jean-Minjoz, CHRU de Besanc¸on, 3, boulevard Fleming, 25030 Besanc¸on, France b Radiology Department, hôpital Saint-Joseph, 184, rue Raymond-Losserand, 75014 Paris, France c EA 4662, Nanomedicine Laboratory, Imagery and Therapeutics, University of Franche-Comté, Besanc¸on, France KEYWORDS Abstract Acute colitis is an acute condition of the colon. For the radiologist, it is mainly Colitis; diagnosed during differential diagnosis of acute abdominal conditions. There are many causes Ischaemia; of colitis and the degree of its severity varies. A CT scan is the best imaging examination for IBD; diagnosing it and also for analysing and characterising colitis. The topography, type of lesion Pseudomembranous; and associated factors can often suggest a precise diagnosis but it is nevertheless essential to Neutropenia integrate these findings into the clinical context and take laboratory values into account. The use of endoscopy is still the rule where a doubt remains, or to obtain necessary histological evidence. © 2013 Éditions françaises de radiologie. Published by Elsevier Masson SAS. All rights reserved. Acute colitis is an acute condition of the colon and most often presents in the form of an acute abdominal picture with very variable clinical symptoms and laboratory test results. The most frequent symptoms encountered in colitis are abdominal pain, fever and diarrhoea [1]. Hyperleucocytosis and elevated CRP in laboratory tests are common. -
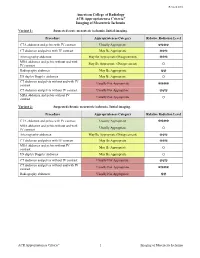
ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia Variant 1: Suspected acute mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ MRA abdomen and pelvis without and with May Be Appropriate (Disagreement) IV contrast O Radiography abdomen May Be Appropriate ☢☢ US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis without IV Usually Not Appropriate contrast O Variant 2: Suspected chronic mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ MRA abdomen and pelvis without and with Usually Appropriate IV contrast O Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ MRA abdomen and pelvis without IV May Be Appropriate contrast O US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ Radiography abdomen Usually Not Appropriate ☢☢ ACR Appropriateness Criteria® 1 Imaging of Mesenteric Ischemia IMAGING OF MESENTERIC ISCHEMIA Expert Panels on Vascular Imaging and Gastrointestinal Imaging: Michael Ginsburg, MDa; Piotr Obara, MDb; Drew L. Lambert, MDc; Michael Hanley, MDd; Michael L. Steigner, MDe; Marc A. Camacho, MD, MSf; Ankur Chandra, MDg; Kevin J. Chang, MDh; Kenneth L. -

Small Bowel Infarction by Aspergillus
short report Haematologica 1997; 82:182-183 SMALL BOWEL INFARCTION BY ASPERGILLUS LUCIO CATALANO, MARCO PICARDI, DARIO ANZIVINO,* LUIGI INSABATO,° ROSARIO NOTARO, BRUNO ROTOLI Cattedre di Ematologia, *Microbiologia e °Anatomia Patologica, Università Federico II, Naples, Italy ABSTRACT Primary gut involvement by Aspergillus is a rare for small bowel perforation. The patient died a and often fatal complication of intensive anti- week later in spite of amphotericin-B treatment leukemic therapy. We describe the case of an adult and neutrophil recovery. Anti-Aspergillus prophy- patient affected by acute leukemia who developed laxis and early introduction of amphotericin-B in a small bowel fungal thromboembolism without the treatment of febrile neutropenia is probably radiographic evidence of lung involvement during advisable in all cases of AML. the post-induction aplastic phase. The diagnosis ©1997, Ferrata Storti Foundation was made histologically at laparotomy performed Key words: Aspergillosis, small bowel, mycotic thromboembolism linical reports of gut involvement by revealed diffuse mycotic infiltration of the intestinal Aspergillus with arterial infarctions are rare.1-3 wall with fungal emboli obturating the lumen of CWe report on an adult male affected by a the superior mesenteric artery branches (Figures 1 favorable subtype of acute myeloid leukemia (AML and 2). Colonies of A. fumigatus grew from bowel M4-Eo) who succumbed to fatal intestinal asper- fragment cultures. Melena persisted despite neu- gillosis (IA) after effective induction treatment. trophil recovery (which was accelerated by adminis- tration of G-CSF at 300 µg/d for 7 days) and treat- Case report ment with 50 mg/d liposomal amphotericin, cho- AML, FAB M4-Eo with cytogenetic evidence of sen because the patient was in severe renal failure inv 16, was diagnosed in a 58-year-old male in (plasma creatinine 5 mg/dL). -

Colonic Ischemia 9/21/14, 9:02 PM
Colonic ischemia 9/21/14, 9:02 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Colonic ischemia Authors Section Editors Deputy Editor Peter Grubel, MD John F Eidt, MD Kathryn A Collins, MD, PhD, FACS J Thomas Lamont, MD Joseph L Mills, Sr, MD Martin Weiser, MD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Aug 2014. | This topic last updated: Aug 25, 2014. INTRODUCTION — Intestinal ischemia is caused by a reduction in blood flow, which can be related to acute arterial occlusion (embolic, thrombotic), venous thrombosis, or hypoperfusion of the mesenteric vasculature causing nonocclusive ischemia. Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting the elderly [1]. Approximately 15 percent of patients with colonic ischemia develop gangrene, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. The remainder develops nongangrenous ischemia, which is usually transient and resolves without sequelae [2]. However, some of these patients will have a more prolonged course or develop long-term complications, such as stricture or chronic ischemic colitis. The diagnosis and treatment of patients can be challenging since colonic ischemia often occurs in patients who are debilitated and have multiple medical problems. The clinical features, diagnosis, and treatment of ischemia affecting the colon and rectum will be reviewed here. Acute and chronic intestinal ischemia of the small intestine are discussed separately. (See "Acute mesenteric ischemia" and "Chronic mesenteric ischemia".) BLOOD SUPPLY OF THE COLON — The circulation to the large intestine and rectum is derived from the superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and internal iliac arteries (figure 1). -

Brief Reports Enteroliths in a Meckel's Diverticulum Mimicking Gallstone
brief reports Enteroliths in a Meckel’s Diverticulum Mimicking Gallstone Ileus Peter G. Justus, MD, James J. Bergman, MD, and Thomas R. Reagan, MD Redmond, W ashington allstone ileus is a form of mechanical obstruction of pain. The recurring symptoms had a duration of several G the small intestine caused by a large gallstone that hours, each time culminating in severe distress lasting 10 has passed from the gallbladder to the intestine through to 15 minutes. Progressive fatigue and episodic anorexia acholecystoenteral fistula.1 This diagnosis is suspected in pursued. He denied fatty food intolerance, jaundice, vom patients with gallstones and symptoms or signs of inter iting, or a past history of gastrointestinal disease. The mittent small-bowel obstruction. family history and other personal history were unremark Meckel’s diverticulum, the most common malformation able. of the gastrointestinal tract, is found in about 2 percent On examination the patient was well nourished and in of individuals.2 Its rare clinical manifestations include in no acute distress. He was normotensive, afebrile, and testinal obstruction, ulceration, hemorrhage, intussus nonicteric. The abdomen was mildly distended, and there ception, and neoplasm. Such phenomena usually are not was mild tenderness to deep palpation of the right upper diagnosed preoperatively.3 Some 50 cases of enteroliths quadrant. No rebound or guarding was elicited, nor were occurring in a Meckel’s diverticulum have been reported.4 there masses noted. Rectal examination was negative, al This unusual finding occurs most often in men and can though some brown, guaiac-positive stool was recovered. present with lower abdominal pain, vomiting,5 rectal The remainder of the physical examination was within bleeding,6 anemia,7 or bowel obstruction.8 Radiographs normal limits. -

An Ileal Duplication Cyst Manifested As an Ileocolic Intussusception in An
Turk J Gastroenterol 2014; 25 (Suppl.-1): 196-8 An ileal duplication cyst manifested as an ileocolic intussusception in an adult xxxxxxxxxxxxxxx Hyun-Soo Kim1, Ji-Youn Sung2, Won Seo Park3, Youn Wha Kim2 1Aerospace Medical Research Center, Republic of Korea Air Force, Chungcheongbuk-do, Republic of Korea 2Department of Pathology, Kyung Hee University Faculty of Medicine, Seoul, Republic of Korea 3Department of Surgery, Kyung Hee University Faculty of Medicine, Seoul, Republic of Korea ABSTRACT An enteric duplication cyst presenting as enterocolic intussusception is an exceptional clinical entity. We herein report a rare case of an ileal duplication cyst that manifested as an ileocolic intussusception. A 19-year-old woman was hospitalized due to right upper quadrant pain. Colonoscopy revealed a polypoid mass protruding into the co- lonic lumen. Ultrasonography demonstrated intussusception with a teardrop-shaped cystic mass at the tip. Com- puted tomography also showed ileocolic intussusception with a 2.5 cm-sized round cystic mass at the tip of intus- susceptum. Microscopically, the cystic wall consisted of a well-defined smooth muscle coat and heterotopic gastric mucosa, consistent with an enteric duplication cyst. This case highlights an ileal duplication cyst as an uncommon cause of adult ileocolic intussusception. To the best of our knowledge, this is the first case of enteric duplication cyst identified as a pathological lead point for enterocolic intussusception in an adult. Enteric duplication cysts should be included in the differential diagnosis of cystic-leading lesions for adult intussusceptions. Keywords: Enteric duplication cyst, enterocolic intussusception, adult Case Report Case INTRODUCTION of an ileal duplication cyst manifested as an ileocolic in- Intussusception occurs when a portion of the diges- tussusception in a young adult woman. -

Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S
Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S. Naval Hospital Sigonella, Sigonella, Italy DWAYNE C. CLARK, M.D., Fond du Lac Regional Clinic, Fond du Lac, Wisconsin Acute abdominal pain is a common presenting complaint in older patients. Presentation may differ from that of the younger patient and is often complicated by coexistent disease, delays in presentation, and physical and social barri- ers. The physical examination can be misleadingly benign, even with catastrophic conditions such as abdominal aortic aneurysm rupture and mesenteric ischemia. Changes that occur in the biliary system because of aging make older patients vulnerable to acute cholecystitis, the most common indication for surgery in this population. In older patients with appendicitis, the initial diagnosis is correct only one half of the time, and there are increased rates of perforation and mortality when compared with younger patients. Medication use, gallstones, and alcohol use increase the risk of pancreatitis, and advanced age is an indicator of poor prognosis for this disease. Diverticulitis is a common cause of abdominal pain in the older patient; in appropriately selected patients, it may be treated on an outpatient basis with oral antibiotics. Small and large bowel obstructions, usually caused by adhesive disease or malignancy, are more common in the aged and often require surgery. Morbidity and mortality among older patients presenting with acute abdominal pain are high, and these patients often require hospitalization with prompt surgical consultation. (Am Fam Physician 2006;74:1537-44. Copyright © 2006 American Academy of Family Physicians.) cute abdominal pain (generally sultation.2,11 In retrospective studies, more defined as pain of less than one than one half of older patients presenting week’s duration) is a common to the emergency department with acute presenting complaint among abdominal pain required hospital admission, Aolder patients. -

Jejunal Diverticula Causing a Life-Threatening Lower
Available online at www.ijmrhs.com cal R edi ese M ar of c l h a & n r H u e o a J l l t h International Journal of Medical Research & a S n ISSN No: 2319-5886 o c i t i Health Sciences, 2019, 8(4): 196-200 e a n n c r e e t s n I • • IJ M R H S Jejunal Diverticula Causing a Life-Threatening Lower Gastrointestinal Bleeding: A Case Report Abdelmoniem MM Makkawi* and Mohammed Eltoum Hamid Azoz Department of Surgery, University of Elimam Elmahadi, Kosti, Sudan *Corresponding e-mail: [email protected] ABSTRACT A jejunal diverticulum is a rare and usually asymptomatic disease. More commonly it is usually seen as incidental findings on radiological studies or during surgery. Complications such as bleeding, perforation, abscess formation, obstruction, malabsorption, blind loop syndrome, volvulus, and intussusception may warrant surgical intervention. Herein, we report a case of a 62-year old woman presenting with massive lower gastrointestinal bleeding, she was pale, clammy and hemodynamically unstable, she was initially resuscitated with IV fluids and whole blood, urgent upper endoscopy was normal, colonoscopy revealed sigmoid colon ulcerative lesion with histopathological evidence of adenocarcinoma, there was bleeding coming from upwards. After staging of the tumor, the decision was then made to proceed to exploratory laparotomy with a pre-operative plan of segmental colectomy. Intra-operatively segmental sigmoid colectomy was performed with end to end anastomosis, during formal laparotomy we found 2 giant diverticula in the proximal jejunum, small bowel resection and end to end anastomosis was done with the good postoperative outcome. -

Delayed Diagnosis of Chronic Mesenteric Ischaemia Woon CYL, Tay KH, Tan SG
Case Report Singapore Med J 2007; 48(1) : e9 Delayed diagnosis of chronic mesenteric ischaemia Woon CYL, Tay KH, Tan SG ABSTRACT peptic ulcer disease and a 30-year smoking history. Chronic mesenteric ischaemia is a rare disease. He first presented with colicky pain in the right Patients typically present with a protracted hypochondrium and epigastrium. He was diagnosed course of vague abdominal symptoms and with acute cholecystitis and underwent open profound weight loss, leading to a delay in cholecystectomy. Recovery was uneventful. Over the diagnosis. If untreated, it progresses to following two years, he was admitted ten times for colicky bowel infarction, which has a poor prognosis. left hypochondriac and epigastric pain, often worse Once diagnosed, however, it can be easily postprandially, poor appetite, diarrhoea, and weight loss remedied via endovascular stenting or open of 13 kg. Abnormalities on blood investigations included surgery. Symptom reversal is prompt and mildly-elevated alkaline phosphatase, gamma glutamyl patients rapidly achieve premorbid habitus. transferase, serum amylase and urine amylase. Repeated We report a 58-year-old man in whom oesophagogastroduodenoscopies (OGDs), colonoscopies, the diagnosis was missed for two years, during barium studies, abdominal computed tomography (CT) which numerous investigations were performed. and magnetic resonance cholangiopancreatography The diagnosis was eventually revealed on scans were normal. He finally underwent a coeliac plexus angiography, and he was cured by mesenteric block for pain relief. bypass surgery. For patients with the triad of Two months later, he returned with similar abdominal chronic, unrelenting weight loss, sitophobia symptoms. Owing to his severely cachectic appearance (food fear) and postprandial abdominal pain, and the persistence of symptoms, the diagnosis of this condition must be considered, and actively CMI was entertained. -

Zenker's Diverticulum and Squamous Esophageal Cancer
Journal of Mind and Medical Sciences Volume 4 | Issue 2 Article 15 2017 Zenker’s diverticulum and squamous esophageal cancer: a case report Ion Dina Carol Davila University, St. Ioan Clinical Hospital, Department of Gastroenterology, Bucharest, Romania Octav Ginghina Carol Davila University, St. Ioan Clinical Hospital, Department of Surgery, Bucharest, Romania Corina D. Toderescu Vasile Goldis Western University of Arad, Faculty of General Medicine, Arad, Romania Cristian Bălălău Carol Davila University, St. Pantelimon Hospital, Department of Surgery, Bucharest, Romania, [email protected] Bianca Galateanu University of Bucharest, Department of Biochemistry and Molecular Biology, Bucharest, Romania See next page for additional authors Follow this and additional works at: http://scholar.valpo.edu/jmms Part of the Medical Sciences Commons, and the Surgery Commons Recommended Citation Dina, Ion; Ginghina, Octav; Toderescu, Corina D.; Bălălău, Cristian; Galateanu, Bianca; Negrei, Carolina; and Iacobescu, Claudia (2017) "Zenker’s diverticulum and squamous esophageal cancer: a case report," Journal of Mind and Medical Sciences: Vol. 4 : Iss. 2 , Article 15. DOI: 10.22543/7674.42.P193197 Available at: http://scholar.valpo.edu/jmms/vol4/iss2/15 This Case Presentation is brought to you for free and open access by ValpoScholar. It has been accepted for inclusion in Journal of Mind and Medical Sciences by an authorized administrator of ValpoScholar. For more information, please contact a ValpoScholar staff member at [email protected]. Zenker’s diverticulum and squamous esophageal cancer: a case report Authors Ion Dina, Octav Ginghina, Corina D. Toderescu, Cristian Bălălău, Bianca Galateanu, Carolina Negrei, and Claudia Iacobescu This case presentation is available in Journal of Mind and Medical Sciences: http://scholar.valpo.edu/jmms/vol4/iss2/15 J Mind Med Sci.