Surveillance and Control of Selected Mosquito-Borne Diseases in Florida
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Investigating the Role of Host TTR-Rbps During SFV4 and MHV-68 Infection
Investigating the role of host TTR-RBPs during SFV4 and MHV-68 infection Thesis submitted in accordance with the requirements of the University of Liverpool for the degree of Doctor in Philosophy by Jamie Casswell October 2019 Contents Figure Contents Page……………………………………………………………………………………7 Table Contents Page…………………………………………………………………………………….9 Acknowledgements……………………………………………………………………………………10 Abbreviations…………………………………………………………………………………………….11 Abstract……………………………………………………………………………………………………..17 1. Chapter 1 Introduction……………………………………………………………………………19 1.1 DNA and RNA viruses ............................................................................. 20 1.2 Taxonomy of eukaryotic viruses ............................................................. 21 1.3 Arboviruses ............................................................................................ 22 1.4 Togaviridae ............................................................................................ 22 1.4.1 Alphaviruses ............................................................................................................................. 23 1.4.1.1 Semliki Forest Virus ........................................................................................................... 25 1.4.1.2 Alphavirus virion structure and structural proteins ......................................................... 26 1.4.1.3 Alphavirus non-structural proteins ................................................................................... 29 1.4.1.4 Alphavirus genome organisation -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Notification Requirements
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2021 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of within the next reporting cycle. a case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 Approved by CSTE: June 2019 within 24 hours of a case meeting the notification criteria, followed by Interim Update Approved by CSTE: April 5, 2020 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2020 electronic transmission. Updated: May 28, 2020 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Page 1 of 5 Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis -

Construção E Aplicação De Hmms De Perfil Para a Detecção E Classificação De Vírus
UNIVERSIDADE DE SÃO PAULO PROGRAMA INTERUNIDADES DE PÓS-GRADUAÇÃO EM BIOINFORMÁTICA Construção e Aplicação de HMMs de Perfil para a Detecção e Classificação de Vírus Miriã Nunes Guimarães SÃO PAULO 2019 Construção e Aplicação de HMMs de Perfil para a Detecção e Classificação de Vírus Miriã Nunes Guimarães Dissertação apresentada à Universidade de São Paulo, como parte das exigências do Programa de Pós-Graduação Interunidades em Bioinformática, para obtenção do título de Mestre em Ciências. Área de Concentração: Bioinformática Orientador: Prof. Dr. Arthur Gruber SÃO PAULO 2019 “Na vida, não existe nada a temer, mas a entender.” Marie Curie Agradecimentos Ao Professor Arthur Gruber pela oportunidade desde o início como estagiária no laboratório, pela orientação neste período de aprendizado no mestrado e por fornecer um ambiente de trabalho favorável. À aluna de doutorado Liliane Santana Oliveira que aguentou todas as minhas amolações diárias no laboratório pelo Hangouts, por dúvidas que eram erros meus em comandos de execução, pela paciência, pela amizade, pela companhia nos bandejões da faculdade com cardápio glutenfree que nem sempre eram tão bons assim. À aluna de mestrado Irina Yuri Kawashima que estava comigo no laboratório diariamente, pelas várias discussões sobre o mundo dos vírus e de conhecimentos da bioinformática, pelas ferramentas para facilitar o andamento do projeto, por todas guloseimas glutenfree que seria impossível eu não agradecer pois tenho ciência que não vou encontrar outra amiga masterchef assim. À Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) pelo financiamento durante estes 24 meses de mestrado. Aos meus pais pelo carinho e preocupação comigo durante estes 24 anos, pelo incentivo aos estudos e pelo apoio para eu me manter a uma distância de quase 400km de pura saudade. -

Study of Chikungunya Virus Entry and Host Response to Infection Marie Cresson
Study of chikungunya virus entry and host response to infection Marie Cresson To cite this version: Marie Cresson. Study of chikungunya virus entry and host response to infection. Virology. Uni- versité de Lyon; Institut Pasteur of Shanghai. Chinese Academy of Sciences, 2019. English. NNT : 2019LYSE1050. tel-03270900 HAL Id: tel-03270900 https://tel.archives-ouvertes.fr/tel-03270900 Submitted on 25 Jun 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. N°d’ordre NNT : 2019LYSE1050 THESE de DOCTORAT DE L’UNIVERSITE DE LYON opérée au sein de l’Université Claude Bernard Lyon 1 Ecole Doctorale N° 341 – E2M2 Evolution, Ecosystèmes, Microbiologie, Modélisation Spécialité de doctorat : Biologie Discipline : Virologie Soutenue publiquement le 15/04/2019, par : Marie Cresson Study of chikungunya virus entry and host response to infection Devant le jury composé de : Choumet Valérie - Chargée de recherche - Institut Pasteur Paris Rapporteure Meng Guangxun - Professeur - Institut Pasteur Shanghai Rapporteur Lozach Pierre-Yves - Chargé de recherche - CHU d'Heidelberg Rapporteur Kretz Carole - Professeure - Université Claude Bernard Lyon 1 Examinatrice Roques Pierre - Directeur de recherche - CEA Fontenay-aux-Roses Examinateur Maisse-Paradisi Carine - Chargée de recherche - INRA Directrice de thèse Lavillette Dimitri - Professeur - Institut Pasteur Shanghai Co-directeur de thèse 2 UNIVERSITE CLAUDE BERNARD - LYON 1 Président de l’Université M. -

2018 DSHS Arbovirus Activity
Health and Human Texas Department of State Services Health Services Arbovirus Activity in Texas 2018 Surveillance Report August 2019 Texas Department of State Health Services Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California (CAL) serogroup viruses, chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2018, reported human arboviral disease cases were attributed to WNV (82%), DENV (11%), CHIKV (4%), ZIKV (2%), and CAL (1%) (Table 1). In addition, there were two cases reported as arbovirus disease cases which could not be diagnostically or epidemiologically differentiated between DENV and ZIKV. Animal infections or disease caused by WNV and SLEV were also reported during 2018. Local transmission of DENV, SLEV, and WNV was documented during 2018 (Figure 1). No reports of EEEV or WEEV were received during 2018. Table 1. Year-End Arbovirus Activity Summary, Texas, 2018 Positive Human* Arbovirus Mosquito Avian Equine TOTAL TOTAL Fever Neuroinvasive Severe Deaths PVD‡ Pools (Human) CAL 1 1 1 CHIK 7 7 7 DEN 20 20 20 SLE 2 0 2 WN 1,021 6 19 38 108 146 11 24 1,192 Zika** 4 4 TOTAL 1,023 6 19 65 109 0 178 11 24 1,226 CAL - California serogroup includes California encephalitis, Jamestown Canyon, Keystone, La Crosse, Snowshoe hare and Trivittatus viruses CHIK - Chikungunya DEN - Dengue SLE - Saint Louis encephalitis WN - West Nile ‡PVD - Presumptive viremic blood donors are people who had no symptoms at the time of donating blood through a blood collection agency, but whose blood tested positive when screened for the presence of West Nile virus or Zika virus. -
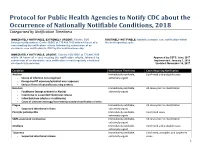
Protocol for Public Health Agencies to Notify CDC About the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification within Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of a the next reporting cycle. case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 within 24 hours of a case meeting the notification criteria, followed by Approved by CSTE: June 2017 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2018 electronic transmission. Updated: November 16, 2017 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis Immediately notifiable, Confirmed cases extremely -

Taxonomy of the Family Arenaviridae and the Order Bunyavirales: Update 2018
Archives of Virology https://doi.org/10.1007/s00705-018-3843-5 VIROLOGY DIVISION NEWS Taxonomy of the family Arenaviridae and the order Bunyavirales: update 2018 Piet Maes1 · Sergey V. Alkhovsky2 · Yīmíng Bào3 · Martin Beer4 · Monica Birkhead5 · Thomas Briese6 · Michael J. Buchmeier7 · Charles H. Calisher8 · Rémi N. Charrel9 · Il Ryong Choi10 · Christopher S. Clegg11 · Juan Carlos de la Torre12 · Eric Delwart13,14 · Joseph L. DeRisi15 · Patrick L. Di Bello16 · Francesco Di Serio17 · Michele Digiaro18 · Valerian V. Dolja19 · Christian Drosten20,21,22 · Tobiasz Z. Druciarek16 · Jiang Du23 · Hideki Ebihara24 · Toufc Elbeaino18 · Rose C. Gergerich16 · Amethyst N. Gillis25 · Jean‑Paul J. Gonzalez26 · Anne‑Lise Haenni27 · Jussi Hepojoki28,29 · Udo Hetzel29,30 · Thiện Hồ16 · Ní Hóng31 · Rakesh K. Jain32 · Petrus Jansen van Vuren5,33 · Qi Jin34,35 · Miranda Gilda Jonson36 · Sandra Junglen20,22 · Karen E. Keller37 · Alan Kemp5 · Anja Kipar29,30 · Nikola O. Kondov13 · Eugene V. Koonin38 · Richard Kormelink39 · Yegor Korzyukov28 · Mart Krupovic40 · Amy J. Lambert41 · Alma G. Laney42 · Matthew LeBreton43 · Igor S. Lukashevich44 · Marco Marklewitz20,22 · Wanda Markotter5,33 · Giovanni P. Martelli45 · Robert R. Martin37 · Nicole Mielke‑Ehret46 · Hans‑Peter Mühlbach46 · Beatriz Navarro17 · Terry Fei Fan Ng14 · Márcio Roberto Teixeira Nunes47,48 · Gustavo Palacios49 · Janusz T. Pawęska5,33 · Clarence J. Peters50 · Alexander Plyusnin28 · Sheli R. Radoshitzky49 · Víctor Romanowski51 · Pertteli Salmenperä28,52 · Maria S. Salvato53 · Hélène Sanfaçon54 · Takahide Sasaya55 · Connie Schmaljohn49 · Bradley S. Schneider25 · Yukio Shirako56 · Stuart Siddell57 · Tarja A. Sironen28 · Mark D. Stenglein58 · Nadia Storm5 · Harikishan Sudini59 · Robert B. Tesh48 · Ioannis E. Tzanetakis16 · Mangala Uppala59 · Olli Vapalahti28,30,60 · Nikos Vasilakis48 · Peter J. Walker61 · Guópíng Wáng31 · Lìpíng Wáng31 · Yànxiăng Wáng31 · Tàiyún Wèi62 · Michael R. -

Western Equine Encephalitis Virus Is a Recombinant Virus (RNA Recombination/Alphavirus/Evolution of RNA Viruses) CHANG S
Proc. Natl. Acad. Sci. USA Vol. 85, pp. 5997-6001, August 1988 Evolution Western equine encephalitis virus is a recombinant virus (RNA recombination/Alphavirus/evolution of RNA viruses) CHANG S. HAHN, SHLOMO LUSTIG*, ELLEN G. STRAUSS, AND JAMES H. STRAUSSt Division of Biology, 156-29, California Institute of Technology, Pasadena, CA 91125 Communicated by James Bonner, April 14, 1988 ABSTRACT The alphaviruses are a group of 26 mosquito- virus; O'Nyong-nyong virus; and Ross River virus. Sindbis borne viruses that cause a variety of human diseases. Many of and Semliki Forest viruses have been intensively studied as the New World alphaviruses cause encephalitis, whereas the models for alphavirus replication (7). Sindbis virus is widely Old World viruses more typically cause fever, rash, and distributed, being found in Europe, India, southeast Asia, arthralgia. The genome is a single-stranded nonsegmented Australia, and Africa. Close relatives of this virus, such as RNA molecule of + polarity; it is about 11,700 nucleotides in Ockelbo virus in Europe (8) and Babanki virus in Africa, length. Several alphavirus genomes have been sequenced in cause disease in humans characterized by fever, rash, and whole or in part, and these sequences demonstrate that alpha- arthritis. Chikungunya and O'Nyong-nyong viruses have viruses have descended from a common ancestor by divergent caused large epidemics in Africa of a dengue-like disease also evolution. We have now obtained the sequence of the 3'- characterized by fever, rash, and arthralgia. Ross River virus terminal 4288 nucleotides of the RNA of the New World is the causative agent of epidemic polyarthritis in Australia Alphavirus western equine encephalitis virus (WEEV). -

DSHS Arbovirus Activity 061817
Arbovirus Activity in Texas 2017 Surveillance Report June 2018 Texas Department of State Health Services Infectious Disease Control Unit Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California serogroup viruses (CAL), chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2017, reported human arboviral disease cases were attributed to WNV (54%), ZIKV (22%), DENV (17%), and CHIKV (6%) (Table 1). Animal infections or disease caused by CAL, EEEV, SLEV, and WNV were also reported during 2017. Table 1. Year-End Arbovirus Activity Summary, Texas, 2017 California Serogroup Viruses California serogroup viruses (CAL) are bunyaviruses and include California encephalitis virus (CEV), Jamestown Canyon virus, Keystone virus, La Crosse virus (LACV), snowshoe hare virus, and Trivittatus virus. These viruses are maintained in a cycle between mosquito vectors and vertebrate hosts in forest habitats. In the United States (U.S.), approximately 80-100 reported cases of human neuroinvasive disease are caused by LACV each year (CDC), mostly in mid-Atlantic and southeastern states. From 2002-2016, Texas reported a total of 5 cases of human CAL disease (range: 0-3 cases/year): 1 case of CEV neuroinvasive disease and 4 cases of LACV neuroinvasive disease. In 2017, one CEV-positive mosquito pool was identified in Orange County (Figure 1); no human cases of CAL disease were reported. -

Prevalence and Determinants of Black Water Fever in Malaria
Jebmh.com Original Research Article Prevalence and Determinants of Black Water Fever in Malaria Manoj Kumar Mohapatra1, Prafulla Kumar Bariha2, Samir Jena3, Kshetra Mohan Tudu4, Ravi Kumar G. N.5, Sumeet Kumar Sahu6, Dhiraj Kumar Lenka7, Gayatri C.8 1Professor, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. 2Assistant Professor, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. 3Junior Resident, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. 4Junior Resident, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. 5Junior Resident, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. 6Junior Resident, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. 7Junior Resident, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. 8Junior Resident, Department of General Medicine, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. ABSTRACT BACKGROUND Study on black-water fever in malaria is less common in India. Early diagnosis and Corresponding Author: treatment can save the life of the patient. Therefore, we studied the clinical Dr. Prafulla Kumar Bariha, Assistant Professor, features, risk factors and outcome of black-water fever with malaria. Veer Surendra Sai Institute of Medical Sciences and Research, METHODS Burla, Odisha, India. The study was carried out at Department of Medicine, VIMSAR, Burla, Sambalpur, E-mail: [email protected] Odisha. -

Medical Aspects of Biological Warfare
Alphavirus Encephalitides Chapter 20 ALPHAVIRUS ENCEPHALITIDES SHELLEY P. HONNOLD, DVM, PhD*; ERIC C. MOSSEL, PhD†; LESLEY C. DUPUY, PhD‡; ELAINE M. MORAZZANI, PhD§; SHANNON S. MARTIN, PhD¥; MARY KATE HART, PhD¶; GEORGE V. LUDWIG, PhD**; MICHAEL D. PARKER, PhD††; JONATHAN F. SMITH, PhD‡‡; DOUGLAS S. REED, PhD§§; and PAMELA J. GLASS, PhD¥¥ INTRODUCTION HISTORY AND SIGNIFICANCE ANTIGENICITY AND EPIDEMIOLOGY Antigenic and Genetic Relationships Epidemiology and Ecology STRUCTURE AND REPLICATION OF ALPHAVIRUSES Virion Structure PATHOGENESIS CLINICAL DISEASE AND DIAGNOSIS Venezuelan Equine Encephalitis Eastern Equine Encephalitis Western Equine Encephalitis Differential Diagnosis of Alphavirus Encephalitis Medical Management and Prevention IMMUNOPROPHYLAXIS Relevant Immune Effector Mechanisms Passive Immunization Active Immunization THERAPEUTICS SUMMARY 479 244-949 DLA DS.indb 479 6/4/18 11:58 AM Medical Aspects of Biological Warfare *Lieutenant Colonel, Veterinary Corps, US Army; Director, Research Support and Chief, Pathology Division, US Army Medical Research Institute of Infectious Diseases, 1425 Porter Street, Fort Detrick, Maryland 21702; formerly, Biodefense Research Pathologist, Pathology Division, US Army Medical Research Institute of Infectious Diseases, 1425 Porter Street, Fort Detrick, Maryland †Major, Medical Service Corps, US Army Reserve; Microbiologist, Division of Virology, US Army Medical Research Institute of Infectious Diseases, 1425 Porter Street, Fort Detrick, Maryland 21702; formerly, Science and Technology Advisor, Detachment