Introduction Four Hand Injuries Not to Miss Ulnar Collateral Ligament Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
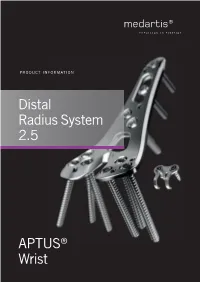
Distal Radius System 2.5
PRODUCT INFORMATION Distal Radius System 2.5 APTUS® Wrist 2 | Distal Radius System 2.5 Contents 3 A New Generation of Radius Plates 4 One System for Primary and Secondary Reconstruction 6 ADAPTIVE II Distal Radius Plates 8 FPL Plates 10 Hook Plates 11 Lunate Facet Plates 12 Rim Plates 13 Fracture Plates 14 Correction Plates 15 Volar Frame Plates 16 Extra-Articular Plates 17 Small Fragment Plates 18 Dorsal Frame Plates 19 XL Plates 20 Distal Ulna Plates 21 Fracture Treatment Concept 22 Technology, Biomechanics, Screw Features 24 Precisely Guided Screw Placement 25 Instrument for Reconstruction of the Volar Tilt 26 Storage 27 Overview Screw Trajectories 29 Ordering Information 47 Bibliography For further information regarding the APTUS product line visit: www.medartis.com Medartis, APTUS, MODUS, TriLock, HexaDrive and SpeedTip are registered trademarks of Medartis AG / Medartis Holding AG, 4057 Basel, Switzerland www.medartis.com Distal Radius System 2.5 | 3 A New Generation of Radius Plates Why is a new generation of radius plates needed? Distal radius fractures are the most common fractures of the stable plate systems have enabled open reduction and inter- upper extremities. The knowledge of these fractures has grown nal fixation to become an established treatment method for enormously over the last years. Treatment concepts have like- intra- and extra-articular distal radius fractures. These sys- wise been refined. It is now generally accepted that the best tems have enabled even severe extension fractures with dor- possible anatomical reconstruction of the radiocarpal joint sal defect zones to be precisely repositioned and treated with (RCJ) and distal radioulnar joint (DRUJ) to produce a func- osteosynthesis via volar access without the need for additional tional outcome is a requirement. -

6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -

Sustentaculum Lunatum: Appreciation of the Palmar Lunate Facet in Management of Complex Intra-Articular Fractures of the Distal Radius
A Review Paper Sustentaculum Lunatum: Appreciation of the Palmar Lunate Facet in Management of Complex Intra-Articular Fractures of the Distal Radius Ebrahim Paryavi, MD, MPH, Matthew W. Christian, MD, W. Andrew Eglseder, MD, and Raymond A. Pensy, MD key role in restoring the anatomy of the palmar distal radial Abstract metaphysis during internal fixation. This fragment in com- Fracture of the distal radius is the most common wrist minuted fractures was first ascribed special importance by injury. Treatment of complex intra-articular fractures of Melone5 in his description of common fracture patterns. In the distal radius requires an accurate diagnosis of the the present article, we describe the anatomical characteristics fracture pattern and a thoughtful approach to fixation. of the sustentaculum lunatum and the clinical relevance of We propose a new term, sustentaculum lunatum, for this fragment to management of fractures of the distal radius. the palmar lunate facet. The sustentaculum lunatum deserves specific attention because of its importance Classification in load transmission across the radiocarpal joint. It is A variety of classification systems have been proposed to char- acterize and guide treatment of fractures of the distal radius. also key to restoring the anatomy of the palmarAJO distal The earliest descriptions of fracture patterns were presented by radial metaphysis during internal fixation. We provide Castaing6 and Frykman7 in the 1960s. The Frykman classifica- a review of the structure and function of the susten- tion historically has been popular but is limited in accuracy in taculum lunatum and describe fixation techniques. This its characterization of fragments and their displacement and is article is intended to promote awareness of this frag- limited in its ability to guide treatment. -

Palmar Plating of Distal Radius Fractures – Pearls and Pitfalls
Palmar Plating of Distal Radius Fractures – Pearls and Pitfalls Michael S. Bednar, M.D. Chief, Hand Surgery Professor, Dept. of Ortho Surgery & Rehab Loyola University – Chicago Disclosure n Consultant – Biomet/Zimmer Evolution in Treatment of Distal Radius Fractures 1 External Fixation and Percutaneous Pinning External Fixation and Percutaneous Pinning External Fixation 2 Percutaneous Pinning Percutaneous Pinning Old ORIF concept: n Dorsally displaced = Dorsal plate n Palmarly displaced = Palmar plate 3 Goals of Treatment n ORIF n Indications n Displaced palmar intra and extra- articular fractures ORIF n Palmar Barton and Smith Fractures n ORIF is accepted form of treatment n Palmar plate is well tolerated n Exposure radial to FCR has low morbidity 4 Cohort Studies Volar Fixed Angle n Orbay, J. L., Fernandez, D.L. (2002). 31 partients n Kamano, M., Y. Honda, et al. (2002). 33 patients Follows the contour of the subchondral bone Pegs and screw locked into plate support articular surface when placed directed under the subchondral bone. 5 Distally angled pegs neutralize dorsal forces Joint Reaction Force §.Volar buttress neutralizes volar forces Volar locking plating indications • Dorsal or palmar angulation • Intra-articular fractures • Comminuted fractures • Osteopenia Volar locking plating indications • Dorsal or palmar angulation • Intra-articular fractures • Comminuted fractures • Osteopenia 6 3 Months Post OP Wrist Fractures = ORIF 7 ORIF 8 No metal over radial styloid, causes tendon ruputure Complications – Wrong Fracture Type n -

Locking Versus Nonlocking Palmar Plate Fixation of Distal Radius Fractures
n Feature Article SPOTLIGHT ON upper extremity Locking Versus Nonlocking Palmar Plate Fixation of Distal Radius Fractures MICHAEL OSTI, MD; CHRISTOPH MITTLER, MD; RICHARD ZINNECKER, MD; CHRISTOPH WESTREICHER, MD; CLEMENS ALLHOFF, MD; KARL PETER BENEDETTO, MD abstract Full article available online at Healio.com/Orthopedics. Search: 20121023-18 This study compared functional and radiological outcomes after treatment of extension- type distal radius fractures with conventional titanium nonlocking T-plates or titanium 1.5-mm locking plates. A total of 60 patients were included and followed for 4 to 7 years after receiving nonlocking T-plates (group A; n530) or locking plates (group B; n530) with and without dorsal bone grafting. Bone grafting was significantly more of- ten performed in the nonlocking group to increase dorsal fracture fixation and stability (P,.003). Pre- and postoperative and follow-up values for palmar tilt, radial inclination, radial shortening, and ulnar variance were recorded. Age, sex, and fracture type were similarly distributed between the 2 groups. Postoperative and follow-up evaluation re- vealed equal allocation of intra-articular step formation and osteoarthritic changes to both groups. The overall complication rate was 25%. Compared with the nonlocking system, patients undergoing locking plate fixation presented with statistically signifi- cantly better values for postoperative palmar tilt (5.53° vs 8.15°; P,.02) and radial incli- nation (22.13° vs 25.03°; P,.02). However, forearm pronation was significantly better in group A (P,.005). At follow-up, radial inclination tended to approach a statistically significant difference in favor of group B. All clinical assessment, including Mayo wrist score, Disabilities of the Arm, Shoulder, and Hand score, Green and O’Brien score, Gartland and Werley score, visual analog scale score, and grip strength, yielded no statistically significant difference between the 2 groups. -

Palmar and Dorsal Fixed-Angle Plates in AO C-Type
Jakubietz et al. Journal of Orthopaedic Surgery and Research 2012, 7:8 http://www.josr-online.com/content/7/1/8 RESEARCH ARTICLE Open Access Palmar and dorsal fixed-angle plates in AO C-type fractures of the distal radius: is there an advantage of palmar plates in the long term? Michael G Jakubietz1*, Joerg G Gruenert2 and Rafael G Jakubietz1 Abstract Background: Current surgical approaches to the distal radius include dorsal and palmar plate fixation. While palmar plates have gained widespread popularity, few reports have provided data on long term clinical outcomes in comparison. This paper reports the result of a randomised clinical study comparing dorsal Pi plates and palmar, angle-stable plates for treatment of comminuted, intraarticular fractures of the distal radius over the course of twelve months. Methods: 42 patients with unilateral, intraarticular fractures of the distal radius were included and randomised to 2 groups, 22 were treated with a palmar plate, 20 received a dorsal Pi-plate. Results were evaluated after 6 weeks, 3, 6 and 12 months postoperatively focussing on functional recovery as well as radiological results. Results: The palmar plate group demonstrated significantly better results regarding range of motion and grip strength over the course of 12 months. While a comparable increase in function was observed in both groups, the better results from the early postoperative period in the palmar plate group prevailed over the whole course. Radiological results showed a significantly increased palmar tilt and carpal sag in dorsal plates, with other radiological parameters being comparable. Pain levels were decreased in dorsal plates after hardware removal and failed to show significant differences after 12 months. -

TMPR™ Total Metacarpophalangeal Replacement Operative Technique
TMPR™ Total Metacarpophalangeal Replacement Operative Technique Balanced Natural Movement Contents Section 1 | Introduction 3 Section 2 | Operative technique 4 Contents Section 3 | Inventory 12 Section 4 | Sizing chart 13 Manufactured by MatOrtho Limited 13 Mole Business Park | Randalls Road | Leatherhead | Surrey | KT22 7BA | United Kingdom T: +44 (0)1372 224200 | [email protected] For more information visit: www.MatOrtho.com © MatOrtho Limited 2016. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording or any information storage and retrieval system. 2 | TMPR™ Total Metacarpophalangeal Replacement | Operative Technique Section 1 | TMPR™ implant design features Construction is of standard joint replacement materials i.e. cobalt chrome and ultrahigh molecular weight polyethylene. The metacarpal bearing is a section of a sphere narrowed from side to side, with an offset centre of rotation which provides a cam action to tighten the collateral ligaments during flexion. The dorsal surface has a groove for the location of the extensor tendon. Flanges cover the front and back of the Introduction metacarpal neck which is otherwise cut square. The phalangeal surface is a disc with a shallow concave surface congruent with the metacarpal head. Both implant stems extend to the mid shaft to spread the fixation stresses. The thin metacarpal stem slides in a separate polyethylene plug. The metacarpal plug has thin flexible fins in the shape of truncated triangles conforming to the endosteal surface. The phalangeal stem bears similar fins in the shape of rounded rectangles conforming to the proximal phalanx canal. -

Four Hand Injuries Not to Miss: Avoiding Pitfalls in the Emergency Department Philip Yoonga, Catherine A
Review 1 Four hand injuries not to miss: avoiding pitfalls in the emergency department Philip Yoonga, Catherine A. Johnsona, Edward Yoongc and Adrian Chojnowskib The clinical and radiological findings in some hand injuries European Journal of Emergency Medicine 2011, 00:000–000 can be subtle and easily misinterpreted, leading to Keywords: emergency medicine, hand injuries, upper extremity, wounds irreversible changes and profound functional loss. The and injuries importance of early and accurate diagnosis is clear. This aNorwich Radiology Academy, bDepartment of Trauma and Orthopaedics, Norfolk and Norwich University Hospital, Norwich, Norfolk and cSchool of Medicine, study looks at four such injuries, with reference to pertinent University of Manchester, Manchester, UK anatomy, typical mechanisms of injury, examination and Correspondence to Dr Philip Yoong, MBBS, Norwich Radiology Academy, radiological findings, with emphasis on avoiding pitfalls Cotman Centre, Colney Lane, Norwich NR4 7UB, UK in the emergency department. European Journal of Tel: + 44 1603 286140; fax: + 44 1603 286077; e-mail: [email protected] c Emergency Medicine 00:000–000 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins. Received 7September2010Accepted 17 November 2010 Introduction and accurate diagnosis is therefore essential. A sudden Upper limb injuries are commonly seen in the emergency forced abduction of the thumb is typical [11], most com- department [1]: fractures of the upper limb comprise monly in the context of trauma or contact sports. Skiers are approximately half of all fractures seen [2]. Much emphasis especially prone to this injury when falling while holding a is made on the distal radius, elbow and shoulder: fractures ski pole with the injured hand, hence the term ‘Skier’s here are frequently seen and usually well managed. -

Fracture Dislocations of the Proximal Interphalangeal Joint
FRACTURE DISLOCATIONS OF THE PROXIMAL INTERPHALANGEAL JOINT BY RICHARD KANG, MD, AND PETER J. STERN, MD Fracture dislocations of the proximal interphalangeal joint may occur by several different mechanisms of injury and are of 3 basic fracture patterns: palmar lip fractures, dorsal lip fractures, and pilon fractures. Proper treatment of these injuries is predicated on maintenance of concentric reduction of the joint, restoration of joint stability, and institution of early motion. Anatomic reconstitution of the articular surface, though ideal, is less important. Many methods are available to treat these injuries. Understanding the fracture within the context of a stability-based classifi- cation system helps to guide in the selection of the most appropriate treatment. Copyright © 2002 by the American Society for Surgery of the Hand racture dislocations of the proximal interphalan- lanx: (1) palmar lip fractures, (2) dorsal lip fractures, geal joint are common injuries that, when inad- and (3) pilon fractures (Fig 1). These fracture patterns Fequately understood, can be confusing for the are the result of characteristic mechanisms of injury. physician to treat. Worse, inappropriate treatment can Pure hyperextension may cause an avulsion fracture lead to a dysfunctional joint secondary to persistent pain, from the base of the middle phalanx. More commonly, stiffness, and posttraumatic degenerative arthrosis. A however, PIPJ fracture dislocations occur as a result of thorough understanding of the biomechanics of the in- an axial load, the specific fracture pattern depending jured proximal interphalangeal joint, the principles of its on the amount of flexion of the PIPJ at the time of treatment, and the available treatment options is essen- axial loading. -
Text Preview
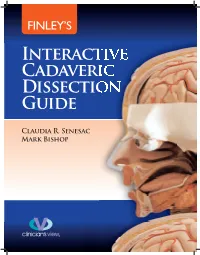
ix Introduction ANATOMY . IS THE VESTIBULE OF THE TEMPLE OF MEDICAL SCIENCE. —DE LINT, 19261 The ability to perform dissection provides a unique opportunity to observe the intricate in- terplay of human structure. This is especially true if the student is able to participate in an anatomy laboratory in which several (or many) different cadavers are located. A consistent theme in the treatises of early anatomists is awe and wonder at the incredible complexity and variety of the human organism. This unique and special opportunity was not always available to aspiring students. Imagine the difficulty of performing studious dissection before the development of effective embalm- ing or refrigeration, for example. Anatomists traveled from town to town to study from “fresh” bodies that had not yet begun to decay. To compound matters, dissection of human bodies sometimes happened in secret, in closed rooms and furtively at night. For more than 4000 years, we have sought to determine the structure and function of the human body. Chinese writings and drawings from about 2500 BCE describe circulation, breathing, and many internal organs.2 Around 1600 BCE, Egyptians recorded that the blood vessels were known to come from the heart, and these early anatomists recognized the liver, spleen, kidneys, uterus, and bladder.2 Hindu medicine dating from 600 BCE contains refer- ences to the skeleton and advanced surgical procedures.2 In the third and fourth centuries BCE, Hippocrates, Aristotle, and their followers compiled observations about the musculoskeletal system and organs. Most of these were made by com- bining external observation with conjecture based on the dissection of nonhuman animals.2 Herophilus and Erasistratus, working as surgeons in Alexandria in approximately 300 BCE, made systematic studies designed to discover the workings of human anatomy.2 However, the most influential anatomist of ancient times was, perhaps, Galen. -

Distal Radius Fractures
17 Distal Radius Fractures Scott W. Wolfe With the wide array of treatment options now available, this is an exciting era for the treatment of fractures of the distal radius. An improved understanding of kinematics, bone quality, and muscle forces acting across the fracture has led to increased awareness of a fracture’s relative stability, as well as the development of innovative devices to counteract these forces and restore stability. Innovations have occurred in closed treatment, percutaneous fixation, external fixation, and in particular, implants for internal fixation. However, new devices and techniques require careful assessment of efficacy, risk, and benefit as they are applied in practice, especially since the incidence of this fracture is likely to rise in an aging population. At this time, there are few published studies that definitively demonstrate the superiority of one technique or implant over another, as long as the anatomy of the distal radius is restored. Distal radius fractures are the most common fractures seen in the emergency department; they represent approximately 3% of all upper extremity injuries, with an incidence of greater than 640,000 annually in the United States alone.20 There is a bimodal distribution of these injuries, with a peak in the 5- to 24-year-old, predominantly male population who sustain athletic and high-energy injuries and a second peak in the elderly, predominantly female population characterized by lower-energy or “fragility” fractures. U.S. census data indicate that the percentage of persons aged 65 and older in the United States will rise from 12% to 19% over the next quarter century. -

Injuries to the Ulnar Collateral Ligament of the Thumb Metacarpophalangeal Joint
Ballard Office 5350 Tallman Ave NW, Suite 500 Seattle, WA 98107 www.seattlehandandelbow.com Wallingford Office 2409 45th Street, Seattle, WA 98103 Injuries to the Ulnar Collateral Ligament of the Thumb Metacarpophalangeal Joint Philip Heyma n, MD Abstract ment, the palmar plate, and, to a limited extent, the dorsal capsule. Injuries to the ulnar collateral ligament of the metacarpophalangeal (MCP) Biomechanical and clinical studies joint of the thumb are relatively common. When an incomplete rupture is pres- have shown that each of these ent, valgus stress testing with the MCP joint positioned in extension reveals structures contributes to joint sta- minimal or no instability (less than 30 degrees of laxity or less than 15 degrees bility and that their contribution is more laxity than in the noninjured thumb). When a complete rupture is pres- dependent on the position of the ent, valgus stress testing with the MCP joint positioned in extension reveals MCP joint.2,3 In flexion, the taut marked laxity (more than 30 degrees or more than 15 degrees more laxity than proper collateral ligament, which in the noninjured thumb). In this instance, displacement of the ligament proxi- runs from the middle of the mal and superficial to the adductor aponeurosis, which is often termed a Stener metacarpal head to the palmar lesion, is likely. Partial ligament injuries in which the ligament is not displaced aspect of the proximal phalanx, is may be treated nonoperatively. When a Stener lesion is present, however, pri- the primary joint stabilizer (Fig. 1). mary ligament healing cannot occur without operative management. Whether Because of this configuration, it treatment should be operative or nonperative can generally be decided on the also prevents palmar subluxation basis of the findings from the history, the radiographs, and the physical exami- of the proximal phalanx.