Distal Radius Fractures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transolecranon Distal Humerus Fractures: a Mini Review
Patel SS, Gatta J, Lee A, Bafus BT. Transolecranon Distal Humerus Fractures: A Mini Review. J Orthopedics & Orthopedic Surg. 2021;2(1):7-12 Mini Review Open Access Transolecranon Distal Humerus Fractures: A Mini Review Shaan S. Patel*, Julian Gatta, Adrienne Lee, Blaine T. Bafus Department of Orthopaedic Surgery, MetroHealth Medical Center, Cleveland, OH, USA Article Info Abstract Article Notes Background: Transolecranon distal humerus fractures are uncommon Received: March 13, 2021 injuries. The purpose of this study is to review the outcomes and complications Accepted: April 22, 2021 associated with transolecranon distal humerus fractures. *Correspondence: Material and Methods: We performed a systematic search of PubMed *Dr. Shaan S. Patel, Department of Orthopaedic Surgery, for articles published between 1990 and 2021. Included studies reported MetroHealth Medical Center, Cleveland, OH, USA; Telephone No: (205) 495-0460; Email: [email protected]. outcomes and complications of transolecranon distal humerus fractures. Data was extracted from the included studies to describe patient demographics, ©2021 Patel SS. This article is distributed under the terms of the injury characteristics, outcome measurements, and complications. Creative Commons Attribution 4.0 International License. Results: A total of 4 studies met inclusion criteria for data extraction and Keywords analysis. Two studies evaluated an adult cohort of a total of 18 patients. The Transolecranon average Disabilities of the Arm, Shoulder, and Hand (DASH) score was 40 (range Olecranon 4.2 – 76.5). Fifteen patients (83%) had a complication. Elbow stiffness (11/18, Distal humerus 61%) was the most common complication. Eleven patients (61%) underwent Fracture Outcomes more than one procedure. Two studies evaluated a pediatric cohort of a total Complications of 9 patients. -
Isolated Avulsion Fracture of the Lesser Tuberosity of The
(aspects of trauma) Isolated Avulsion Fracture of the Lesser Tuberosity of the Humerus in an Adult: Case Report and Literature Review Aman Dhawan, MD, Kevin Kirk, DO, Thomas Dowd, MD, and William Doukas, MD solated avulsion fractures of also describe our operative technique, comminuted 3-cm lesser tuberosity the lesser tuberosity of the including use of heavy, nonabsorb- fracture fragment retracted approxi- proximal humerus are rare. able suture. mately 2 cm from the donor site We report the case of a right- (Figures 1B–1D). No biceps tendon Ihand–dominant woman in her early ASE EPORT subluxation or injury and no intra- C R 30s who sustained such an injury, A right-hand–dominant woman in articular pathology were noted. with an intact subscapularis tendon her early 30s presented with right The lesser tuberosity fracture was attached to the lesser tuberosity frag- shoulder pain 1 day after a fall down surgically repaired less than 2 weeks ment. Treatment included surgery to a flight of stairs. During the acci- after injury. Through a deltopectoral restore tension to the subscapularis dent, as her feet slipped out from approach, the rotator interval and muscle and maintain the force couple underneath her and her torso fell the 3×2-cm fracture fragment were about the shoulder joint. One year after injury, the patient reported no pain, excellent range of motion, and “[To be diagnosed] this injury...requires... return to activities. This case demonstrates the diag- careful review of orthogonal radiographs nostic challenge of this injury, which requires a high index of suspicion and and advanced imaging.” careful review of orthogonal radio- graphs and advanced imaging. -

Do Fluoroscopic and Radiographic Images Underestimate Pin Protrusion in Paediatric Supracondylar Humerus and Distal Radius Fractures? a Synthetic Bone Model Analysis
Original Clinical Article Do fluoroscopic and radiographic images underestimate pin protrusion in paediatric supracondylar humerus and distal radius fractures? A synthetic bone model analysis S. Kenney Orthopaedic surgeons using fluoroscopy should be aware of J. Schlechter this discrepancy when assessing intraoperative fluoroscopic images to decide on acceptable implant position. Level of Evidence: Level V Abstract Purpose Fluoroscopy is commonly used to confirm accept- Cite this article: Kenney S, Schlechter J. Do fluoroscopic and able position of percutaneously placed pins when treating radiographic images underestimate pin protrusion in pae- paediatric fractures. There is a paucity of literature investigat- diatric supracondylar humerus and distal radius fractures? ing the accuracy of fluoroscopic imaging when determining A synthetic bone model analysis. J Child Orthop 2019;13. DOI: pin position relative to the far cortex of the fixated bone. The 10.1302/1863-2548.13.180173 purpose of this study was to evaluate the accuracy of fluor- oscopic and radiographic imaging in measuring smooth pin Keywords: supracondylar humerus fracture; percutaneous protrusion from the far cortex of a bone model. pinning; fluoroscopic imaging; distal radius fracture; paediatrics Methods Eight bone models were implanted with smooth pins and anteroposterior fluoroscopic and radiographic stud- ies were obtained. All images were evaluated by orthopaedic Introduction attending physicians, residents and medical students. The Paediatric supracondylar humerus and distal radius frac- length of pin protrusion from the model surface was estimat- tures are common injuries making up 17% and 23% of ed on fluoroscopic imaging and measured on radiographs and all paediatric fractures, respectively.1 When these fractures compared with actual lengths measured on the bone models. -
Distal Radius System 2.5
PRODUCT INFORMATION Distal Radius System 2.5 APTUS® Wrist 2 | Distal Radius System 2.5 Contents 3 A New Generation of Radius Plates 4 One System for Primary and Secondary Reconstruction 6 ADAPTIVE II Distal Radius Plates 8 FPL Plates 10 Hook Plates 11 Lunate Facet Plates 12 Rim Plates 13 Fracture Plates 14 Correction Plates 15 Volar Frame Plates 16 Extra-Articular Plates 17 Small Fragment Plates 18 Dorsal Frame Plates 19 XL Plates 20 Distal Ulna Plates 21 Fracture Treatment Concept 22 Technology, Biomechanics, Screw Features 24 Precisely Guided Screw Placement 25 Instrument for Reconstruction of the Volar Tilt 26 Storage 27 Overview Screw Trajectories 29 Ordering Information 47 Bibliography For further information regarding the APTUS product line visit: www.medartis.com Medartis, APTUS, MODUS, TriLock, HexaDrive and SpeedTip are registered trademarks of Medartis AG / Medartis Holding AG, 4057 Basel, Switzerland www.medartis.com Distal Radius System 2.5 | 3 A New Generation of Radius Plates Why is a new generation of radius plates needed? Distal radius fractures are the most common fractures of the stable plate systems have enabled open reduction and inter- upper extremities. The knowledge of these fractures has grown nal fixation to become an established treatment method for enormously over the last years. Treatment concepts have like- intra- and extra-articular distal radius fractures. These sys- wise been refined. It is now generally accepted that the best tems have enabled even severe extension fractures with dor- possible anatomical reconstruction of the radiocarpal joint sal defect zones to be precisely repositioned and treated with (RCJ) and distal radioulnar joint (DRUJ) to produce a func- osteosynthesis via volar access without the need for additional tional outcome is a requirement. -

Ultrasound-Assisted Closed Reduction of Distal Radius Fractures
SCIENTIFIC ARTICLE Ultrasound-Assisted Closed Reduction of Distal Radius Fractures Narihito Kodama, MD, PhD, Yoshinori Takemura, MD, PhD, Hiroaki Ueba, MD, Shinji Imai, MD, PhD, Yoshitaka Matsusue, MD, PhD Purpose To assess the accuracy and ability of ultrasound for monitoring closed reduction for distal radius fractures. Methods Consecutive patients undergoing ultrasound-guided closed reduction of acute, dis- placed distal radius fractures between January 2003 and December 2006 at our department were enrolled. The control group was extracted from patients who underwent a closed reduction for similar fractures under fluoroscopy or without any imaging assistance. To confirm the accuracy of the ultrasonography measurements, displacement distance values were compared with those on radiographic imaging before and after reduction. X-ray pa- rameters for pre- and postreduction, reduction time, total cost, and success rate were compared between the ultrasound-guided and the control groups. Results The ultrasound-guided group consisted of 43 patients (mean age, 68 y) and the control group consisted of 57 patients, which included 35 patients (mean age, 74 y) with fluoroscopic reduction and of 22 patients (mean age, 72 y) with reduction unaided by imaging. There were no significant displacement differences between radiographic and ultrasound measurements. In x-ray parameters for pre- and postreduction, there were no significant differences between the 2 groups. Ultrasound-guided reduction took longer than the other 2 methods. The success rate of the ultrasound and the fluoroscopic groups were similar (95% and 94%, respectively). Conclusions Our data suggest that ultrasound assistance can aid reduction of distal radius fractures as well as fluoroscopy. (J Hand Surg Am. -

Downloads As of 6/2011.) 2
CURRICULUM VITAE Michael J. Prayson, MD Department of Orthopaedic Surgery, Sports Medicine & Rehabilitation Wright State University Boonshoft School of Medicine 30 E. Apple Street, Suite 2200 Dayton, Ohio 45409 937-208-2128 937-208-2920 Fax EDUCATION Institution Concentration Degree/Date Kent State University & Combined 6-Year Program BS/MD 1989 Northeastern Ohio Universities College of Medicine Rootstown, Ohio POST GRADUATE EDUCATION Item Date Orthopaedic Surgery Internship & Residency Training 1989-1994 Akron General Medical Center, Akron, Ohio Orthopaedic Traumatology Fellowship 1994-1995 Department of Orthopaedic Surgery University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania ACADEMIC EXPERIENCE Institution Position Date Northeastern Ohio Universities College of Medicine Clinical Instructor 1993-1994 Rootstown, Ohio University of Missouri Assistant Professor 1995-1998 Department of Orthopaedic Surgery Kansas City, Missouri Akron General Medical Center Assistant Professor 1998-1999 Department of Orthopaedic Surgery Akron, Ohio University of Pittsburgh Medical Center Assistant Professor 1999-2004 Department of Orthopaedic Surgery Pittsburgh, Pennsylvania Wright State University Boonshoft School of Medicine Associate Professor 2004-2009 Department of Orthopaedic Surgery, Director of Orthopaedic Sports Medicine & Rehabilitation Undergraduate Education 2004-2006 Dayton, Ohio Trauma Fellowship Director 2006-Present Director of Orthopaedic Trauma 2004-Present Section Chair of Orthopaedic Trauma 2008-2010 Vice Chairman 2008-Present -

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

Bone Mineral Density and Prevalence of Osteoporosis in Postmenopausal Korean Women with Low-Energy Distal Radius Fractures
ORIGINAL ARTICLE Musculoskeletal Disorders http://dx.doi.org/10.3346/jkms.2016.31.6.972 • J Korean Med Sci 2016; 31: 972-975 Bone Mineral Density and Prevalence of Osteoporosis in Postmenopausal Korean Women with Low-Energy Distal Radius Fractures Hong Jun Jung,1 Ho Youn Park,2 The aim of this study was to evaluate the bone mineral density and the prevalence of Jin Sam Kim,1 Jun-O Yoon,1 osteoporosis in postmenopausal Korean women with low-energy distal radius fractures and and In-Ho Jeon1 compared with those of aged-matched normal Korean women. Two hundred and six patients with distal radius fractures between March 2006 and March 2010 were included in 1Department of Orthopaedic Surgery, Asan Medical Center, School of Medicine, University of Ulsan, this study. Patients were divided into three groups by age; group 1 (50-59 years), group 2 Seoul, Korea; 2Department of Orthopedic Surgery, (60-69 years), and group 3 (70-79 years). Controls were age-matched normal Korean Uijeongbu St. Mary’s Hospital, The Catholic women. The bone mineral density values at all measured sites, except for the spine, were University of Korea, Uijeongbu, Korea significantly lower in group 1 than those of control. While the bone mineral density values Received: 3 July 2015 in groups 2 and 3 were lower than those of controls, these differences were not statistically Accepted: 16 March 2016 significant. All groups had significantly higher prevalence of osteoporosis at the Ward’s triangle; however, at the spine, femoral neck and trochanteric area it was not significantly Address for Correspondence: different from those of age-matched controls. -

CS-FFRA-05 – 2005-16 Super Duty Fabricated Radius Arms NOTE
Carli Suspension: 422 Jenks Circle, Corona, CA 92880 Tech Support: (714) 532-2798 CS-FFRA-05 – 2005-16 Super Duty Fabricated Radius Arms NOTE: Please review the product instructions prior to attempting installation to ensure installer is equipped with all tools and capabilities necessary to complete the product installation. We recommend thoroughly reading the instructions at least twice prior to attempting Installation. Before beginning disassembly of the vehicle, check the “What’s Included” section of the instructions to ensure you’ve received all parts necessary to complete installation. Further, verify that the parts received are PROPER TO YOUR application (year range, motor, etc.) to avoid potential down-time in correcting potential discrepancies. Any discrepancies will be handled by Carli Suspension and the correcting products will be shipped UPS Ground. LIFETIME PRODUCT WARRANTY Carli Suspension provides a limited lifetime product warranty against defects in workmanship and materials from date of purchase to the original purchaser for all products produced by Carli Suspension. Parts not manufactured by, but made to Carli Suspension’s specifications by third party manufacturers will carry a warranty through their respective manufacturer. (i.e. King Shocks, Bilstein Shocks, Fox Shocks). Deaver Leaf Spring’s warranty will be processed by Carli Suspension. Proof of purchase (from the original purchaser only) will be required to process any warranty claims. Carli Suspension products must be purchased for the listed Retail Price reflected by the price listed on the Carli Suspension Website at the time of purchase. Carli Suspension reserves the right to refuse warranty claims made by any customer refusing or unable to present proof of purchase, or presenting proof of purchase reflecting a price lower than Carli Suspension’s Retail Price at the time the item was purchased. -
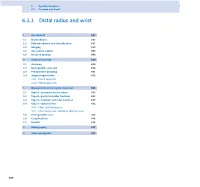
6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -

Sustentaculum Lunatum: Appreciation of the Palmar Lunate Facet in Management of Complex Intra-Articular Fractures of the Distal Radius
A Review Paper Sustentaculum Lunatum: Appreciation of the Palmar Lunate Facet in Management of Complex Intra-Articular Fractures of the Distal Radius Ebrahim Paryavi, MD, MPH, Matthew W. Christian, MD, W. Andrew Eglseder, MD, and Raymond A. Pensy, MD key role in restoring the anatomy of the palmar distal radial Abstract metaphysis during internal fixation. This fragment in com- Fracture of the distal radius is the most common wrist minuted fractures was first ascribed special importance by injury. Treatment of complex intra-articular fractures of Melone5 in his description of common fracture patterns. In the distal radius requires an accurate diagnosis of the the present article, we describe the anatomical characteristics fracture pattern and a thoughtful approach to fixation. of the sustentaculum lunatum and the clinical relevance of We propose a new term, sustentaculum lunatum, for this fragment to management of fractures of the distal radius. the palmar lunate facet. The sustentaculum lunatum deserves specific attention because of its importance Classification in load transmission across the radiocarpal joint. It is A variety of classification systems have been proposed to char- acterize and guide treatment of fractures of the distal radius. also key to restoring the anatomy of the palmarAJO distal The earliest descriptions of fracture patterns were presented by radial metaphysis during internal fixation. We provide Castaing6 and Frykman7 in the 1960s. The Frykman classifica- a review of the structure and function of the susten- tion historically has been popular but is limited in accuracy in taculum lunatum and describe fixation techniques. This its characterization of fragments and their displacement and is article is intended to promote awareness of this frag- limited in its ability to guide treatment. -

Broken Bones: Common Pediatric Lower Extremity Fractures—Part III
10173-06_ON2506-Hart.qxd 11/9/06 3:51 PM Page 390 Broken Bones: Common Pediatric Lower Extremity Fractures—Part III Erin S. Hart ▼ Brenda Luther ▼ Brian E. Grottkau Lower extremity injuries and fractures occur frequently in young usually have pain with hamstring stretching and hip flex- children and adolescents. Nurses are often one of the first ion/abduction). Patients also frequently demonstrate an healthcare providers to assess a child with an injury or fracture. antalgic gait and have pain during their activity or sport. Although basic fracture care and principles can be applied, An anteroposterior radiograph of the pelvis usually reveals nurses caring for these young patients must have a good under- the avulsed fragment. Comparative views of the contralat- standing of normal bone growth and development as well as eral side are often helpful in confirming the diagnosis and avoiding further unnecessary advanced imaging studies. common mechanisms of injury and fracture patterns seen in This injury is usually treated symptomatically and often children. Similar to many of the injuries in the upper extremity, involves rest, application of ice, and relaxation of the in- fractures in the lower extremity in children often can be treated volved tendon (O’Kane, 1999). Conservative treatment of nonoperatively with closed reduction and casting. However, this pelvic avulsion fractures is usually successful. Crutches are article will also review several lower extremity fractures that often needed for several weeks to reduce symptoms and frequently require surgical intervention to obtain a precise rest the extremity involved. Complications following pelvic anatomical reduction. Common mechanisms of injury, fracture avulsion fractures in children are rare, and most patients patterns, and current management techniques will be discussed.