Pediatric Orthopedic Injuries… … from an ED State of Mind
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transolecranon Distal Humerus Fractures: a Mini Review
Patel SS, Gatta J, Lee A, Bafus BT. Transolecranon Distal Humerus Fractures: A Mini Review. J Orthopedics & Orthopedic Surg. 2021;2(1):7-12 Mini Review Open Access Transolecranon Distal Humerus Fractures: A Mini Review Shaan S. Patel*, Julian Gatta, Adrienne Lee, Blaine T. Bafus Department of Orthopaedic Surgery, MetroHealth Medical Center, Cleveland, OH, USA Article Info Abstract Article Notes Background: Transolecranon distal humerus fractures are uncommon Received: March 13, 2021 injuries. The purpose of this study is to review the outcomes and complications Accepted: April 22, 2021 associated with transolecranon distal humerus fractures. *Correspondence: Material and Methods: We performed a systematic search of PubMed *Dr. Shaan S. Patel, Department of Orthopaedic Surgery, for articles published between 1990 and 2021. Included studies reported MetroHealth Medical Center, Cleveland, OH, USA; Telephone No: (205) 495-0460; Email: [email protected]. outcomes and complications of transolecranon distal humerus fractures. Data was extracted from the included studies to describe patient demographics, ©2021 Patel SS. This article is distributed under the terms of the injury characteristics, outcome measurements, and complications. Creative Commons Attribution 4.0 International License. Results: A total of 4 studies met inclusion criteria for data extraction and Keywords analysis. Two studies evaluated an adult cohort of a total of 18 patients. The Transolecranon average Disabilities of the Arm, Shoulder, and Hand (DASH) score was 40 (range Olecranon 4.2 – 76.5). Fifteen patients (83%) had a complication. Elbow stiffness (11/18, Distal humerus 61%) was the most common complication. Eleven patients (61%) underwent Fracture Outcomes more than one procedure. Two studies evaluated a pediatric cohort of a total Complications of 9 patients. -
Pediatric Trauma Imaging from Head To
High yield pediatric imaging Pediatric Trauma and other Pediatric Emergencies Lynn Ansley Fordham, MD, FACR, FAIUM, FAAWR UNC School of Medicine Department of Radiology Division Chief Pediatric Radiology Overview • Discuss epidemiology of pediatric trauma • Discuss unique aspects of skeletal trauma and fractures in children • Look at a few example of fractures • Review other common pediatric emergencies • Some Pollev Pollev.com\lynnfordham • Lots cases Keywords for PACs case review • PTF • TUBES AND LINES • Pre call cases peds Who to page for peds 2am Thursday morning? Faculty call shift 5pm to 8 am, for midnight to 8am, use prior day schedule Etiology of Skeletal Trauma in Children Significance of pediatric injuries • injuries 40% deaths in 1-4 year olds • injuries 90% deaths in 5-19 year olds Causes of Mortality in Childhood • MVA most common in all age groups • pedestrian (vs. auto 5-9) • bicycle • firearms • fires • drowning/ near drowning Causes of Morbidity in Childhood • falls – most common cause of injury in children • non-fatal MVAs • bicycle related trauma • trampolines • near drowning • other non-fatal injuries Trends over time • Decrease in death rates due to unintentional injuries – Carseats – Bicycle helmets • Increase in homicide rate • Increase in suicide rate MVA common injuries • depends on impact and seatbelt status • spine – craniocervical junction – thoracolumbar spine • pelvis • extremities • sternum rare in children Pediatric Fractures • Fractures related to the physis (growth plate) – Use Salter Harris classification -

Downloads As of 6/2011.) 2
CURRICULUM VITAE Michael J. Prayson, MD Department of Orthopaedic Surgery, Sports Medicine & Rehabilitation Wright State University Boonshoft School of Medicine 30 E. Apple Street, Suite 2200 Dayton, Ohio 45409 937-208-2128 937-208-2920 Fax EDUCATION Institution Concentration Degree/Date Kent State University & Combined 6-Year Program BS/MD 1989 Northeastern Ohio Universities College of Medicine Rootstown, Ohio POST GRADUATE EDUCATION Item Date Orthopaedic Surgery Internship & Residency Training 1989-1994 Akron General Medical Center, Akron, Ohio Orthopaedic Traumatology Fellowship 1994-1995 Department of Orthopaedic Surgery University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania ACADEMIC EXPERIENCE Institution Position Date Northeastern Ohio Universities College of Medicine Clinical Instructor 1993-1994 Rootstown, Ohio University of Missouri Assistant Professor 1995-1998 Department of Orthopaedic Surgery Kansas City, Missouri Akron General Medical Center Assistant Professor 1998-1999 Department of Orthopaedic Surgery Akron, Ohio University of Pittsburgh Medical Center Assistant Professor 1999-2004 Department of Orthopaedic Surgery Pittsburgh, Pennsylvania Wright State University Boonshoft School of Medicine Associate Professor 2004-2009 Department of Orthopaedic Surgery, Director of Orthopaedic Sports Medicine & Rehabilitation Undergraduate Education 2004-2006 Dayton, Ohio Trauma Fellowship Director 2006-Present Director of Orthopaedic Trauma 2004-Present Section Chair of Orthopaedic Trauma 2008-2010 Vice Chairman 2008-Present -

Greenstick Fracture Soft Cast No FU
Orthopaedic Department York Teaching Hospital This is a follow-up letter to your recent telephone consultation with the fracture care team explaining the ongoing management of your injury. Your case has been reviewed by an Orthopaedic Consultant (Bone Specialist) and Fracture Care Physiotherapist. You have sustained a greenstick fracture to your distal radius and/or ulna (forearm just before the wrist). This is a specific type of fracture that occurs in children’s bones Healing: This normally takes approximately 4 - 6 weeks to heal. It is normal for it to continue to ache a bit for a few weeks after this. Pain and swelling: Take pain killers as needed. The plaster backslab helps healing by keeping the bones in a good position. Elevate the arm to reduce swelling for the first few days Using your arm: You may use the arm as pain allows. It is important to keep the elbow moving to prevent stiffness. Follow up: There is a small chance that this fracture can displace (move). Therefore we routinely recommend a repeat x ray at 1 week after the injury and a new plaster cast. Arrangements for this appointment should have been made during your telephone consultation. Should you need to reschedule this appointment please see contact details at the top of this letter. Area of injury: If you are worried that you are unable to follow this rehabilitation plan, Or, if you are experiencing pain or symptoms, other than at the site of the original injury or surrounding area, or have any questions, then please phone the Fracture Care Team for advice. -

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

Case Report Tillaux Fracture in Adult
Case Report Syed et al: Tillaux fracture in adult Tillaux Fracture In Adult: A Case Report Syed T, Storey P, Rocha R, Kocheta A, Singhai S Study performed at Rotherham District General Hospital, Rotherham, South Yorkshire, United Kingdom Abstract Case report We report a rare case of Tillaux fracture of the ankle in a 36-year-old man. He sustained the injury in a football tackle and presented to us with pain and swelling of the left ankle. After preliminary X- rays, a CT scan was done which showed a Tillaux type fracture which is a rare injury after epiphyseal fusion. The ankle was treated with open reduction and internal fixation with screws and plaster for 6 weeks. At 3 months the patient had no pain in the ankle and able to mobilize full weight bearing on that side. Keywords : Ankle fracture, Tillaux fracture, Anterolateral tibial avulsion Address of correspondence: How to cite this article: Dr. Towheed Syed, Syed T, Storey P, Rocha R, Kocheta A, Singhai S. Tillaux Fracture 4-4-3-18/401, Senior heights, Street In Adult: A Case Report. Ortho J MPC. 2020;26(2): 95-98 no.3, Lalamma gardens, Puppalguda, Available from: Manikonda, Hyderabad - 500089 https://ojmpc.com/index.php/ojmpc/article/view/126 Email – [email protected] Introduction aim to educate the clinicians about this rare injury in adults, which is worthy of discussion. Tillaux fracture is an uncommon, rare ankle injury, described as an avulsion fracture of Case report anterolateral part of distal tibia due to the stronger pull of the anterior tibiofibular A 36-year-old gentleman presented to the ligament, by an external rotation force to the emergency department immediately after foot causing a Salter Harris type III injury [1- trauma sustained in a football tackle. -
PSI Appendix G Version 6.0 Patient Safety Indicators Appendices
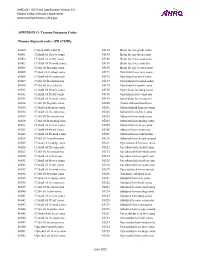
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX G: Trauma Diagnosis Codes Trauma diagnosis codes: (TRAUMID) 80000 Closed skull vault fx 85184 Brain lac nec-proln coma 80001 Cl skull vlt fx w/o coma 85185 Brain lac nec-deep coma 80002 Cl skull vlt fx-brf coma 85186 Brain lacer nec-coma nos 80003 Cl skull vlt fx-mod coma 85189 Brain lacer nec-concuss 80004 Cl skl vlt fx-proln coma 85190 Brain lac nec w open wnd 80005 Cl skul vlt fx-deep coma 85191 Opn brain lacer w/o coma 80006 Cl skull vlt fx-coma nos 85192 Opn brain lac-brief coma 80009 Cl skl vlt fx-concus nos 85193 Opn brain lacer-mod coma 80010 Cl skl vlt fx/cerebr lac 85194 Opn brain lac-proln coma 80011 Cl skull vlt fx w/o coma 85195 Open brain lac-deep coma 80012 Cl skull vlt fx-brf coma 85196 Opn brain lacer-coma nos 80013 Cl skull vlt fx-mod coma 85199 Open brain lacer-concuss 80014 Cl skl vlt fx-proln coma 85200 Traum subarachnoid hem 80015 Cl skul vlt fx-deep coma 85201 Subarachnoid hem-no coma 80016 Cl skull vlt fx-coma nos 85202 Subarach hem-brief coma 80019 Cl skl vlt fx-concus nos 85203 Subarach hem-mod coma 80020 Cl skl vlt fx/mening hem 85204 Subarach hem-prolng coma 80021 Cl skull vlt fx w/o coma 85205 Subarach hem-deep coma 80022 Cl skull vlt fx-brf coma 85206 Subarach hem-coma nos 80023 Cl skull vlt fx-mod coma 85209 Subarach hem-concussion 80024 Cl skl vlt fx-proln coma 85210 Subarach hem w opn wound 80025 Cl skul vlt fx-deep coma 85211 Opn subarach hem-no coma 80026 Cl skull vlt fx-coma nos 85212 -

Management of Pediatric Forearm Torus Fractures: a Systematic
ORIGINAL ARTICLE Management of Pediatric Forearm Torus Fractures A Systematic Review and Meta-Analysis Nan Jiang, MD,*† Zhen-hua Cao, MD,*‡ Yun-fei Ma, MD,*† Zhen Lin, MD,§ and Bin Yu, MD*† many disadvantages, such as heavy, bulky, and requires a second Objectives: Pediatric forearm torus fracture, a frequent reason for emer- visit to the hospital for removal. These flaws of cast may bring gency department visits, can be immobilized by both rigid cast and non- inconvenience to children as well as their families. In recent years, rigid methods. However, controversy still exists regarding the optimal many pediatric clinicians reported other methods to instead tradi- treatment of the disease. The aim of this study was to compare, in a system- tionally used cast, including soft cast,9,10 Futuro wrist splint,8,11 atic review, clinical efficacy of rigid cast with nonrigid methods for immo- and double Tubigrip.11 Although patients that suffered from fore- bilization of the pediatric forearm torus fractures. arm torus fractures can be immobilized by both rigid cast and non- Methods: Literature search was performed of PubMed and Cochrane Li- rigid materials, controversy still exists in the optimal treatment of brary by 2 independent reviewers to identify randomized controlled trials this fracture. comparing rigid cast with nonrigid methods for pediatric forearm torus The aim of this study was to, in a systematic review and fractures from inception to December 31, 2013, without limitation of publi- meta-analysis, compare clinical efficacy of recently used nonrigid cation language. Trial quality was assessed using the modified Jadad scale. immobilization methods with rigid cast. -

Vanderbilt Sports Medicine
Alabama AAP Fall Meeting Sept.19-20, 2009 Pediatric Fracture Care for the Pediatrician Andrew Gregory, MD, FAAP, FACSM Assistant Professor Orthopedics & Pediatrics Program Director, Sports Medicine Fellowship Vanderbilt University Vanderbilt Sports Medicine Disclosure No conflict of interest - unfortunately for me, I have no financial relationships with companies making products regarding this topic to disclose Objectives Review briefly the differences of pediatric bone Review Pediatric Fracture Classification Discuss subtle fractures in kids Discuss a few other pediatric only conditions 1 Pediatric Skeleton Bone is relatively elastic and rubbery Periosteum is quite thick & active Ligaments are strong relative to the bone Presence of the physis - “weak link” Ligament injuries & dislocations are rare – “kids don’t sprain stuff” Fractures heal quickly and have the capacity to remodel Anatomy of Pediatric Bone Epiphysis Physis Metaphysis Diaphysis Apophysis Pediatric Fracture Classification Plastic Deformation – Bowing usually of fibula or ulna Buckle/ Torus – compression, stable Greenstick – unicortical tension Complete – Spiral, Oblique, Transverse Physeal – Salter-Harris Apophyseal avulsion 2 Plastic deformation Bowing without fracture Often deformed requiring reduction Buckle (Torus) Fracture Buckled Periosteum – Metaphyseal/ diaphyseal junction Greenstick Fracture Cortex Broken on Only One Side – Incomplete 3 Complete Fractures Transverse – Perpendicular to the bone Oblique – Across the bone at 45-60 o – Unstable Spiral – Rotational -

SALTER HARRIS FRACTURES in CHILDREN
SALTER HARRIS FRACTURES in CHILDREN Kyra Frost 11/12/19 Diagnostic Radiology RAD 4001 Dr. Kumaravel Clinical History salter harris type 2 left tibia • 10 year old previously healthy boy comes into the Ed with a one day history of pain, swelling, and inability to move his left ankle after falling while playing tag. • Current Sx: • Pain and swelling around the ankle • Pain did not improve after taking Ibuprofen and putting ice on the • Physical exam findings: • Vital signs with in normal limits with the exception of mild tachycardia most likely related to pain: T: 99 HR: 110 RR: 15 BP: 118/78 Spo2: 100 % RA • Swelling at the left ankle joint and pain with passive ROM • Pt was unable to preform active ROM due to pain, and was unable to bear weight on affected left side. • Pt had 5+ strength in right lower extremity, DTR were 2+ throughout, and distal dorsalis pedis was 2+ bilaterally on exam • Work- Up • Xray of left, ankle, and foot • Xray of right, ankle, and foot for comparison McGovern Medical School Radiograph of left ankle • The average cost for an Xray of the Salter Harris foot is: type II Growth Plate 50-130$ Our patient was most likely billed 300-600 dollars Patient: 10/ 24/2019: Plain Radiographic Film in AP Plain Xray radiograph film in AP and Lateral view and Lateral views showing a minimally displaced of an 11 year old boy Salter Harris II Fracture of the distal tibia (of note – not original image due to formatting https://www.newchoicehealth.com/places/texas/houston/x- issues) ray McGovern Medical School Breaking it Down: Is -

University of Washington Orthopaedics & Sports Medicine
Discoveries 2018 University of Washington Orthopaedics & Sports Medicine University of Washington Department of Orthopaedics and Sports Medicine Discoveries 2018 Department of Orthopaedics and Sports Medicine University of Washington Seattle, WA 98195 EDITOR-IN-CHIEF: Howard A. Chansky, MD [email protected] ASSISTANT EDITORS: Christopher H. Allan, MD [email protected] Stephen A. Kennedy, MD, FRCSC [email protected] Adam A. Sassoon, MD, MS [email protected] MANAGING EDITOR: Fred Westerberg [email protected] Front Cover Illustration: Angie Kennedy, MSc, is a Seattle-based mixed media artist. She specializes in custom collage pieces that use mementos and artifacts to celebrate people and special life events. She drew on her experience as a former scientific researcher to create this collage of images from the pages of the current publication. The ‘W’ in the background is a nod to the University of Washington with an overlay of the current imagery arranged in an abstract assemblage. For more information www.americanheavyweight.com A pdf of this publication is available at our website: www.orthop.washington.edu. Permission Requests: All inquiries should be directed to the Managing Editor, University of Washington, Department of Orthopaedics and Sports Medicine, 1959 NE Pacific Street, Box 356500, Seattle, WA 98195-6500, or at the email address above. Contents 1 Foreword 2 From The Assistant Editors: The Modern Art of Musculoskeletal Research, Education, and Clinical Care 3 2018 Distinguished Alumnus, David J. Belfie, MD 4 New Faculty 6 Department of Orthopaedics and Sports Medicine Faculty 12 Visiting Lecturers Validation of a Rabbit Model of Trauma-Induced 14 Brandon J. Ausk, PhD, Philippe Huber, BS, Heterotopic Ossification Ted S. -

Pediatric Ankle Fractures
CHAPTER 26 PEDIATRIC ANKLE FRACTURES Sofi e Pinney, DPM, MS INTRODUCTION stronger than both the physis and bone. As a result, there is a greater capacity for plastic deformation and less chance of The purpose of this review is to examine the current intra-articular fractures, joint dislocation, and ligamentous literature on pediatric ankle fractures. I will discuss the disruptions. However, ligamentous injury may be more anatomic considerations of a pediatric patient, how to common than originally believed (1). A case-control study evaluate and manage these fractures, and when to surgically by Zonfrillo et al found an association between an increased repair them. Surgical techniques and complications will be risk of athletic injury in obese children, and concluded a briefl y reviewed. higher body mass index risk factor for ankle sprains (4). Ankle fractures are the third most common fractures in Secondary ossifi cation centers are located in the children, after the fi nger and distal radial physeal fracture. epiphysis. The distal tibial ossifi cation center appears at 6-24 Approximately 20-30% of all pediatric fractures are ankle months of age and closes asymmetrically over an 18-month fractures. Most ankle fractures occur at 8-15 years old. The period fi rst central, then medial and posterior, with the peak injury age is 11-12 years, and is relatively uncommon anterolateral portion closing last at 15 and 17 years of age for under the age 5. This injury is more common in boys. females and males, respectively. The distal fi bula ossifi cation The most common cause of pediatric ankle fractures is a center appears at 9-24 months of age and closes 1-2 years rotational force, and is often seen in sports injuries associated after the distal tibial.