Vanderbilt Sports Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Greenstick Fracture Soft Cast No FU
Orthopaedic Department York Teaching Hospital This is a follow-up letter to your recent telephone consultation with the fracture care team explaining the ongoing management of your injury. Your case has been reviewed by an Orthopaedic Consultant (Bone Specialist) and Fracture Care Physiotherapist. You have sustained a greenstick fracture to your distal radius and/or ulna (forearm just before the wrist). This is a specific type of fracture that occurs in children’s bones Healing: This normally takes approximately 4 - 6 weeks to heal. It is normal for it to continue to ache a bit for a few weeks after this. Pain and swelling: Take pain killers as needed. The plaster backslab helps healing by keeping the bones in a good position. Elevate the arm to reduce swelling for the first few days Using your arm: You may use the arm as pain allows. It is important to keep the elbow moving to prevent stiffness. Follow up: There is a small chance that this fracture can displace (move). Therefore we routinely recommend a repeat x ray at 1 week after the injury and a new plaster cast. Arrangements for this appointment should have been made during your telephone consultation. Should you need to reschedule this appointment please see contact details at the top of this letter. Area of injury: If you are worried that you are unable to follow this rehabilitation plan, Or, if you are experiencing pain or symptoms, other than at the site of the original injury or surrounding area, or have any questions, then please phone the Fracture Care Team for advice. -
PSI Appendix G Version 6.0 Patient Safety Indicators Appendices
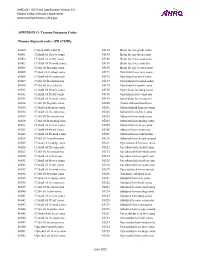
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX G: Trauma Diagnosis Codes Trauma diagnosis codes: (TRAUMID) 80000 Closed skull vault fx 85184 Brain lac nec-proln coma 80001 Cl skull vlt fx w/o coma 85185 Brain lac nec-deep coma 80002 Cl skull vlt fx-brf coma 85186 Brain lacer nec-coma nos 80003 Cl skull vlt fx-mod coma 85189 Brain lacer nec-concuss 80004 Cl skl vlt fx-proln coma 85190 Brain lac nec w open wnd 80005 Cl skul vlt fx-deep coma 85191 Opn brain lacer w/o coma 80006 Cl skull vlt fx-coma nos 85192 Opn brain lac-brief coma 80009 Cl skl vlt fx-concus nos 85193 Opn brain lacer-mod coma 80010 Cl skl vlt fx/cerebr lac 85194 Opn brain lac-proln coma 80011 Cl skull vlt fx w/o coma 85195 Open brain lac-deep coma 80012 Cl skull vlt fx-brf coma 85196 Opn brain lacer-coma nos 80013 Cl skull vlt fx-mod coma 85199 Open brain lacer-concuss 80014 Cl skl vlt fx-proln coma 85200 Traum subarachnoid hem 80015 Cl skul vlt fx-deep coma 85201 Subarachnoid hem-no coma 80016 Cl skull vlt fx-coma nos 85202 Subarach hem-brief coma 80019 Cl skl vlt fx-concus nos 85203 Subarach hem-mod coma 80020 Cl skl vlt fx/mening hem 85204 Subarach hem-prolng coma 80021 Cl skull vlt fx w/o coma 85205 Subarach hem-deep coma 80022 Cl skull vlt fx-brf coma 85206 Subarach hem-coma nos 80023 Cl skull vlt fx-mod coma 85209 Subarach hem-concussion 80024 Cl skl vlt fx-proln coma 85210 Subarach hem w opn wound 80025 Cl skul vlt fx-deep coma 85211 Opn subarach hem-no coma 80026 Cl skull vlt fx-coma nos 85212 -

Management of Pediatric Forearm Torus Fractures: a Systematic
ORIGINAL ARTICLE Management of Pediatric Forearm Torus Fractures A Systematic Review and Meta-Analysis Nan Jiang, MD,*† Zhen-hua Cao, MD,*‡ Yun-fei Ma, MD,*† Zhen Lin, MD,§ and Bin Yu, MD*† many disadvantages, such as heavy, bulky, and requires a second Objectives: Pediatric forearm torus fracture, a frequent reason for emer- visit to the hospital for removal. These flaws of cast may bring gency department visits, can be immobilized by both rigid cast and non- inconvenience to children as well as their families. In recent years, rigid methods. However, controversy still exists regarding the optimal many pediatric clinicians reported other methods to instead tradi- treatment of the disease. The aim of this study was to compare, in a system- tionally used cast, including soft cast,9,10 Futuro wrist splint,8,11 atic review, clinical efficacy of rigid cast with nonrigid methods for immo- and double Tubigrip.11 Although patients that suffered from fore- bilization of the pediatric forearm torus fractures. arm torus fractures can be immobilized by both rigid cast and non- Methods: Literature search was performed of PubMed and Cochrane Li- rigid materials, controversy still exists in the optimal treatment of brary by 2 independent reviewers to identify randomized controlled trials this fracture. comparing rigid cast with nonrigid methods for pediatric forearm torus The aim of this study was to, in a systematic review and fractures from inception to December 31, 2013, without limitation of publi- meta-analysis, compare clinical efficacy of recently used nonrigid cation language. Trial quality was assessed using the modified Jadad scale. immobilization methods with rigid cast. -

Pediatric Orthopedic Injuries… … from an ED State of Mind
Traumatic Orthopedics Peds RC Exam Review February 28, 2019 Dr. Naminder Sandhu, FRCPC Pediatric Emergency Medicine Objectives to cover today • Normal bone growth and function • Common radiographic abnormalities in MSK diseases • Part 1: Atraumatic – Congenital abnormalities – Joint and limb pain – Joint deformities – MSK infections – Bone tumors – Common gait disorders • Part 2: Traumatic – Common pediatric fractures and soft tissue injuries by site Overview of traumatic MSK pain Acute injuries • Fractures • Joint dislocations – Most common in ED: patella, digits, shoulder, elbow • Muscle strains – Eg. groin/adductors • Ligament sprains – Eg. Ankle, ACL/MCL, acromioclavicular joint separation Chronic/ overuse injuries • Stress fractures • Tendonitis • Bursitis • Fasciitis • Apophysitis Overuse injuries in the athlete WHY do they happen?? Extrinsic factors: • Errors in training • Inappropriate footwear Overuse injuries Intrinsic: • Poor conditioning – increased injuries early in season • Muscle imbalances – Weak muscle near strong (vastus medialus vs lateralus patellofemoral pain) – Excessive tightness: IT band, gastroc/soleus Sever disease • Anatomic misalignments – eg. pes planus, genu valgum or varum • Growth – strength and flexibility imbalances • Nutrition – eg. female athlete triad Misalignment – an intrinsic factor Apophysitis • *Apophysis = natural protruberance from a bone (2ndary ossification centres, often where tendons attach) • Examples – Sever disease (Calcaneal) – Osgood Schlatter disease (Tibial tubercle) – Sinding-Larsen-Johansson -

Ankle Injuries
Pediatric Fractures of the Ankle Nicholas Frane DO Zucker/Hofstra School of Medicine Northwell Health Core Curriculum V5 Disclosure • Radiographic Images Courtesy of: Dr. Jon-Paul Dimauro M.D or Christopher D Souder, MD, unless otherwise specified Core Curriculum V5 Outline • Epidemiology • Anatomy • Classification • Assessment • Treatment • Outcomes Core Curriculum V5 Epidemiology • Distal tibial & fibular physeal injuries 25%-38% of all physeal fractures • Ankle is the 2nd most common site of physeal Injury in children • Most common mechanism of injury Sports • 58% of physeal ankle fractures occur during sports activities • M>F • Commonly seen in 8-15y/o Hynes D, O'Brien T. Growth disturbance lines after injury of the distal tibial physis. Their significance in prognosis. J Bone Joint Surg Br. 1988;70:231–233 Zaricznyj B, Shattuck LJ, Mast TA, et al. Sports-related injuries in school-aged children. Am J Sports Med. 1980;8:318–324. Core Curriculum V5 Epidemiology Parikh SN, Mehlman CT. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Ankle Fracture Pearls and Pitfalls. J Orthop Trauma. 2017;31 Suppl 6:S27-S31. doi:10.1097/BOT.0000000000001014 Spiegel P, et al. Epiphyseal fractures of the distal ends of the tibia and fibula. J Bone Joint Surg Am. 1978;60(8):1046-50. Core Curriculum V5 Anatomy • Ligamentous structures attach distal to the physis • Growth plate injury more likely than ligament failure secondary to tensile weakness in physis • Syndesmosis • Anterior Tibio-fibular ligament (AITFL) • Posterior Inferior Tibio-fibular -

Torus (Buckle) Fracture Discharge Advice
Torus (Buckle) Fracture Discharge Advice Information for you Follow us on Twitter @NHSaaa Find us on Facebook at www.facebook.com/nhsaaa Visit our website: www.nhsaaa.net All our publications are available in other formats What has happened? Your child has sustained a torus fracture, also known as a “buckle” fracture, of the radius and/or ulna (the long bones at the wrist). The bone “buckles” on one side rather than actually breaks and is commonly seen in children as their bones are soft and flexible. Will my child need a cast? Torus fractures heal well without any long-term complications. They do not require any operations or to be placed in a cast. However, using a wrist splint provides comfort and reduces the risk of further injury. It should be worn at all times but can be removed for washing and showering without any risk to the fracture. Simple painkillers such as paracetamol and/or ibuprofen can also be used to reduce discomfort. How long should my child wear the splint for? In general, the older the child is, the longer they will need to wear the splint. We recommend that children under five years old should wear the splint for one week, those age five to ten years should wear it for two weeks and those over ten years should wear it for three weeks. If your child removes the splint before this time but is comfortable and moving their wrist freely then there is no need to insist that they wear the splint for longer. However, if your child is still sore and reluctant to use their wrist when the splint is removed, then you 2 may reapply the splint. -

Musculoskeletal System Imaging
SUMPh “N. Testemitanu” Radiology and Medical imaging department MUSCULOSKELETAL SYSTEM IMAGING M. Crivceanschii, assistant professor GOALS AND OBJECTIVES • to be aware of the role of modern diagnostic imaging modalities • to be familiar with main radiological signs and syndromes • tips and tricks in musculoskeletal imaging IMAGING MODALITIES • that every student should now IMAGING MODALITIES • Conventional Radiography • Fluoroscopy • Arthrography • Computed Tomography • Magnetic Resonance Imaging • Ultrasound • Scintigraphy PLAIN X-RAY FILM • First line study for most medical issues • Excellent for fractures/bony detail • Very limited for soft tissues (ligaments, tendons, muscles) • Only a screening tool in the spine • The radiologist should obtain at least two (2) views of the bone involved at 90° angles to each other • with each view including two adjacent joints FLUOROSCOPY • Arthrography • Tenography • Arteriography • Percutaneous Bone or Soft Tissue Biopsy CT SCANNING • Excellent for bony structural anatomy in the setting of complicated fracture • Less effective than MR for soft tissues and active processes • High radiation Dose • Interventional options MRI SCANNING • Excellent for soft tissue pathology • Good-excellent for bone pathology • No ionizing radiation • NOT patient friendly • Some absolute and relative contraindications ULTRASOUND • Reproducible in trained hands • Excellent for superficial soft tissue elements including tendons and muscles • No ionizing radiation • Patient friendly SCINTIGRAPHY • Image the entire skeleton at once • It provides a metabolic picture • It is particularly helpful in condition such as fibrous dysplasia, Langerhans Cell Histocytosis or metastatic cancer. CONGENITAL SKELETAL ANOMALIES CONGENITAL SKELETAL ANOMALIES • Chromosomal disorders (e. g. Down’s syndrome, Marfan syndrome, Turner’s syndrome, etc.) • Dwarfism (rhizomelic – proximal segments shortening, mesomelic – middle segments, acromelic – distal segments) • Skeletal dysplasias (e. -

Basic Principles of Fracture Treatment in Children
Eklem Hastalıkları ve Eklem Hastalik Cerrahisi Cerrahisi 2018;29(1):52-57 Joint Diseases and Related Surgery Review / Derleme doi: 10.5606/ehc.2018.58165 Basic principles of fracture treatment in children Çocuklarda kırık tedavisinin temel prensipleri Hakan Ömeroğlu, MD1 Department of Orthopedics and Traumatology, TOBB University of Economics and Technology, Faculty of Medicine, Ankara, Turkey ABSTRACT ÖZ This review aims to summarize the basic treatment principles Bu derlemede çocuklarda tiplerine göre kırıkların temel of fractures according to their types and general management tedavi prensipleri ve fizis kırıkları, çoklu kırıklar, açık principles of special conditions including physeal fractures, kırıklar ve patolojik kırıkları içeren özel durumların genel multiple fractures, open fractures, and pathologic fractures yönetim prensipleri özetlendi. Yaralanma mekanizmasını in children. Definition of the fracture is needed for better daha iyi anlamak, uygun bir tedavi stratejisi belirlemek ve understanding the injury mechanism, planning a proper prognozu tahmin etmek için kırığın tanımlanması gereklidir. treatment strategy, and estimating the prognosis. As the İyileşme süreci daha az komplike, yeniden şekillenme healing process is less complicated, remodeling capacity is kapasitesi daha yüksek ve kaynamama seyrek olduğu için higher and non-union is rare, the fractures in children are çocuklarda kırıklar çoğunlukla cerrahi dışı yöntemlerle commonly treated by non-surgical methods. Surgical treatment tedavi edilir. Çoklu yaralanması olan -

Imaging of Pediatric Fracture
IMAGING OF PEDIATRIC FRACTURE ELYSANTI DWI MARTADIANI DEPARTMENT OF DIAGNOSTIC RADIOLOGY UDAYANA MEDICAL FACULTY / SANGLAH GENERAL HOSPITAL OVERVIEW Unique Features of Pediatric Skeleton Type of Pediatric Fractures Imaging Modality Take Home Points PEDIATRIC SKELETON Prevents propagation of More porous and fractures Comminuted elastic in early fractures << childhood Resist stress and Stronger ligaments torsional forces Fracture of and tendons than growth plate the physis << PEDIATRIC SKELETON Incomplete fractures Thick periosteum Better healing Puberty Increase in muscle strength Avulsion and rapid growth fracture OVERVIEW Unique Features of Pediatric Skeleton Type of Pediatric Fractures Imaging Modality Take Home Points INCOMPLETE FRACTURES • Plastic Deformity / Bowing Fracture • Buckle / Torus Fracture • Greenstick Fracture Plastic Deformity / Bowing Fracture • Angulation of the bone beyond its elastic limit, but the energy is insufficient to produce a fracture • No fracture line is visible radiographically • Unique to children • >> in the ulna, occasionally in the fibula. • Bend in the ulna of < 20° in a 4 year old child should correct with growth http://www.rch.org.au/fracture-education/biomechanics/Biomechanical_differences_between_adult_and_child/ PLASTIC DEFORMITY / BOWING FRACTURE https://www.med-ed.virginia.edu/courses/rad/ext/2elbow/ Buckle / Torus Fracture • Compression failure of bone that usually occurs at the junction of the metaphysis and the diaphysis • Commonly seen in distal radius. • Heal in 3-4 weeks with simple immobilization http://www.rch.org.au/fracture-education/biomechanics/Biomechanical_differences_between_adult_and_child/ TORUS / BUCKLE FRACTURE http://o.quizlet.com/ http://www.healio.com/~/media/Journals/PedAnn/2014/5/_ Greenstick Fracture • Bone is bent and the tensile/convex side of the bone fails. • Fracture line does not propagate to the concave side of the bone, therefore showing evidence of plastic deformation. -
Splinting Avian Fractures
SPLINTING AVIAN FRACTURES Rebecca Duerr D V M M PV M International Bird Rescue Research Center Cordelia, CA © 2004, 2010: 2nd Edition, Rebecca Duerr. All drawings and images are by the author unless otherwise marked. TABLE OF CONTENTS Section Page • Considerations for wild bird care 2 • Glossary of terms 2 • Physical examination 3 • Before beginning the splint 4 • Compound fractures 5 • Prognoses of typical fractures 6 • The avian skeleton 10 • Examining the wing for possible fractures 11 • Splinting fractures of the wing: Humerus or radius/ulna fractures with support 12 • Splinting fractures of the wing: Metacarpal fractures with support 14 • Metacarpal wrap 15 • Calcium supplementation for fractured birds 15 • Slit wing wrap 16 • Examining the leg for possible fractures 17 • Splinting the femur: To immobilize prior to surgery or as the only treatment 18 • Tibiotarsus: making the splint 20 • Tibiotarsus: applying the splint 21 • Splinting the tarsometatarsus 22 • Splinting the foot—applying a shoe 23 • Mallards: walking/swimming splint for tarsometatarsus fractures 25 1 Considerations for wild bird care Treating wild birds with fractures requires the consideration of a number of factors that are not issues in treating domestic pets. First and foremost, each bird must be fit to be released when healed; even with raptors, available placement for disabled birds is a rare thing. It is even difficult to place charismatic species such as eagles. Consequently, reality (and usually rehabilitation licensing) dictates that a bird with an injury that will render it unable to fly or forage should be humanely euthanized. It is both illegal and inhumane to keep most wild birds as pets. -

Classification of Fractures Factsheet Classification of Fractures Factsheet
Classification of fractures Factsheet Classification of fractures Factsheet Effectively assessing injuries and patients is vital to identify complications that may affect bone healing. This factsheet summarises the different types of fracture. Classifying fractures: Fractures are breaks in bones, whether across the entire bone or a greenstick fracture on one side of the bone. They are classified either descriptively or physiologically. Descriptive classification Physiological classification Clinical classification- patient examination, or X-ray The factors that made the bone susceptible to classification- the appearance of the bone and breaking in context and health. direction of the break. Types of fracture: Simple or Closed A fracture is classified as simple or closed when the surrounding soft tissue remains intact with no wounds. There may be soft tissue damage. The fracture may still cause injury to nerves, arteries, or tendons in the injury zone; therefore, neuro-vascular status should be assessed before and after cast application, which is a mandatory part of fracture assessment. Open Sometimes referred to as compound or complex, an open fracture is identified by a skin wound that may connect to the fracture site. The size of the skin wound does not indicate the extent of the fracture, muscle trauma or contamination. Any fracture with a skin wound should be assumed to be an open fracture to limit the risk of infection, which is hard to eradicate if it becomes established in the bone. Open fractures can be direct - where the object that breaks the skin continued and breaks the bone or indirect, where the bone is bent and breaks through the skin. -

Musculoskeletal Radiograph Interpretation – Specific Approach by Joint/Area
Musculoskeletal Radiograph Interpretation – Specific Approach by Joint/Area The generic approach to musculoskeletal radiograph interpretation is covered separately. This is sufficient for most single bone radiographs. However, radiographs of many joints/areas require a specific approach to interpretation or have specific signs which need to be looked for within the ABCS approach – these are outlined here. Facial bones Identify zygoma (stool) and look for fractures of its 4 legs: 1. Zygomatic arch – if you imagine the zygoma as an elephant’s head, this leg looks like an its trunk on a radiograph 2. Frontal process of zygoma 3. Orbital floor 4. Lateral wall of maxillary antrum Soft tissue signs indicating a fracture (working downwards) o Black eyebrow sign – black eyebrow like shadow across top of orbit (air in orbit 2 from sinus, usually due to orbital blow-out fracture) 1 3 o MAXILLARY 1 Teardrop sign – dark shadow at the top of the maxillary antrum (soft tissue ANTRUM herniation of orbital contents from orbital blow-out fracture) 4 o Fluid level – in maxillary antrum (blood from fracture) Common pathology Nasal bone fracture: commonly due to punch injury; may not be seen on radiographs and X-rays are not performed to specifically look for it as it does not change management; look up the patient’s nose to exclude a septal haematoma! Mandible fracture: commonly due to punch injury; use an OPG X-ray to look for it, not a facial bone X-ray Zygomatic arch fracture Orbital floor fracture ‘Tripod’ fracture: fractures of all 4 ‘legs’ of the zygoma due to major trauma – should really be called a quadripod fracture Cervical spine Lateral view (ABCS)… Adequacy: Need to see skull base and C7/T1 disc space (if not, get swimmer’s view) Alignment Alignment arcs (look for smooth curves) 1.