Basic Principles in the Assessment and Treatment of Fractures in Skeletally Immature Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Systemic Therapy of Mscs in Bone Regeneration: a Systematic Review and Meta-Analysis Jingfei Fu, Yanxue Wang, Yiyang Jiang, Juan Du, Junji Xu* and Yi Liu*
Fu et al. Stem Cell Research & Therapy (2021) 12:377 https://doi.org/10.1186/s13287-021-02456-w REVIEW Open Access Systemic therapy of MSCs in bone regeneration: a systematic review and meta-analysis Jingfei Fu, Yanxue Wang, Yiyang Jiang, Juan Du, Junji Xu* and Yi Liu* Abstract Objectives: Over the past decades, many studies focused on mesenchymal stem cells (MSCs) therapy for bone regeneration. Due to the efficiency of topical application has been widely dicussed and systemic application was also a feasible way for new bone formation, the aim of this study was to systematically review systemic therapy of MSCs for bone regeneration in pre-clinical studies. Methods: The article search was conducted in PubMed and Embase databases. Original research articles that assessed potential effect of systemic application of MSCs for bone regeneration in vivo were selected and evaluated in this review, according to eligibility criteria. The efficacy of MSC systemic treatment was analyzed by random effects meta-analysis, and the outcomes were expressed in standard mean difference (SMD) and its 95% confidence interval. Subgroup analyses were conducted on animal species and gender, MSCs types, frequency and time of injection, and bone diseases. Results: Twenty-three articles were selected in this review, of which 21 were included in meta-analysis. The results showed that systemic therapy increased bone mineral density (SMD 3.02 [1.84, 4.20]), bone volume to tissue volume ratio (2.10 [1.16, 3.03]), and the percentage of new bone area (7.03 [2.10, 11.96]). Bone loss caused by systemic disease tended to produce a better response to systemic treatment (p=0.05 in BMD, p=0.03 in BV/TV). -

Greenstick Fracture Soft Cast No FU
Orthopaedic Department York Teaching Hospital This is a follow-up letter to your recent telephone consultation with the fracture care team explaining the ongoing management of your injury. Your case has been reviewed by an Orthopaedic Consultant (Bone Specialist) and Fracture Care Physiotherapist. You have sustained a greenstick fracture to your distal radius and/or ulna (forearm just before the wrist). This is a specific type of fracture that occurs in children’s bones Healing: This normally takes approximately 4 - 6 weeks to heal. It is normal for it to continue to ache a bit for a few weeks after this. Pain and swelling: Take pain killers as needed. The plaster backslab helps healing by keeping the bones in a good position. Elevate the arm to reduce swelling for the first few days Using your arm: You may use the arm as pain allows. It is important to keep the elbow moving to prevent stiffness. Follow up: There is a small chance that this fracture can displace (move). Therefore we routinely recommend a repeat x ray at 1 week after the injury and a new plaster cast. Arrangements for this appointment should have been made during your telephone consultation. Should you need to reschedule this appointment please see contact details at the top of this letter. Area of injury: If you are worried that you are unable to follow this rehabilitation plan, Or, if you are experiencing pain or symptoms, other than at the site of the original injury or surrounding area, or have any questions, then please phone the Fracture Care Team for advice. -

Effect of Freeze-Dried Bovine Bone Xenograft on Tumor Necrosis Factor- Alpha Secretion in Human Peripheral Blood Mononuclear Cells
Asian Jr. of Microbiol. Biotech. Env. Sc. Vol. 20 (December Suppl.) : 2018 : S88-S92 © Global Science Publications ISSN-0972-3005 EFFECT OF FREEZE-DRIED BOVINE BONE XENOGRAFT ON TUMOR NECROSIS FACTOR- ALPHA SECRETION IN HUMAN PERIPHERAL BLOOD MONONUCLEAR CELLS AHMAD K.M. HUMIDAT1, DAVID B. KAMADJAJA2,3*, CHRIST BIANTO1, ANINDITA Z. RASYIDA1, PURWATI3 AND ACHMAD HARIJADI2 1Residency Program, Department of Oral and Maxillofacial Surgery, Faculty of Dental Medicine, Universitas Airlangga, Surabaya, Indonesia. 2Department of Oral Maxillofacial Surgery, Faculty of Dental Medicine, Universitas Airlangga, Surabaya,Indonesia. 3Stem Cell Research and Development Center, Universitas Airlangga, Surabaya, Indonesia (Received 25 September, 2018; accepted 15 November, 2018) Key words: Tumor Necrosis Factor , Freeze Dried Bovine Bone Xenograft, Human peripheral blood mononuclear cell. Abstract– Alveolar bone augmentation requires the use of bone graft particles to promote bone formation. Freeze-dried bovine bone xenograft (FDBBX) is a type of bone substitute may be potential as an alternative to autogenous bone graft. However, since it is xenogeneic material, it may trigger body’s immune response and cause early resorption of the graft. Tumor Necrosis Factor- (TNF-) is a cytokine which is released rapidly after trauma or infection and is one of the most abundant mediators in inflammation tissue. The immune system and immune response play a very important role in the concept of bone healing. Human peripheral blood mononuclear cells (hPBMCs) is a critical component of the immune system which release TNF-. This study aims to evaluate FDBBX effect on the secretion of TNF-á in hPBMCs culture. hPBMC cultures were divided into two groups. In experimental groups, the cell was cultured in FDBX conditioned medium of 2.5% dilution while in control group, basic medium was used. -

Interactions Between Bone and Immune Systems: a Focus on the Role of Inflammation in Bone Resorption and Fracture Healing
PERIODICUM BIOLOGORUM UDC 57:61 VOL. 116, No 1, 45–52, 2014 CODEN PDBIAD ISSN 0031-5362 Interactions between bone and immune systems: A focus on the role of inflammation in bone resorption and fracture healing Abstract TOMISLAV KELAVA1,2 ALAN ŠUĆUR1,2 Functional interactions between the immune system and bone tissues are SANIA KUZMAC2,3 reflected in a number of cytokines, chemokines, hormones and other media- 2,3 VEDRAN KATAVIĆ tors regulating the functions of both bone and immune cells. Investigations 1 Department of Physiology and Immunology of the mechanisms of those interactions have become important for the un- University of Zagreb School of Medicine derstanding of the pathogeneses of diseases like inflammatory arthritis, in- [alata 3b, Zagreb-HR 10000, Croatia flammatory bowel disease, periodontal disease and osteoporosis. This review 2 Laboratory for Molecular Immunology first addresses the roles of the inflammatory mediators and mechanisms by University of Zagreb School of Medicine which they cause inflammation-induced bone loss. In the second part of the [alata 12, Zagreb-HR 10000, Croatia review we stress the importance of proinflammatory mediators for normal 3 Department of Anatomy fracture healing. Defective bone remodeling underlying different patho- University of Zagreb School of Medicine logical processes may be caused by disturbed differentiation and function of [alata 3b, Zagreb-HR 10000, Croatia either osteoclast or osteoblast lineage cells. Understanding of the mechanisms governing enhanced differentiation and activation -
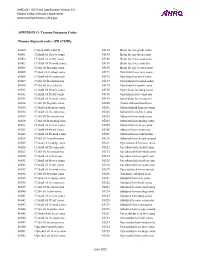
PSI Appendix G Version 6.0 Patient Safety Indicators Appendices
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX G: Trauma Diagnosis Codes Trauma diagnosis codes: (TRAUMID) 80000 Closed skull vault fx 85184 Brain lac nec-proln coma 80001 Cl skull vlt fx w/o coma 85185 Brain lac nec-deep coma 80002 Cl skull vlt fx-brf coma 85186 Brain lacer nec-coma nos 80003 Cl skull vlt fx-mod coma 85189 Brain lacer nec-concuss 80004 Cl skl vlt fx-proln coma 85190 Brain lac nec w open wnd 80005 Cl skul vlt fx-deep coma 85191 Opn brain lacer w/o coma 80006 Cl skull vlt fx-coma nos 85192 Opn brain lac-brief coma 80009 Cl skl vlt fx-concus nos 85193 Opn brain lacer-mod coma 80010 Cl skl vlt fx/cerebr lac 85194 Opn brain lac-proln coma 80011 Cl skull vlt fx w/o coma 85195 Open brain lac-deep coma 80012 Cl skull vlt fx-brf coma 85196 Opn brain lacer-coma nos 80013 Cl skull vlt fx-mod coma 85199 Open brain lacer-concuss 80014 Cl skl vlt fx-proln coma 85200 Traum subarachnoid hem 80015 Cl skul vlt fx-deep coma 85201 Subarachnoid hem-no coma 80016 Cl skull vlt fx-coma nos 85202 Subarach hem-brief coma 80019 Cl skl vlt fx-concus nos 85203 Subarach hem-mod coma 80020 Cl skl vlt fx/mening hem 85204 Subarach hem-prolng coma 80021 Cl skull vlt fx w/o coma 85205 Subarach hem-deep coma 80022 Cl skull vlt fx-brf coma 85206 Subarach hem-coma nos 80023 Cl skull vlt fx-mod coma 85209 Subarach hem-concussion 80024 Cl skl vlt fx-proln coma 85210 Subarach hem w opn wound 80025 Cl skul vlt fx-deep coma 85211 Opn subarach hem-no coma 80026 Cl skull vlt fx-coma nos 85212 -

Management of Pediatric Forearm Torus Fractures: a Systematic
ORIGINAL ARTICLE Management of Pediatric Forearm Torus Fractures A Systematic Review and Meta-Analysis Nan Jiang, MD,*† Zhen-hua Cao, MD,*‡ Yun-fei Ma, MD,*† Zhen Lin, MD,§ and Bin Yu, MD*† many disadvantages, such as heavy, bulky, and requires a second Objectives: Pediatric forearm torus fracture, a frequent reason for emer- visit to the hospital for removal. These flaws of cast may bring gency department visits, can be immobilized by both rigid cast and non- inconvenience to children as well as their families. In recent years, rigid methods. However, controversy still exists regarding the optimal many pediatric clinicians reported other methods to instead tradi- treatment of the disease. The aim of this study was to compare, in a system- tionally used cast, including soft cast,9,10 Futuro wrist splint,8,11 atic review, clinical efficacy of rigid cast with nonrigid methods for immo- and double Tubigrip.11 Although patients that suffered from fore- bilization of the pediatric forearm torus fractures. arm torus fractures can be immobilized by both rigid cast and non- Methods: Literature search was performed of PubMed and Cochrane Li- rigid materials, controversy still exists in the optimal treatment of brary by 2 independent reviewers to identify randomized controlled trials this fracture. comparing rigid cast with nonrigid methods for pediatric forearm torus The aim of this study was to, in a systematic review and fractures from inception to December 31, 2013, without limitation of publi- meta-analysis, compare clinical efficacy of recently used nonrigid cation language. Trial quality was assessed using the modified Jadad scale. immobilization methods with rigid cast. -

Vanderbilt Sports Medicine
Alabama AAP Fall Meeting Sept.19-20, 2009 Pediatric Fracture Care for the Pediatrician Andrew Gregory, MD, FAAP, FACSM Assistant Professor Orthopedics & Pediatrics Program Director, Sports Medicine Fellowship Vanderbilt University Vanderbilt Sports Medicine Disclosure No conflict of interest - unfortunately for me, I have no financial relationships with companies making products regarding this topic to disclose Objectives Review briefly the differences of pediatric bone Review Pediatric Fracture Classification Discuss subtle fractures in kids Discuss a few other pediatric only conditions 1 Pediatric Skeleton Bone is relatively elastic and rubbery Periosteum is quite thick & active Ligaments are strong relative to the bone Presence of the physis - “weak link” Ligament injuries & dislocations are rare – “kids don’t sprain stuff” Fractures heal quickly and have the capacity to remodel Anatomy of Pediatric Bone Epiphysis Physis Metaphysis Diaphysis Apophysis Pediatric Fracture Classification Plastic Deformation – Bowing usually of fibula or ulna Buckle/ Torus – compression, stable Greenstick – unicortical tension Complete – Spiral, Oblique, Transverse Physeal – Salter-Harris Apophyseal avulsion 2 Plastic deformation Bowing without fracture Often deformed requiring reduction Buckle (Torus) Fracture Buckled Periosteum – Metaphyseal/ diaphyseal junction Greenstick Fracture Cortex Broken on Only One Side – Incomplete 3 Complete Fractures Transverse – Perpendicular to the bone Oblique – Across the bone at 45-60 o – Unstable Spiral – Rotational -

Pediatric Orthopedic Injuries… … from an ED State of Mind
Traumatic Orthopedics Peds RC Exam Review February 28, 2019 Dr. Naminder Sandhu, FRCPC Pediatric Emergency Medicine Objectives to cover today • Normal bone growth and function • Common radiographic abnormalities in MSK diseases • Part 1: Atraumatic – Congenital abnormalities – Joint and limb pain – Joint deformities – MSK infections – Bone tumors – Common gait disorders • Part 2: Traumatic – Common pediatric fractures and soft tissue injuries by site Overview of traumatic MSK pain Acute injuries • Fractures • Joint dislocations – Most common in ED: patella, digits, shoulder, elbow • Muscle strains – Eg. groin/adductors • Ligament sprains – Eg. Ankle, ACL/MCL, acromioclavicular joint separation Chronic/ overuse injuries • Stress fractures • Tendonitis • Bursitis • Fasciitis • Apophysitis Overuse injuries in the athlete WHY do they happen?? Extrinsic factors: • Errors in training • Inappropriate footwear Overuse injuries Intrinsic: • Poor conditioning – increased injuries early in season • Muscle imbalances – Weak muscle near strong (vastus medialus vs lateralus patellofemoral pain) – Excessive tightness: IT band, gastroc/soleus Sever disease • Anatomic misalignments – eg. pes planus, genu valgum or varum • Growth – strength and flexibility imbalances • Nutrition – eg. female athlete triad Misalignment – an intrinsic factor Apophysitis • *Apophysis = natural protruberance from a bone (2ndary ossification centres, often where tendons attach) • Examples – Sever disease (Calcaneal) – Osgood Schlatter disease (Tibial tubercle) – Sinding-Larsen-Johansson -

Bone Healing
BONE HEALING How Does a Bone Heal? Bone generally takes 6 to 8 weeks ll broken bones go through the to heal to a significant degree. In A same healing process. This general, children's bones heal faster is true whether a bone has been than those of adults. The foot and cut as part of a surgical procedure ankle surgeon will determine when or fractured through an injury. the patient is ready to bear weight The bone healing process Inflammation on the area. This will depend on the has three overlapping stages: location and severity of the fracture, inflammation, bone production, the type of surgical procedure and bone remodeling. performed, and other considerations. • Inflammation starts immediately after the bone is fractured and What Helps Promote lasts for several days. When Bone Healing? the bone is fractured there is If a bone will be cut during a bleeding into the area, leading planned surgical procedure, some to inflammation and clotting of steps can be taken pre-and post- blood at the fracture site. This operatively to help optimize healing. provides the initial structural Bone production The surgeon may offer advice on diet stability and framework for and nutritional supplements that are producing new bone. essential to bone growth. Smoking • Bone production begins when cessation, and adequate control the clotted blood formed by of blood sugar levels in diabetics, inflammation is replaced with are important. Smoking and high fibrous tissue and cartilage glucose levels interfere with bone (known as “soft callus”). As healing. healing progresses, the soft For all patients with fractured callus is replaced with hard bones, immobilization is a critical bone (known as “hard callus”), Bone remodeling part of treatment, because any which is visible on x-rays several movement of bone fragments slows weeks after the fracture. -

Biology of Bone Repair
Biology of Bone Repair J. Scott Broderick, MD Original Author: Timothy McHenry, MD; March 2004 New Author: J. Scott Broderick, MD; Revised November 2005 Types of Bone • Lamellar Bone – Collagen fibers arranged in parallel layers – Normal adult bone • Woven Bone (non-lamellar) – Randomly oriented collagen fibers – In adults, seen at sites of fracture healing, tendon or ligament attachment and in pathological conditions Lamellar Bone • Cortical bone – Comprised of osteons (Haversian systems) – Osteons communicate with medullary cavity by Volkmann’s canals Picture courtesy Gwen Childs, PhD. Haversian System osteocyte osteon Picture courtesy Gwen Childs, PhD. Haversian Volkmann’s canal canal Lamellar Bone • Cancellous bone (trabecular or spongy bone) – Bony struts (trabeculae) that are oriented in direction of the greatest stress Woven Bone • Coarse with random orientation • Weaker than lamellar bone • Normally remodeled to lamellar bone Figure from Rockwood and Green’s: Fractures in Adults, 4th ed Bone Composition • Cells – Osteocytes – Osteoblasts – Osteoclasts • Extracellular Matrix – Organic (35%) • Collagen (type I) 90% • Osteocalcin, osteonectin, proteoglycans, glycosaminoglycans, lipids (ground substance) – Inorganic (65%) • Primarily hydroxyapatite Ca5(PO4)3(OH)2 Osteoblasts • Derived from mesenchymal stem cells • Line the surface of the bone and produce osteoid • Immediate precursor is fibroblast-like Picture courtesy Gwen Childs, PhD. preosteoblasts Osteocytes • Osteoblasts surrounded by bone matrix – trapped in lacunae • Function -

Distal Radius Fracture
Distal Radius Fracture Osteoporosis, a common condition where bones become brittle, increases the risk of a wrist fracture if you fall. How are distal radius fractures diagnosed? Your provider will take a detailed health history and perform a physical evaluation. X-rays will be taken to confirm a fracture and help determine a treatment plan. Sometimes an MRI or CT scan is needed to get better detail of the fracture or to look for associated What is a distal radius fracture? injuries to soft tissues such as ligaments or Distal radius fracture is the medical term for tendons. a “broken wrist.” To fracture a bone means it is broken. A distal radius fracture occurs What is the treatment for distal when a sudden force causes the radius bone, radius fracture? located on the thumb side of the wrist, to break. The wrist joint includes many bones Treatment depends on the severity of your and joints. The most commonly broken bone fracture. Many factors influence treatment in the wrist is the radius bone. – whether the fracture is displaced or non-displaced, stable or unstable. Other Fractures may be closed or open considerations include age, overall health, (compound). An open fracture means a bone hand dominance, work and leisure activities, fragment has broken through the skin. There prior injuries, arthritis, and any other injuries is a risk of infection with an open fracture. associated with the fracture. Your provider will help determine the best treatment plan What causes a distal radius for your specific injury. fracture? Signs and Symptoms The most common cause of distal radius fracture is a fall onto an outstretched hand, • Swelling and/or bruising at the wrist from either slipping or tripping. -

Current and Future Concepts for the Treatment of Impaired Fracture Healing
International Journal of Molecular Sciences Review Current and Future Concepts for the Treatment of Impaired Fracture Healing Carsten W. Schlickewei y, Holger Kleinertz y, Darius M. Thiesen , Konrad Mader , Matthias Priemel, Karl-Heinz Frosch and Johannes Keller * Clinic of Trauma, Hand and Reconstructive Surgery, University Medical Center Hamburg-Eppendorf, 20246 Hamburg, Germany; [email protected] (C.W.S.); [email protected] (H.K.); [email protected] (D.M.T.); [email protected] (K.M.); [email protected] (M.P.); [email protected] (K.-H.F.) * Correspondence: [email protected]; Tel.: +49-1522-2817-439 These authors contributed equally to this work. y Received: 30 October 2019; Accepted: 15 November 2019; Published: 19 November 2019 Abstract: Bone regeneration represents a complex process, of which basic biologic principles have been evolutionarily conserved over a broad range of different species. Bone represents one of few tissues that can heal without forming a fibrous scar and, as such, resembles a unique form of tissue regeneration. Despite a tremendous improvement in surgical techniques in the past decades, impaired bone regeneration including non-unions still affect a significant number of patients with fractures. As impaired bone regeneration is associated with high socio-economic implications, it is an essential clinical need to gain a full understanding of the pathophysiology and identify novel treatment approaches. This review focuses on the clinical implications of impaired bone regeneration, including currently available treatment options. Moreover, recent advances in the understanding of fracture healing are discussed, which have resulted in the identification and development of novel therapeutic approaches for affected patients.