Musculoskeletal Radiograph Interpretation – Specific Approach by Joint/Area
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Do Fluoroscopic and Radiographic Images Underestimate Pin Protrusion in Paediatric Supracondylar Humerus and Distal Radius Fractures? a Synthetic Bone Model Analysis
Original Clinical Article Do fluoroscopic and radiographic images underestimate pin protrusion in paediatric supracondylar humerus and distal radius fractures? A synthetic bone model analysis S. Kenney Orthopaedic surgeons using fluoroscopy should be aware of J. Schlechter this discrepancy when assessing intraoperative fluoroscopic images to decide on acceptable implant position. Level of Evidence: Level V Abstract Purpose Fluoroscopy is commonly used to confirm accept- Cite this article: Kenney S, Schlechter J. Do fluoroscopic and able position of percutaneously placed pins when treating radiographic images underestimate pin protrusion in pae- paediatric fractures. There is a paucity of literature investigat- diatric supracondylar humerus and distal radius fractures? ing the accuracy of fluoroscopic imaging when determining A synthetic bone model analysis. J Child Orthop 2019;13. DOI: pin position relative to the far cortex of the fixated bone. The 10.1302/1863-2548.13.180173 purpose of this study was to evaluate the accuracy of fluor- oscopic and radiographic imaging in measuring smooth pin Keywords: supracondylar humerus fracture; percutaneous protrusion from the far cortex of a bone model. pinning; fluoroscopic imaging; distal radius fracture; paediatrics Methods Eight bone models were implanted with smooth pins and anteroposterior fluoroscopic and radiographic stud- ies were obtained. All images were evaluated by orthopaedic Introduction attending physicians, residents and medical students. The Paediatric supracondylar humerus and distal radius frac- length of pin protrusion from the model surface was estimat- tures are common injuries making up 17% and 23% of ed on fluoroscopic imaging and measured on radiographs and all paediatric fractures, respectively.1 When these fractures compared with actual lengths measured on the bone models. -

Ultrasound-Assisted Closed Reduction of Distal Radius Fractures
SCIENTIFIC ARTICLE Ultrasound-Assisted Closed Reduction of Distal Radius Fractures Narihito Kodama, MD, PhD, Yoshinori Takemura, MD, PhD, Hiroaki Ueba, MD, Shinji Imai, MD, PhD, Yoshitaka Matsusue, MD, PhD Purpose To assess the accuracy and ability of ultrasound for monitoring closed reduction for distal radius fractures. Methods Consecutive patients undergoing ultrasound-guided closed reduction of acute, dis- placed distal radius fractures between January 2003 and December 2006 at our department were enrolled. The control group was extracted from patients who underwent a closed reduction for similar fractures under fluoroscopy or without any imaging assistance. To confirm the accuracy of the ultrasonography measurements, displacement distance values were compared with those on radiographic imaging before and after reduction. X-ray pa- rameters for pre- and postreduction, reduction time, total cost, and success rate were compared between the ultrasound-guided and the control groups. Results The ultrasound-guided group consisted of 43 patients (mean age, 68 y) and the control group consisted of 57 patients, which included 35 patients (mean age, 74 y) with fluoroscopic reduction and of 22 patients (mean age, 72 y) with reduction unaided by imaging. There were no significant displacement differences between radiographic and ultrasound measurements. In x-ray parameters for pre- and postreduction, there were no significant differences between the 2 groups. Ultrasound-guided reduction took longer than the other 2 methods. The success rate of the ultrasound and the fluoroscopic groups were similar (95% and 94%, respectively). Conclusions Our data suggest that ultrasound assistance can aid reduction of distal radius fractures as well as fluoroscopy. (J Hand Surg Am. -

Medical Policy Ultrasound Accelerated Fracture Healing Device
Medical Policy Ultrasound Accelerated Fracture Healing Device Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 497 BCBSA Reference Number: 1.01.05 Related Policies Electrical Stimulation of the Spine as an Adjunct to Spinal Fusion Procedures, #498 Electrical Bone Growth Stimulation of the Appendicular Skeleton, #499 Bone Morphogenetic Protein, #097 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Members Low-intensity ultrasound treatment may be MEDICALLY NECESSARY when used as an adjunct to conventional management (i.e., closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following: Patient comorbidities: Diabetes, Steroid therapy, Osteoporosis, History of alcoholism, History of smoking. Fracture locations: Jones fracture, Fracture of navicular bone in the wrist (also called the scaphoid), Fracture of metatarsal, Fractures associated with extensive soft tissue or vascular damage. Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of delayed union of bones, including delayed union** of previously surgically-treated fractures, and excluding the skull and vertebra. 1 Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of fracture nonunions of bones, including nonunion*** of previously surgically-treated fractures, and excluding the skull and vertebra. Other applications of low-intensity ultrasound treatment are INVESTIGATIONAL, including, but not limited to, treatment of congenital pseudarthroses, open fractures, fresh* surgically-treated closed fractures, stress fractures, arthrodesis or failed arthrodesis. -

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

Clinical Efficacy of Extended Modified Posteromedial Approach Versus
Clinical ecacy of extended modied posteromedial approach versus posterolateral approach for surgical treatment of posterior pilon fracture: a retrospective analysis Qin-Ming Zhang Aliated Hospital of Jining Medical University Hai-Bin Wang Aliated Hospital of Jining Medical University Xiao-Yan Li Aliated Hospital of Jining Medical University Feng-Long Chu Aliated Hospital of Jining Medical University Liang Han Aliated Hospital of Jining Medical University Dong-Mei Li Aliated Hospital of Jining Medical University Bin Wu ( [email protected] ) Alited Hospital of Jining Medical University https://orcid.org/0000-0003-3707-0056 Research article Keywords: posterior pilon fracture, approach, fracture xation, buttress plate Posted Date: March 30th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-19392/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/12 Abstract Background: Posterior pilon fracture is a type of ankle fracture associated with poorer treatment results compared to the conventional ankle fracture. This is partly related to the lack of consensus on the classication, approach selection, and internal xation method for this type of fracture. This study aimed to investigate the clinical ecacy of posterolateral approach versus extended modied posteromedial approach for surgical treatment of posterior pilon fracture. Methods: Data of 67 patients with posterior pilon fracture who received xation with a buttress plate between January 2015 and December 2018 were retrospectively reviewed. Patients received steel plate xation through either the posterolateral approach (n = 35, group A) or the extended modied posteromedial approach (n = 32, group B). Operation time, intraoperative blood loss, excellent and good rate of reduction, fracture healing time, American Orthopaedic Foot & Ankle Society (AOFAS) Ankle- Hindfoot Scale score, and Visual Analogue Scale score were compared between groups A and B. -

Bone Mineral Density and Prevalence of Osteoporosis in Postmenopausal Korean Women with Low-Energy Distal Radius Fractures
ORIGINAL ARTICLE Musculoskeletal Disorders http://dx.doi.org/10.3346/jkms.2016.31.6.972 • J Korean Med Sci 2016; 31: 972-975 Bone Mineral Density and Prevalence of Osteoporosis in Postmenopausal Korean Women with Low-Energy Distal Radius Fractures Hong Jun Jung,1 Ho Youn Park,2 The aim of this study was to evaluate the bone mineral density and the prevalence of Jin Sam Kim,1 Jun-O Yoon,1 osteoporosis in postmenopausal Korean women with low-energy distal radius fractures and and In-Ho Jeon1 compared with those of aged-matched normal Korean women. Two hundred and six patients with distal radius fractures between March 2006 and March 2010 were included in 1Department of Orthopaedic Surgery, Asan Medical Center, School of Medicine, University of Ulsan, this study. Patients were divided into three groups by age; group 1 (50-59 years), group 2 Seoul, Korea; 2Department of Orthopedic Surgery, (60-69 years), and group 3 (70-79 years). Controls were age-matched normal Korean Uijeongbu St. Mary’s Hospital, The Catholic women. The bone mineral density values at all measured sites, except for the spine, were University of Korea, Uijeongbu, Korea significantly lower in group 1 than those of control. While the bone mineral density values Received: 3 July 2015 in groups 2 and 3 were lower than those of controls, these differences were not statistically Accepted: 16 March 2016 significant. All groups had significantly higher prevalence of osteoporosis at the Ward’s triangle; however, at the spine, femoral neck and trochanteric area it was not significantly Address for Correspondence: different from those of age-matched controls. -
PSI Appendix G Version 6.0 Patient Safety Indicators Appendices
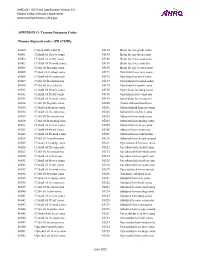
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX G: Trauma Diagnosis Codes Trauma diagnosis codes: (TRAUMID) 80000 Closed skull vault fx 85184 Brain lac nec-proln coma 80001 Cl skull vlt fx w/o coma 85185 Brain lac nec-deep coma 80002 Cl skull vlt fx-brf coma 85186 Brain lacer nec-coma nos 80003 Cl skull vlt fx-mod coma 85189 Brain lacer nec-concuss 80004 Cl skl vlt fx-proln coma 85190 Brain lac nec w open wnd 80005 Cl skul vlt fx-deep coma 85191 Opn brain lacer w/o coma 80006 Cl skull vlt fx-coma nos 85192 Opn brain lac-brief coma 80009 Cl skl vlt fx-concus nos 85193 Opn brain lacer-mod coma 80010 Cl skl vlt fx/cerebr lac 85194 Opn brain lac-proln coma 80011 Cl skull vlt fx w/o coma 85195 Open brain lac-deep coma 80012 Cl skull vlt fx-brf coma 85196 Opn brain lacer-coma nos 80013 Cl skull vlt fx-mod coma 85199 Open brain lacer-concuss 80014 Cl skl vlt fx-proln coma 85200 Traum subarachnoid hem 80015 Cl skul vlt fx-deep coma 85201 Subarachnoid hem-no coma 80016 Cl skull vlt fx-coma nos 85202 Subarach hem-brief coma 80019 Cl skl vlt fx-concus nos 85203 Subarach hem-mod coma 80020 Cl skl vlt fx/mening hem 85204 Subarach hem-prolng coma 80021 Cl skull vlt fx w/o coma 85205 Subarach hem-deep coma 80022 Cl skull vlt fx-brf coma 85206 Subarach hem-coma nos 80023 Cl skull vlt fx-mod coma 85209 Subarach hem-concussion 80024 Cl skl vlt fx-proln coma 85210 Subarach hem w opn wound 80025 Cl skul vlt fx-deep coma 85211 Opn subarach hem-no coma 80026 Cl skull vlt fx-coma nos 85212 -

Distal Radius Fractures (Broken Wrist)
DISEASES & CONDITIONS Distal Radius Fractures (Broken Wrist) The radius is the larger of the two bones of the forearm. The end toward the wrist is called the distal end. A fracture of the distal radius occurs when the area of the radius near the wrist breaks. Distal radius fractures are very common. In fact, the radius is the most commonly broken bone in the arm. Description A distal radius fracture almost always occurs about 1 inch from the end of the bone. The break can occur in many different ways, however. One of the most common distal radius fractures is a Colles fracture, in which the broken fragment of the radius tilts upward. This fracture was first described in 1814 by an Irish surgeon and anatomist, Abraham Colles -- hence the name A Colles fracture occurs when the "Colles" fracture. broken end of the radius tilts upward. Other ways the distal radius can break include: Intra-articular fracture. A fracture that extends into the wrist joint. ("Articular" means "joint.") Extra-articular fracture. A fracture that does not extend into the joint is called an extra-articular fracture. Open fracture. When a fractured bone breaks the skin, it is called an open fracture. These types of fractures require immediate medical attention because of the risk for infection. Comminuted fracture. When a bone is broken into more than two pieces, it is called a comminuted fracture. It is important to classify the type of fracture, because some fractures are more difficult to treat than others. Intra-articular fractures, open fractures, comminuted fractures, and displaced fractures (when the broken pieces of bone do not line up straight).are more difficult to treat, for example. -

Management of Pediatric Forearm Torus Fractures: a Systematic
ORIGINAL ARTICLE Management of Pediatric Forearm Torus Fractures A Systematic Review and Meta-Analysis Nan Jiang, MD,*† Zhen-hua Cao, MD,*‡ Yun-fei Ma, MD,*† Zhen Lin, MD,§ and Bin Yu, MD*† many disadvantages, such as heavy, bulky, and requires a second Objectives: Pediatric forearm torus fracture, a frequent reason for emer- visit to the hospital for removal. These flaws of cast may bring gency department visits, can be immobilized by both rigid cast and non- inconvenience to children as well as their families. In recent years, rigid methods. However, controversy still exists regarding the optimal many pediatric clinicians reported other methods to instead tradi- treatment of the disease. The aim of this study was to compare, in a system- tionally used cast, including soft cast,9,10 Futuro wrist splint,8,11 atic review, clinical efficacy of rigid cast with nonrigid methods for immo- and double Tubigrip.11 Although patients that suffered from fore- bilization of the pediatric forearm torus fractures. arm torus fractures can be immobilized by both rigid cast and non- Methods: Literature search was performed of PubMed and Cochrane Li- rigid materials, controversy still exists in the optimal treatment of brary by 2 independent reviewers to identify randomized controlled trials this fracture. comparing rigid cast with nonrigid methods for pediatric forearm torus The aim of this study was to, in a systematic review and fractures from inception to December 31, 2013, without limitation of publi- meta-analysis, compare clinical efficacy of recently used nonrigid cation language. Trial quality was assessed using the modified Jadad scale. immobilization methods with rigid cast. -

Vanderbilt Sports Medicine
Alabama AAP Fall Meeting Sept.19-20, 2009 Pediatric Fracture Care for the Pediatrician Andrew Gregory, MD, FAAP, FACSM Assistant Professor Orthopedics & Pediatrics Program Director, Sports Medicine Fellowship Vanderbilt University Vanderbilt Sports Medicine Disclosure No conflict of interest - unfortunately for me, I have no financial relationships with companies making products regarding this topic to disclose Objectives Review briefly the differences of pediatric bone Review Pediatric Fracture Classification Discuss subtle fractures in kids Discuss a few other pediatric only conditions 1 Pediatric Skeleton Bone is relatively elastic and rubbery Periosteum is quite thick & active Ligaments are strong relative to the bone Presence of the physis - “weak link” Ligament injuries & dislocations are rare – “kids don’t sprain stuff” Fractures heal quickly and have the capacity to remodel Anatomy of Pediatric Bone Epiphysis Physis Metaphysis Diaphysis Apophysis Pediatric Fracture Classification Plastic Deformation – Bowing usually of fibula or ulna Buckle/ Torus – compression, stable Greenstick – unicortical tension Complete – Spiral, Oblique, Transverse Physeal – Salter-Harris Apophyseal avulsion 2 Plastic deformation Bowing without fracture Often deformed requiring reduction Buckle (Torus) Fracture Buckled Periosteum – Metaphyseal/ diaphyseal junction Greenstick Fracture Cortex Broken on Only One Side – Incomplete 3 Complete Fractures Transverse – Perpendicular to the bone Oblique – Across the bone at 45-60 o – Unstable Spiral – Rotational -

Pediatric Orthopedic Injuries… … from an ED State of Mind
Traumatic Orthopedics Peds RC Exam Review February 28, 2019 Dr. Naminder Sandhu, FRCPC Pediatric Emergency Medicine Objectives to cover today • Normal bone growth and function • Common radiographic abnormalities in MSK diseases • Part 1: Atraumatic – Congenital abnormalities – Joint and limb pain – Joint deformities – MSK infections – Bone tumors – Common gait disorders • Part 2: Traumatic – Common pediatric fractures and soft tissue injuries by site Overview of traumatic MSK pain Acute injuries • Fractures • Joint dislocations – Most common in ED: patella, digits, shoulder, elbow • Muscle strains – Eg. groin/adductors • Ligament sprains – Eg. Ankle, ACL/MCL, acromioclavicular joint separation Chronic/ overuse injuries • Stress fractures • Tendonitis • Bursitis • Fasciitis • Apophysitis Overuse injuries in the athlete WHY do they happen?? Extrinsic factors: • Errors in training • Inappropriate footwear Overuse injuries Intrinsic: • Poor conditioning – increased injuries early in season • Muscle imbalances – Weak muscle near strong (vastus medialus vs lateralus patellofemoral pain) – Excessive tightness: IT band, gastroc/soleus Sever disease • Anatomic misalignments – eg. pes planus, genu valgum or varum • Growth – strength and flexibility imbalances • Nutrition – eg. female athlete triad Misalignment – an intrinsic factor Apophysitis • *Apophysis = natural protruberance from a bone (2ndary ossification centres, often where tendons attach) • Examples – Sever disease (Calcaneal) – Osgood Schlatter disease (Tibial tubercle) – Sinding-Larsen-Johansson -

Upper Extremity Fractures
Department of Rehabilitation Services Physical Therapy Standard of Care: Distal Upper Extremity Fractures Case Type / Diagnosis: This standard applies to patients who have sustained upper extremity fractures that require stabilization either surgically or non-surgically. This includes, but is not limited to: Distal Humeral Fracture 812.4 Supracondylar Humeral Fracture 812.41 Elbow Fracture 813.83 Proximal Radius/Ulna Fracture 813.0 Radial Head Fractures 813.05 Olecranon Fracture 813.01 Radial/Ulnar shaft fractures 813.1 Distal Radius Fracture 813.42 Distal Ulna Fracture 813.82 Carpal Fracture 814.01 Metacarpal Fracture 815.0 Phalanx Fractures 816.0 Forearm/Wrist Fractures Radius fractures: • Radial head (may require a prosthesis) • Midshaft radius • Distal radius (most common) Residual deformities following radius fractures include: • Loss of radial tilt (Normal non fracture average is 22-23 degrees of radial tilt.) • Dorsal angulation (normal non fracture average palmar tilt 11-12 degrees.) • Radial shortening • Distal radioulnar (DRUJ) joint involvement • Intra-articular involvement with step-offs. Step-off of as little as 1-2 mm may increase the risk of post-traumatic arthritis. 1 Standard of Care: Distal Upper Extremity Fractures Copyright © 2007 The Brigham and Women's Hospital, Inc. Department of Rehabilitation Services. All rights reserved. Types of distal radius fracture include: • Colle’s (Dinner Fork Deformity) -- Mechanism: fall on an outstretched hand (FOOSH) with radial shortening, dorsal tilt of the distal fragment. The ulnar styloid may or may not be fractured. • Smith’s (Garden Spade Deformity) -- Mechanism: fall backward on a supinated, dorsiflexed wrist, the distal fragment displaces volarly. • Barton’s -- Mechanism: direct blow to the carpus or wrist.