Medical Policy Ultrasound Accelerated Fracture Healing Device
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

Clinical Efficacy of Extended Modified Posteromedial Approach Versus
Clinical ecacy of extended modied posteromedial approach versus posterolateral approach for surgical treatment of posterior pilon fracture: a retrospective analysis Qin-Ming Zhang Aliated Hospital of Jining Medical University Hai-Bin Wang Aliated Hospital of Jining Medical University Xiao-Yan Li Aliated Hospital of Jining Medical University Feng-Long Chu Aliated Hospital of Jining Medical University Liang Han Aliated Hospital of Jining Medical University Dong-Mei Li Aliated Hospital of Jining Medical University Bin Wu ( [email protected] ) Alited Hospital of Jining Medical University https://orcid.org/0000-0003-3707-0056 Research article Keywords: posterior pilon fracture, approach, fracture xation, buttress plate Posted Date: March 30th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-19392/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/12 Abstract Background: Posterior pilon fracture is a type of ankle fracture associated with poorer treatment results compared to the conventional ankle fracture. This is partly related to the lack of consensus on the classication, approach selection, and internal xation method for this type of fracture. This study aimed to investigate the clinical ecacy of posterolateral approach versus extended modied posteromedial approach for surgical treatment of posterior pilon fracture. Methods: Data of 67 patients with posterior pilon fracture who received xation with a buttress plate between January 2015 and December 2018 were retrospectively reviewed. Patients received steel plate xation through either the posterolateral approach (n = 35, group A) or the extended modied posteromedial approach (n = 32, group B). Operation time, intraoperative blood loss, excellent and good rate of reduction, fracture healing time, American Orthopaedic Foot & Ankle Society (AOFAS) Ankle- Hindfoot Scale score, and Visual Analogue Scale score were compared between groups A and B. -
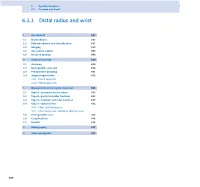
6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -

Bimalleolar Ankle Fracture Fixation of a 13-Year-Old Patient with Two Activascrew™ LAG Bioabsorbable Screws
Bimalleolar ankle fracture fixation of a 13-year-old patient with two ActivaScrew™ LAG bioabsorbable screws. Pierre Lascombes Professor, M.D., Ph.D. For medical professional use, not public. © 2020 Bioretec Ltd. and Prof. Lascombes. All rights reserved. Table of Contents Summary Table ........................................................................................................... 3 1 Case Description .................................................................................................. 4 2 Implants and operative technique ......................................................................... 5 3 Outcome ............................................................................................................... 7 4 Contact Information Concerning the Case ............................................................ 8 For medical professional use, not public Page 2 / 8 © 2020 Bioretec Ltd., Prof. Lascombes. All rights reserved. Summary Table Demographics Patient number: P01 Patient Initials: NX Smoking: No Sex: Female Use of alcohol: No Age: 13 Years Systemic disease: No Height: 158 cm Cont. Medication: No Weight: 40 kg Case description Diagnosis: Dislocation right ankle - bimalleolar fracture Cause of injury: Gymnastic injury Operation Operator: Lascombes Operation year: 2016 Note: Immediate reduction of the Operation description: Open reduction of medial malleolus and fixation with TWO resorbable screws dislocation at emergenry room - ketamine. Surgical treatment 5 hours Operation time:h57 min Immobilisation -

5Th Metatarsal Fracture
FIFTH METATARSAL FRACTURES Todd Gothelf MD (USA), FRACS, FAAOS, Dip. ABOS Foot, Ankle, Shoulder Surgeon Orthopaedic You have been diagnosed with a fracture of the fifth metatarsal bone. Surgeons This tyPe of fracture usually occurs when the ankle suddenly rolls inward. When the ankle rolls, a tendon that is attached to the fifth metatarsal bone is J. Goldberg stretched. Because the bone is weaker than the tendon, the bone cracks first. A. Turnbull R. Pattinson A. Loefler All bones heal in a different way when they break. This is esPecially true J. Negrine of the fifth metatarsal bone. In addition, the blood suPPly varies to different I. PoPoff areas, making it a lot harder for some fractures to heal without helP. Below are D. Sher descriPtions of the main Patterns of fractures of the fifth metatarsal fractures T. Gothelf and treatments for each. Sports Physicians FIFTH METATARSAL AVULSION FRACTURE J. Best This fracture Pattern occurs at the tiP of the bone (figure 1). These M. Cusi fractures have a very high rate of healing and require little Protection. Weight P. Annett on the foot is allowed as soon as the Patient is comfortable. While crutches may helP initially, walking without them is allowed. I Prefer to Place Patients in a walking boot, as it allows for more comfortable walking and Protects the foot from further injury. RICE treatment is initiated. Pain should be exPected to diminish over the first four weeks, but may not comPletely go away for several months. Follow-uP radiographs are not necessary if the Pain resolves as exPected. -

BSUH VFC Initial Management Guidelines Dec 2014
BSUH VFC initial management guidelines Dec 2014 Contents Page Elbow injuries: Radial head / Radial neck fractures 3 Elbow dislocations 3 Shoulder Injuries: Shoulder dislocation 4 ACJ dislocation 4 Proximal Humerus fractures 5 Greater Tuberosity fractures 5 Midshaft Humerus 6 Mid-shaft clavicle fractures 7 Lateral 1/3 Clavicle fractures 8 Medial 1/3 clavicle fractures 9 Soft tissue injury shoulder 11 Calcific tendinitis 11 Common lower limb injuries Foot injuries: 5th Metatarsal fracture 12 Stress fractures 12 5th Midshaft fractures 12 Single Metatarsal fractures 12 Single phalanx fractures 12 Multiple Metatarsal fractures 13 Mid-foot fractures 13 Calcaneal fractures 14 Ankle injuries: Page 1 of 18 Weber A ankle fractures 15 Weber B 15 Weber C 15 Medial malleolus / and Posterior malleolus fractures 15 Bi-tri malleolus fractures 16 Soft tissue ankle injury / Avulsion lateral malleolus 16 TA ruptures 16 Knee injuries Locked Knee 17 Soft tissue knee injury 17 Patella Dislocation 17 Patella fractures 17 Possible Tumours 18 Page 2 of 18 Upper Limb Injuries Elbow injuries Radial head / neck fractures Mason 1 head / borderline Mason 1-2 protocol BAS for comfort only 2/52 and early gentle ROM DC VFC. Patient to contact VFC at 3/52 post injury if struggling to regain ROM Mason 2 >2mm articular step off discuss case with consultant on hot week likely conservative management if unsure d/w upper limb consultants opinion for 2/52 repeat x-ray and review in VFC Mason 3 head # or >30degrees neck angulation = Urgent Ref to UL clinic (LL or LT) for discussion with regards to surgical management. -

Treatment of Distal Radius Fractures – Clinical Outcome, Regional Variation and Health Economics
From THE DEPARTMENT OF CLINICAL SCIENCE AND EDUCATION, SÖDERSJUKHUSET Karolinska Institutet, Stockholm, Sweden TREATMENT OF DISTAL RADIUS FRACTURES – CLINICAL OUTCOME, REGIONAL VARIATION AND HEALTH ECONOMICS Jenny Saving Stockholm 2019 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by Eprint AB 2019 © Jenny Saving, 2019 ISBN 978-91-7831-339-6 Treatment of distal radius fractures – clinical outcome, regional variation and health economics THESIS FOR DOCTORAL DEGREE (Ph.D.) By Jenny Saving, MD Principal Supervisor: Opponent: MD, Associate Professor Anders Enocson MD, Professor Lars Adolfsson Karolinska Institutet University of Linköping Department of Clinical Science and Education Department of Clinical and Experimental Division of Orthopaedics Medicine Södersjukhuset Examination Board: Co-supervisor(s): MD, Professor Hans Mallmin MD, PhD, Cecilia Mellstrand Navarro Uppsala University Karolinska Institutet Department of Surgical Sciences Department of Clinical Science and Education Section of Orthopaedics Division of Hand Surgery Södersjukhuset MD, Associate Professor Rüdiger Weiss Karolinska Institutet MD, Professor Sari Ponzer Department of Molecular Medicine and Surgery Karolinska Instiutet Karolinska University Hospital Department of Clinical Science and Education Division of Orthopaedics MD, Professor Olof Nilsson Södersjukhuset Uppsala University Department of Surgical Sciences Section of Orthopaedics To my family 3 4 ABSTRACT A distal radius fracture (DRF) remains the most common fracture encountered in health care. DRFs have traditionally been treated with a plaster or surgically with percutaneous methods. Since the end of the 20th century, when internal fixation with a volar locking plate (VLP) was introduced, the incidence of DRF surgery in general and of plating in particular have increased markedly. -

Metacarpal Fractures
METACARPAL FRACTURES BY LORYN P. WEINSTEIN, MD, AND DOUGLAS P. HANEL, MD The majority of metacarpal fractures are closed injuries amenable to conservative treatment with external immobilization and subsequent rehabilitation. Internal fixation is favored for unstable fracture patterns and patients who require early motion. Percutaneous pinning usually is successful for metacarpal neck fractures and comminuted head fractures. Shaft and base fractures can be treated with pinning or open reduction and internal fixation; the latter, being more rigid, allows early rehabilitation. External fixation has a limited yet defined role for metacarpal fractures with complex soft-tissue injury and/or segmental bone loss. The recent development of bioabsorbable implants holds promise for skeletal rigidity with minimal soft-tissue morbidity, but long-term in vivo data support- ing the use of these implants is not currently available. Copyright © 2002 by the American Society for Surgery of the Hand arly treatment of metacarpal fractures was lim- Surgical techniques rapidly expanded to include ret- ited to the only tools available: manipulation rograde fracture pinning, intramedullary pinning, and Eand casting. The discovery of percutaneous transfixion pinning. Many of the K-wires in use today fracture fixation near the turn of the century opened have the same diamond-shaped tip and sizing speci- up a new world of possibilities. It was 25 years after fications as the original design. Bennett’s original manuscript that Lambotte de- The first plate and screw set for the hand was scribed the first surgical stabilization of a basilar introduced in the late 1930s. By today’s standards, the thumb fracture by using a thin carpenter’s nail.1 By Hermann Metacarpal Bone Set was quite lean; it 1913, Lambotte had authored a fracture text with included 3 longitudinal plates of 2, 3, and 4 holes, a multiple examples of pinning, wiring, and plating of drill, screwdriver, and 9 screws.1 Improvements in hand fractures. -

OUTPATIENT REHABILITATION for a PATIENT FOLLOWING a SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE a Doctoral Project a Comprehensi
OUTPATIENT REHABILITATION FOR A PATIENT FOLLOWING A SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE A Doctoral Project A Comprehensive Case Analysis Presented to the faculty of the Department of Physical Therapy California State University, Sacramento Submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHYSICAL THERAPY by Julie Hammond FALL 2017 © 2017 Julie Hammond ALL RIGHTS RESERVED ii OUTPATIENT REHABILITATION FOR A PATIENT FOLLOWING A SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE A Doctoral Project by Julie Hammond Approved by: _____________________________________, Committee Chair Edward Barakatt, PT, PhD _____________________________________, First Reader William Garcia, PT, DPT, OCS, FAAOMPT _____________________________________, Second Reader Rafael Escamilla, PhD, PT, CSCS ____________________________ Date iii Student: Julie Hammond I certify that this student has met the requirements for format contained in the University format manual, and that this project is suitable for shelving in the Library and credit is to be awarded for the project. __________________________________, Department Chair ____________ Michael McKeough, PT, EdD Date Department of Physical Therapy iv Abstract of OUTPATIENT REHABILITATION FOR A PATIENT FOLLOWING A SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE by Julie Hammond A 46 year old woman with a right surgically stabilized trimalleolar fracture was seen for physical therapy treatment for 13 sessions from 06/17/2016 to 09/16/2106 at an outpatient pro bono physical therapy clinic. Treatment was provided by a student physical therapist under the supervision of a licensed physical therapist. The patient was evaluated at the initial encounter with manual muscle test, goniometric measurements, single leg balance test, Timed Up and Go test, and a self- report questionnaire (Foot and Ankle Ability Measure). -

A Study on Management of Comminuted Colles Fracture by Closed Reduction and Ulnocarpal Stabilisation with 2 K-Wires
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 4 Ver. IV (Apr. 2015), PP 45-51 www.iosrjournals.org A Study on Management of Comminuted Colles Fracture by Closed Reduction and Ulnocarpal Stabilisation with 2 K-Wires Dr. Addepalli Srinivasa Rao, M.S, M.ch (Ortho), Dr. K.N.Sandeep M.S(Ortho) Department of Orthopaedics, Siddhartha Medical College, Vijayawada, Andhrapradesh ,India 520008 Abstract Background – In comminuted Colles fractures treated by conventional method , malunion during healing due to progressive radial collapse is a common complication. Many modalities of treatment have been described with their merits and demerits. Ulnocarpal stabilization is an effective method to prevent radial collapse and hence this study. Materials And Methods – A prospective study of 100 patients of comminuted Colles fracture between 20-70 years age irrespective of sex treated by closed reduction and percutaneous stabilization of ulnocarpal articulation and above elbow POP cast for 6weeks has been presented. Patients were evaluated at 1 year follow up and functionally by Sarmiento’s modification of Lindstrom criteria and Gartland and Werley’s criteria. Results – Excellent to good results in 92%,fair in 4% and poor in 4% of total cases. Complications observed were malunion (n=6), pin tract infection (n=7), pullout of k-wire (n=5), sudeck’s osteodystrophy (n=7), residual pain (n=4),reduced grip strength (n=8) . Conclusion – Percutaneous pinnng by ulnocarpal stabilization is minimally invasive, yet an effective method to maintain the reduction and stability of distal radioulnar joint and radial collapse during healing ,even when the fracture is grossly comminuted ,intraarticular or unstable . -

Bimalleolar Fracture of Ankle Joint Managed by Tension Band Wiring Technique: a Prospective Study Dr
Scholars Journal of Applied Medical Sciences (SJAMS) ISSN 2320-6691 (Online) Sch. J. App. Med. Sci., 2014; 2(1D):428-432 ISSN 2347-954X (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Research Article Bimalleolar Fracture of Ankle Joint Managed By Tension Band Wiring Technique: A Prospective Study Dr. Maruthi CV*1, Dr.Venugopal N2, Dr. Nanjundappa HC2, Dr. Siddalinga swamy MK2 1Assistant Professor, Department of Orthopaedics, MVJ MC and RH, Hoskote, Bangalore, India 2Professor, Dept of Orthopaedics, MVJ MC and RH, Hoskote, Bangalore, India 3MVJ Medical College & Research Hospital, Hoskote, Bangalore -562 114, India *Corresponding author Dr. Maruthi CV Email: Abstract: Ankle fractures are the most commonly encountered by most of the orthopaedic surgeons. According to the lauge Hansen’s classification five different types can be seen. The surgical treatment of adduction, abduction and supination external rotation type of injuries leading to bimalleolar fractures can be fixed with either tension band technique or cancellous screws. Here we are done a study to evaluate the benefits of tension band wiring technique in the management of bimalleolar fractures of the ankle. In our study, 40 cases of bimalleolar fracture of ankle joint of above mentioned types were admitted in Department of Orthopaedics, between February 2009 and November 2013 was included. We included patients above 20 and below 58 years. We excluded patients with pronation external rotation, vertical compression and trimalleolar fractures, pathological fractures, compound fractures and who are medically unfit and at extremely high anaesthesia risk. All the patients, operated by open reduction and internal fixation using tension band wiring technique. -

Risk Factors for Fracture and Fracture Severity of the Distal Radius and Ankle. What About Osteoporosis, Celiac Disease and Obesity?
Risk factors for fracture and fracture severity of the distal radius and ankle. What about osteoporosis, celiac disease and obesity? Anja Myhre Hjelle Thesis for the degree of Philosophiae Doctor (PhD) University of Bergen, Norway 2021 Risk factors for fracture and fracture severity of the distal radius and ankle. What about osteoporosis, celiac disease and obesity? Anja Myhre Hjelle ThesisAvhandling for the for degree graden of philosophiaePhilosophiae doctorDoctor (ph.d (PhD). ) atved the Universitetet University of i BergenBergen Date of defense:2017 17.06.2021 Dato for disputas: 1111 © Copyright Anja Myhre Hjelle The material in this publication is covered by the provisions of the Copyright Act. Year: 2021 Title: Risk factors for fracture and fracture severity of the distal radius and ankle. Name: Anja Myhre Hjelle Print: Skipnes Kommunikasjon / University of Bergen 1 CONTRIBUTORS This work is the result of a collaboration between and funding from The Department of Global Public Health and Primary Care at the University of Bergen, The Department of Rheumatology at the District Hospital of Førde, and The Centre for Health Research in Sogn og Fjordane (a collaborative effort between Førde Health Trust and the health studies department of the Western Norway University College of Applied Sciences). We have also collaborated with The Department of Orthopedic surgery and the Department of Radiology at the District Hospital of Førde, The Departement of Rheumatology at Haukeland University Hospital, Bergen, and The KB Jebsen Coeliac Disease Research Centre, University of Oslo. We are grateful for additional funding received from The Norwegian association for Celiac Disease (Norsk Cøliakiforening) in 2012 and 2015.