Metacarpal Fractures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Policy Ultrasound Accelerated Fracture Healing Device
Medical Policy Ultrasound Accelerated Fracture Healing Device Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 497 BCBSA Reference Number: 1.01.05 Related Policies Electrical Stimulation of the Spine as an Adjunct to Spinal Fusion Procedures, #498 Electrical Bone Growth Stimulation of the Appendicular Skeleton, #499 Bone Morphogenetic Protein, #097 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Members Low-intensity ultrasound treatment may be MEDICALLY NECESSARY when used as an adjunct to conventional management (i.e., closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following: Patient comorbidities: Diabetes, Steroid therapy, Osteoporosis, History of alcoholism, History of smoking. Fracture locations: Jones fracture, Fracture of navicular bone in the wrist (also called the scaphoid), Fracture of metatarsal, Fractures associated with extensive soft tissue or vascular damage. Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of delayed union of bones, including delayed union** of previously surgically-treated fractures, and excluding the skull and vertebra. 1 Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of fracture nonunions of bones, including nonunion*** of previously surgically-treated fractures, and excluding the skull and vertebra. Other applications of low-intensity ultrasound treatment are INVESTIGATIONAL, including, but not limited to, treatment of congenital pseudarthroses, open fractures, fresh* surgically-treated closed fractures, stress fractures, arthrodesis or failed arthrodesis. -

Treatment of Comminuted Fractures of the Base of the Thumb Metacarpal Using a Cemented Bone-K-Wire Frame
Hand Surgery and Rehabilitation 38 (2019) 44–51 Available online at ScienceDirect www.sciencedirect.com Original article Treatment of comminuted fractures of the base of the thumb metacarpal using a cemented bone-K-wire frame Traitement des fractures comminutives de la base du premier me´tacarpien graˆce a` un cadre os-broches-ciment W. Duan, X. Zhang, Y. Yu, Z. Zhang *, X. Shao, W. Du Department of Hand Surgery, Third Hospital of Hebei Medical University, Shijiazhuang, Hebei 050051, PR China ARTICLE INFO ABSTRACT Article history: We aimed to describe the treatment of comminuted fractures of the base of the thumb metacarpal using a Received 13 June 2018 cemented bone-K-wire frame. Between March 2010 and January 2016, 41 fractures of the base of the thumb Received in revised form 8 August 2018 were treated using a cemented bone-K-wire frame. The mean age of the patients was 34 years. The patients’ Accepted 7 September 2018 history included a fall onto the hand in 7 cases, direct trauma in 31 cases, and polytrauma with an unclear Available online 11 October 2018 mechanism of injury in 3 cases. At the final follow-up, hand grip and pinch strength were measured using a dynamometer. All measurements were compared with those of the opposite hand. The patients were assessed Keywords: functionally using the Smith and Cooney score.All K-wires were left in place until the bone healed. Bone healing Cemented K-wire frame was achieved in all thumbs in an average of 5.2 weeks. Follow-up averaged 27 months. The mean hand pinch External fixator Rolando fracture andgripstrengthwas8.7 kg Æ 2.4 kgand38.4 kg Æ 5.9 kg,respectively.Themeanmeasurementsontheopposite Thumb side were 9.2 kg Æ 2.5 kg and 40.2 kg Æ 6.6 kg, respectively. -
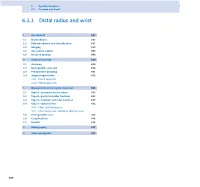
6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -

Approach to Hand Conditions
Approach to Hand Conditions Alphonsus Chong Associate Professor, Department of Orthopaedic Surgery, Singapore Senior Consultant, Department of Hand and Reconstructive Microsurgery, Singapore http://bit.ly/39fuCIK [email protected] Scope • Introduction – Slides at http://bit.ly/39fuCIK • And other material at: https://nus.edu/2Mh4e4s • Physical examination http://bit.ly/39fuCIK : these slides • Traumatic injuries – open and closed • Peripheral nerve problems • Masses in the hand and wrist • Tendinopathy and tendinitis • Deformity https://nus.edu/2Mh4e4s: hand wiki 3 History Taking • Pain – different aspects • Handedness • Deformity • Job v – Congenital • Hobbies – Acquired - ? Traumatic • Previous injury/ surgery • Decreased rangev of motion • Weakness • For acute trauma/conditions: • Numbness – Last meal v • Others e.g. triggering, instability – Mechanism of injury – Time/date of injury Expose both sides: subcutaneous border Scars, wasting, deformity of ulna and elbow- rheumatoid nodules Completeness and fluidity of motion Scars, wasting, deformity Quick Nerve Screen Median Nerve Radial Nerve Ulnar nerve Traumatic Injuries – Open Injuries Open traumatic injuries are a staple work of hand surgeons. Assessment of Hand – Work through the tissues (see Apley) • Skin – note size and types of wounds • Vessels - circulation • Nerves – sensation and motor • Muscle and Tendons – individual flexor and extensor tendon testing • Bones & Joints – appropriate x-rays to assess fractures/ dislocation What do you see? • LOOK • LOOK – Loss of cascade • -

Part Fracture Dislocation Due to Stress Concentration at Intramedullary Nail End 1Devendra Chouhan, 2Vishal Kumar, 3Manish Kundanmal Kothari, 4Mandeep S Dhillon
JPMER Devendra Chouhan et al 10.5005/jp-journals-10028-1142 CASE REPORT Dissociation of Shaft of Humerus from Head in Three- part Fracture Dislocation due to Stress Concentration at Intramedullary Nail End 1Devendra Chouhan, 2Vishal Kumar, 3Manish Kundanmal Kothari, 4Mandeep S Dhillon ABSTRACT authors best knowledge. We report the first such case A three-part fracture dislocation of the proximal humerus of three-part fracture dislocation involving the greater usually dissociates from the shaft at the level of the surgical tuberosity and proximal shaft of humerus with a 25 years neck or the anatomical neck. Dissociation from the shaft below old Rush nail in situ. this level has not reported in the literature before. Here we describe the injury of a middle aged patient with a three-part CASE REPORT fracture dislocation of the humerus with dissociation of the head from the shaft at the level of proximal shaft humerus with A 60-year-old male presented in the emergency depart- a 25 years old Rush nail in situ. The dislocated head was found ment with acute pain in right shoulder following road abutting the thoracic wall. This case report highlights the effect traffic accident 8 hours ago. He was travelling on a bike of stress concentration at intramedullary nail ends in the upper limb as well as the need for an extended approach when the when a car hit him from the side. He was violently thrown dislocated head appears close to the thoracic wall. off his motorcycle followed by fall on an outstretched hand. He had no other complaints. -

Treatment of Distal Radius Fractures – Clinical Outcome, Regional Variation and Health Economics
From THE DEPARTMENT OF CLINICAL SCIENCE AND EDUCATION, SÖDERSJUKHUSET Karolinska Institutet, Stockholm, Sweden TREATMENT OF DISTAL RADIUS FRACTURES – CLINICAL OUTCOME, REGIONAL VARIATION AND HEALTH ECONOMICS Jenny Saving Stockholm 2019 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by Eprint AB 2019 © Jenny Saving, 2019 ISBN 978-91-7831-339-6 Treatment of distal radius fractures – clinical outcome, regional variation and health economics THESIS FOR DOCTORAL DEGREE (Ph.D.) By Jenny Saving, MD Principal Supervisor: Opponent: MD, Associate Professor Anders Enocson MD, Professor Lars Adolfsson Karolinska Institutet University of Linköping Department of Clinical Science and Education Department of Clinical and Experimental Division of Orthopaedics Medicine Södersjukhuset Examination Board: Co-supervisor(s): MD, Professor Hans Mallmin MD, PhD, Cecilia Mellstrand Navarro Uppsala University Karolinska Institutet Department of Surgical Sciences Department of Clinical Science and Education Section of Orthopaedics Division of Hand Surgery Södersjukhuset MD, Associate Professor Rüdiger Weiss Karolinska Institutet MD, Professor Sari Ponzer Department of Molecular Medicine and Surgery Karolinska Instiutet Karolinska University Hospital Department of Clinical Science and Education Division of Orthopaedics MD, Professor Olof Nilsson Södersjukhuset Uppsala University Department of Surgical Sciences Section of Orthopaedics To my family 3 4 ABSTRACT A distal radius fracture (DRF) remains the most common fracture encountered in health care. DRFs have traditionally been treated with a plaster or surgically with percutaneous methods. Since the end of the 20th century, when internal fixation with a volar locking plate (VLP) was introduced, the incidence of DRF surgery in general and of plating in particular have increased markedly. -

Listen to the Associated Podcast Episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, Available at Theradiologyreview.Com O
MSK: Fractures for Radiology Board Study, Matt Covington, MD Listen to the associated podcast episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, available Listen to associated Podcast episodes: ABR Core Exam, Multisystemic Diseases Parts 1-3, available at at theradiologyreview.com or on your favorite podcast directory. Copyrighted. theradiologyreview.com or on your favorite podcast direcry. Fracture resulting From abnormal stress on normal bone = stress Fracture Fracture From normal stress on abnormal bone = insuFFiciency Fracture Scaphoid Fracture site with highest risk for avascular necrosis (proximal or distal)? Proximal pole scaphoid Fractures are at highest risk For AVN Comminuted Fracture at the base oF the First metacarpal = Rolando Fracture Non-comminuted Fracture at base oF the First metacarpal = Bennett Fracture The pull oF which tendon causes the dorsolateral dislocation in a Bennett fracture? The abductor pollicus longus tendon. Avulsion Fracture at the base oF the proximal phalanx with ulnar collateral ligament disruption = Gamekeeper’s thumb. Same Fracture but adductor tendon becomes caught in torn edge oF the ulnar collateral ligament? Stener’s lesion. IF Stener’s lesion is present this won’t heal on its own so you need surgery. You shouldn’t image a Gamekeeper’s thumb with stress views because you can convert it to a Stener’s lesion. Image with MRI instead. Distal radial Fracture with dorsal angulation = Colle’s Fracture (C to D= Colle’s is Dorsal) Distal radial Fracture with volar angulation = Smith’s Fracture (S -

Proximal Humerus Fracture After Keyhole Biceps Tenodesis
A Case Report & Literature Review Proximal Humerus Fracture After Keyhole Biceps Tenodesis Stefanie N. Reiff, BA, Shane J. Nho, MD, MS, and Anthony A. Romeo, MD is the only one published in English. The patient pro- Abstract vided written informed consent for print and electronic A biceps tenodesis is a common surgical procedure that publication of this case report. is often carried out in conjunction with other surgical shoulder repairs to relieve biceps tendonitis. This case CASE REPORT presents a 50-year-old woman who suffered a humerus The patient, a 50-year-old woman, underwent left shoul- fracture following an open keyhole biceps tenodesis. The potential reasons for the fracture as well as a brief der revision arthroscopic subacromial decompression analysis of the technique itself are presented. To our and open biceps tenodesis. Past medical history was sig- knowledge, this is the first case report of a humerus frac- nificant for insulin-dependent diabetes mellitus (onset age, ture following keyhole biceps tenodesis in the English- 15 years) and hypothyroidism. Past surgical history was language literature. notable for left shoulder os acromiale with arthroscopic subacromial decompression performed 7 months before iceps tendonitis, a relatively common condition the revision surgery pertinent to this case. Tenodesis of the that affects the shoulder, causes pain over its biceps tendon was indicated on the basis of past surgical anterior aspect, near the bicipital groove and history, clinical examination in the office, and intraopera- -

A Study on Management of Comminuted Colles Fracture by Closed Reduction and Ulnocarpal Stabilisation with 2 K-Wires
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 4 Ver. IV (Apr. 2015), PP 45-51 www.iosrjournals.org A Study on Management of Comminuted Colles Fracture by Closed Reduction and Ulnocarpal Stabilisation with 2 K-Wires Dr. Addepalli Srinivasa Rao, M.S, M.ch (Ortho), Dr. K.N.Sandeep M.S(Ortho) Department of Orthopaedics, Siddhartha Medical College, Vijayawada, Andhrapradesh ,India 520008 Abstract Background – In comminuted Colles fractures treated by conventional method , malunion during healing due to progressive radial collapse is a common complication. Many modalities of treatment have been described with their merits and demerits. Ulnocarpal stabilization is an effective method to prevent radial collapse and hence this study. Materials And Methods – A prospective study of 100 patients of comminuted Colles fracture between 20-70 years age irrespective of sex treated by closed reduction and percutaneous stabilization of ulnocarpal articulation and above elbow POP cast for 6weeks has been presented. Patients were evaluated at 1 year follow up and functionally by Sarmiento’s modification of Lindstrom criteria and Gartland and Werley’s criteria. Results – Excellent to good results in 92%,fair in 4% and poor in 4% of total cases. Complications observed were malunion (n=6), pin tract infection (n=7), pullout of k-wire (n=5), sudeck’s osteodystrophy (n=7), residual pain (n=4),reduced grip strength (n=8) . Conclusion – Percutaneous pinnng by ulnocarpal stabilization is minimally invasive, yet an effective method to maintain the reduction and stability of distal radioulnar joint and radial collapse during healing ,even when the fracture is grossly comminuted ,intraarticular or unstable . -

Org Tibia (Shinbone) Shaft Fractures
.org Tibia (Shinbone) Shaf Fractures Page ( 1 ) The tibia, or shinbone, is the most common fractured long bone in your body. The long bones include the femur, humerus, tibia, and fi bula. A tibial shaf fracture occurs along the length of the bone, below the knee and above the ankle. Because it typically takes a major force to break a long bone, other injuries of en occur with these types of fractures. Anatomy The lower leg is made up of two bones: the tibia and fi bula. The tibia is the larger of the two bones. It supports most of your weight and is an important part of both the knee joint and ankle joint. The tibia is the larger bone in your lower leg. Tibial shaf fractures occur Types of Tibial Shaf Fractures along the length of the bone. The tibia can break in several ways. The severity of the fracture usually depends on the amount of force that caused the break. The fi bula is of en broken as well. Common types of tibial fractures include: Stable fracture: This type of fracture is barely out of place. The broken ends of the bones basically line up correctly and are aligned. In a stable fracture, the bones usually stay in place during healing. Displaced fracture: When a bone breaks and is displaced, the broken ends are separated and do not line up. These types of fractures of en require surgery to put the pieces back together. Transverse fracture: This type of fracture has a horizontal fracture line. This fracture can be unstable, especially if the fi bula is also broken. -

Common Fractures and Dislocations of the Hand
CME Common Fractures and Dislocations of the Hand Neil F. Jones, M.D. Learning Objectives: After reading this article, the participant should be able Jesse B. Jupiter, M.D. to: 1. Describe the concept of early protected movement with Kirschner-wired Donald H. Lalonde, M.D. finger fractures to the hand therapist. 2. Choose the most appropriate method Orange, Calif.; Boston, Mass.; and of fracture fixation to achieve the goal of a full range of motion. 3. Describe the Saint John, New Brunswick, Canada methods of treatment available for the most common fractures and dislocations of the hand. Background: The main goal of treatment of hand and finger fractures and dislocations is to attain a full range of wrist and nonscissoring finger motion after the treatment is accomplished. This CME article consists of literature review, illustrations, movies, and an online CME examination to bring the participant recent available information on the topic. Methods: The authors reviewed literature regarding the most current treat- ment strategies for common hand and finger fractures and dislocations. Films were created to illustrate operative and rehabilitation methods used to treat these problems. A series of multiple-choice questions, answers, discussions, and references were written and are provided online so that the participant can receive the full benefit of this review. Results: Many treatment options are available, from buddy and Coban taping to closed reduction with immobilization; percutaneous pins or screws; and open reduction with pins, screws, or plates. Knowledge of all available options is important because all can be used to achieve the goal of treatment in the shortest time possible. -

Functional Outcome of Orthogonal Plating in Treatment of Distal
International Journal of Orthopaedics Sciences 2018; 4(2): 78-83 ISSN: 2395-1958 IJOS 2018; 4(2): 78-83 © 2018 IJOS Functional outcome of orthogonal plating in treatment www.orthopaper.com Received: 01-02-2018 of distal humerus fracture Accepted: 05-03-2018 Rajeev Kelkar Rajeev Kelkar and Deepak Singh Rajput Assistant professor, Department of Orthopaedics, MGM Medical College & M.Y. Hospital, Indore, DOI: https://doi.org/10.22271/ortho.2018.v4.i2e.41 M.P, India Abstract Deepak Singh Rajput Background: The study was conducted to evaluate the outcome of orthogonal plating system in distal Resident, Department of humerus intraarticular fracture. Orthopaedics, M.Y. Hospital, Material and Methods: 15 patients of age between 18 to 60 yrs with fracture distal end of humerus with Indore, M.P, India intraarticular extension were evaluated, with the mean age group of 37 to find the functional outcome of Orthogonal plating using olecranon osteotomy approach. Results: The mean union time was 9.53 weeks. The arc of flexion was 99.66o. Average mayo elbow performance score (MEPS) was 83. There were 2 case of infection. One case of implant failure noted secondary to infection leading to implant removal. Discussion and Conclusion: The following results were assessed: operating time, arc of flexion and extension, time to fracture union, functional recovery, and complications. By using proper principles of stable fracture fixation and appropriate exposure in intraarticular fracture (with transolecrenon approach) a good reduction can be achieved which leads to good union, which helps in early mobilization and restoring elbow functions with early intensive physiotherapy. Keywords: Functional outcome, plating, treatment, humerus fracture Introduction Distal Humerus fracture are relatively uncommon and comprise approximately 2-6 % of all fractures [2, 3, 21].