Psychiatric Medication Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HALDOL Brand of Haloperidol Injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia
HALDOL® brand of haloperidol injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. HALDOL Injection is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS). DESCRIPTION Haloperidol is the first of the butyrophenone series of major antipsychotics. The chemical designation is 4-[4-(p-chlorophenyl)-4-hydroxypiperidino] 4’-fluorobutyrophenone and it has the following structural formula: HALDOL (haloperidol) is available as a sterile parenteral form for intramuscular injection. The injection provides 5 mg haloperidol (as the lactate) and lactic acid for pH adjustment between 3.0 – 3.6. -

Medication: Amitriptyline 10 Mg
Amitriptyline (Elavil) COMPLEX CHRONIC DISEASES PROGRAM Medication Handout Date: May 15, 2018 Medication: Amitriptyline 10 mg What is Amitriptyline? Amitriptyline belongs to a group of medications called tricyclic antidepressants (TCAs) that were first used to treat depression. It works by altering the levels of certain neuro- transmitters in the brain such as noradrenalin and serotonin. They have since been found to be effective for many different uses such as: pain, helping with sleep quality (but is not a sleeping pill), irritable bowel syndrome (with diarrhea), migraine prevention, and interstitial cystitis. Expected Benefit: Usually takes several weeks to notice a benefit You may not notice a benefit until you get to a dose of 25 mg Watch for possible side effects: This list of side effects is important for you to be aware of; however, it is also important to remember that not all side effects happen to all people. Many of these less serious side effects will improve over the first few days of taking the medications. If you have problems with these side effects talk with your doctor or pharmacist: Dry mouth – this is the most common side; the others are much less frequent Hangover effect – too sleepy in the morning Blurred vision Urinary retention, trouble with urination Tiredness, dizziness that is more than usual Diarrhea or constipation Stopping the medication: Do NOT stop taking this medication suddenly without asking your doctor – this medication is usually decreased slowly (at higher doses) before it is stopped completely How to use this medication: Take this medication with or without food Dosing Schedule: Start with 5 mg (½ tablet) 2 hrs before bed Increase dose according to table below Many patients can only tolerate 20 or 30 mg If you don’t have dry mouth or side effects, you can continue slowly increasing the dose to a maximum of 70 mg You can stay at a lower dose (stop increasing) if you get side effects (usually dry mouth). -
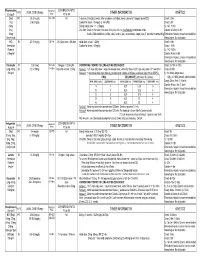
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50 and 75 mg Antidepressant AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road Unit #1 August 29, 2018 Vaughan, ON L4K 4N7 Control No.: 217626 1 PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50, 75 mg THERAPEUTIC CLASSIFICATION Antidepressant ACTIONS AND CLINICAL PHARMACOLOGY Amitriptyline hydrochloride is a tricyclic antidepressant with sedative properties. Its mechanism of action in man is not known. Amitriptyline inhibits the membrane pump mechanism responsible for the re-uptake of transmitter amines, such as norepinephrine and serotonin, thereby increasing their concentration at the synaptic clefts of the brain. Amitriptyline has pronounced anticholinergic properties and produces EKG changes and quinidine-like effects on the heart (See ADVERSE REACTIONS). It also lowers the convulsive threshold and causes alterations in EEG and sleep patterns. Orally administered amitriptyline is readily absorbed and rapidly metabolized. Steady-state plasma concentrations vary widely and this variation may be genetically determined. Amitriptyline is primarily excreted in the urine, mostly in the form of metabolites, with some excretion also occurring in the feces. INDICATIONS AND CLINICAL USE ELAVIL® (amitriptyline hydrochloride) is indicated in the drug management of depressive illness. ELAVIL® may be used in depressive illness of psychotic or endogenous nature and in selected patients with neurotic depression. Endogenous depression is more likely to be alleviated than are other depressive states. ELAVIL® ®, because of its sedative action, is also of value in alleviating the anxiety component of depression. As with other tricyclic antidepressants, ELAVIL® may precipitate hypomanic episodes in patients with bipolar depression. These drugs are not indicated in mild depressive states and depressive reactions. -

Psychiatric Medications in Behavioral Healthcarev5
Copyright © The University of South Florida, 2012 Psychiatric Medications in Behavioral Healthcare An Important Notice None of the pages in this tutorial are meant to be a replacement for professional help. The science of medicine is constantly changing, and these changes alter treatment and drug therapies as a result of what is learned through research and clinical experience. The author has relied on resources believed to be reliable at the time material was developed. However, there is always the possibility of human error or changes in medical science and neither the authors nor the University of South Florida can guarantee that all the information in this program is in every respect accurate or complete and they are not responsible for any errors or omissions or for the results obtained from the use of such information. Each person that reads this program is encouraged to confirm the information with other sources and understand that it not be interpreted as medical or professional advice. All medical information needs to be carefully reviewed with a health care provider. Course Objectives At the completion of this program participants should be able to: • Identify at 5 categories of medications used to treat the symptoms of psychiatric disorders, the therapeutic effects of medications in each category, and the side effects associated with medications in each category. • Identify at least 5 medications and the benefits of those medications as compared to the medications. • Identify at least 5 reasons that a person may stop taking medications or not take medications as prescribed. • Demonstrate your learned understanding of psychiatric medications by passing the combined post‐ tests. -

The Psychoactive Effects of Psychiatric Medication: the Elephant in the Room
Journal of Psychoactive Drugs, 45 (5), 409–415, 2013 Published with license by Taylor & Francis ISSN: 0279-1072 print / 2159-9777 online DOI: 10.1080/02791072.2013.845328 The Psychoactive Effects of Psychiatric Medication: The Elephant in the Room Joanna Moncrieff, M.B.B.S.a; David Cohenb & Sally Porterc Abstract —The psychoactive effects of psychiatric medications have been obscured by the presump- tion that these medications have disease-specific actions. Exploiting the parallels with the psychoactive effects and uses of recreational substances helps to highlight the psychoactive properties of psychi- atric medications and their impact on people with psychiatric problems. We discuss how psychoactive effects produced by different drugs prescribed in psychiatric practice might modify various disturb- ing and distressing symptoms, and we also consider the costs of these psychoactive effects on the mental well-being of the user. We examine the issue of dependence, and the need for support for peo- ple wishing to withdraw from psychiatric medication. We consider how the reality of psychoactive effects undermines the idea that psychiatric drugs work by targeting underlying disease processes, since psychoactive effects can themselves directly modify mental and behavioral symptoms and thus affect the results of placebo-controlled trials. These effects and their impact also raise questions about the validity and importance of modern diagnosis systems. Extensive research is needed to clarify the range of acute and longer-term mental, behavioral, and physical effects induced by psychiatric drugs, both during and after consumption and withdrawal, to enable users and prescribers to exploit their psychoactive effects judiciously in a safe and more informed manner. -

PERPHENAZINE and AMITRIPTYLINE HYDROCHLORIDE- Perphenazine and Amitriptyline Hydrochloride Tablet, Film Coated Mylan Pharmaceuticals Inc
PERPHENAZINE AND AMITRIPTYLINE HYDROCHLORIDE- perphenazine and amitriptyline hydrochloride tablet, film coated Mylan Pharmaceuticals Inc. ---------- WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug- treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Perphenazine and amitriptyline hydrochloride is not approved for the treatment of patients with dementia- related psychosis (see WARNINGS). Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of perphenazine and amitriptyline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. -

Amitriptyline (Elavil): Important Patient Information
What is most important to remember? If you have questions: Strong Internal Medicine • You must check to make sure that it is safe for you to take Ask your doctor, nurse or pharmacist for amitriptyline with all of your other more information about amitriptyline medicines and health problems (Elavil®). • Do not start any new medications, over-the-counter drugs or herbal remedies without talking to your doctor • Contact your prescriber If your symptoms or health problems do not get any better or they become worse • This medicine comes with an Strong Internal Medicine extra patient fact sheet called a 601 Elmwood Avenue Medication Guide. Read it with Ambulatory Care Facility, 5th Floor care. Read it again each time this Rochester, NY 14642 Phone: (585) 275 -7424 medicine is refilled Amitriptyline (Elavil®): • If you think there has been an Visit our website at: Important Patient Information www.urmc.rochester.edu/medicine/ - overdose, call your poison control general-medicine/patientcare/ center or get medical care right away What does amitriptyline (Elavil®) do? What side effects could occur with amitriptyline What are some things that I need to be aware of when • It belongs to a class of medications called tricyclic (Elavil®)? taking amitriptyline (Elavil®)? antidepressants (TCAs). It works by increasing the • Hard stools (constipation) • Tell your doctor or pharmacist if you are allergic to amitriptyline, any other medicines, foods, or substances amounts of certain natural substances in the brain that • Dizziness, feeling sleepy are needed -

HALDOL Decanoate 50 (Haloperidol)
HALDOL® Decanoate 50 (haloperidol) HALDOL® Decanoate 100 (haloperidol) For IM Injection Only WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. HALDOL Decanoate is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS). DESCRIPTION Haloperidol decanoate is the decanoate ester of the butyrophenone, HALDOL (haloperidol). It has a markedly extended duration of effect. It is available in sesame oil in sterile form for intramuscular (IM) injection. The structural formula of haloperidol decanoate, 4-(4-chlorophenyl)-1-[4-(4-fluorophenyl)-4-oxobutyl]-4 piperidinyl decanoate, is: Haloperidol decanoate is almost insoluble in water (0.01 mg/mL), but is soluble in most organic solvents. -

Schizophrenia Paper
The new england journal of medicine review article drug therapy Alastair J.J. Wood, M.D., Editor Schizophrenia Robert Freedman, M.D. From the Institute for Children’s Mental chizophrenia is a chronic, debilitating psychotic mental dis- Disorders, University of Colorado and the order that affects about 1 percent of people. A new generation of medications Veterans Affairs Medical Center, Denver. s Address reprint requests to Dr. Freedman and recent developments in neuropathology, brain imaging, and molecular ge- at the Department of Psychiatry, C-268-71, netics have led to a greater understanding of the pathophysiology of schizophrenia and University of Colorado Health Sciences to improved treatment. Nonetheless, it remains an enigmatic illness that places a sub- Center, Denver CO 80262, or at robert. [email protected]. stantial burden on patients, their families, and society. N Engl J Med 2003;349:1738-49. clinical characteristics Copyright © 2003 Massachusetts Medical Society. Schizophrenia has varied and ominous symptoms that generally begin in late adoles- cence or early adulthood and usually continue throughout life.1 Most patients have a history of behavioral dysfunction — primarily social and learning difficulties.2 Diagnos- tic features of schizophrenia include auditory hallucinations (generally voices that con- verse with or about the patient) and delusions (often the paranoid belief that external forces are conspiring against the patient). Patients may have some insight that the voices are internal thoughts and that the delusions cannot possibly be true, but these phenom- ena remain persistent and troubling. In addition to these overt psychotic, or “positive,” symptoms, various deficits, or “negative” symptoms, occur, including an inability to pay attention, the loss of a sense of pleasure, the loss of will or drive, disorganization or im- poverishment of thoughts and speech, flattening of affect, and social withdrawal (Ta- ble 1). -

Natural Psychoplastogens As Antidepressant Agents
molecules Review Natural Psychoplastogens As Antidepressant Agents Jakub Benko 1,2,* and Stanislava Vranková 1 1 Center of Experimental Medicine, Institute of Normal and Pathological Physiology, Slovak Academy of Sciences, 841 04 Bratislava, Slovakia; [email protected] 2 Faculty of Medicine, Comenius University, 813 72 Bratislava, Slovakia * Correspondence: [email protected]; Tel.: +421-948-437-895 Academic Editor: Olga Pecháˇnová Received: 31 December 2019; Accepted: 2 March 2020; Published: 5 March 2020 Abstract: Increasing prevalence and burden of major depressive disorder presents an unavoidable problem for psychiatry. Existing antidepressants exert their effect only after several weeks of continuous treatment. In addition, their serious side effects and ineffectiveness in one-third of patients call for urgent action. Recent advances have given rise to the concept of psychoplastogens. These compounds are capable of fast structural and functional rearrangement of neural networks by targeting mechanisms previously implicated in the development of depression. Furthermore, evidence shows that they exert a potent acute and long-term positive effects, reaching beyond the treatment of psychiatric diseases. Several of them are naturally occurring compounds, such as psilocybin, N,N-dimethyltryptamine, and 7,8-dihydroxyflavone. Their pharmacology and effects in animal and human studies were discussed in this article. Keywords: depression; antidepressants; psychoplastogens; psychedelics; flavonoids 1. Introduction 1.1. Depression Depression is the most common and debilitating mental disease. Its prevalence and burden have been steadily rising in the past decades. For example, in 1990, the World Health Organization (WHO) projected that depression would increase from 4th to 2nd most frequent cause of world-wide disability by 2020 [1].