In-Depth Cholera Epidemiological Report for South Sudan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cholera in South Sudan Situation Report # 95 As at 23:59 Hours, 29 September to 5 October 2014
Republic of South Sudan Cholera in South Sudan Situation Report # 95 as at 23:59 Hours, 29 September to 5 October 2014 Situation Update As of 5 October 2014, a total of 6,139 cholera cases including 139 deaths (CFR 2%) had been reportedTable 1. Summary in South of Suda choleran as cases summarizedreported in in Juba Tables County 1 and, 23 2.April – 5 October 2014 New New New deaths Total cases Total Total admisions discharges Total Total cases Reporting Sites 29 Sept to currently facility community Total cases 29 Sept to 29 Sept to deaths discharged 5 Oct 2014 admitted deaths deaths 5 Oct 2014 5 Oct 2014 JTH CTC 0 0 0 0 16 0 16 1466 1482 Gurei CTC (changed to ORP) Closed 28 July 2 0 2 365 367 Tongping CTC 0 2 1 3 69 72 Closed August Jube 3/UN House CTC Closed August 0 0 0 0 97 97 Nyakuron West CTC Closed 15 July 0 0 0 18 18 Gumbo CTC Closed 5 July 0 0 0 48 48 Nyakuron ORP Closed 5 July 0 0 0 20 20 Munuki ORP Closed 5 July 0 0 0 8 8 Gumbo ORP Closed 15 July 0 3 3 67 70 Pager PHCU 0 0 0 0 1 5 6 42 48 Other sites 0 0 0 1 15 16 1 17 Total 0 0 0 0 22 24 46 2201 2247 N.B. To prevent double counting of patients, transferred cases from ORPs to CTCs are not counted in the ORPs. Table 2: Summary of cholera cases reported outside Juba County, 23 April – 5 October 2014 New New New Total cases Total Total admisions discharges deaths Total Total cases Total States Reporting Sites currently facility community 29 Sept to 29 Sept to 29 Sep to deaths discharged cases admitted deaths deaths 5 Oct 2014 5 Oct 2014 5 Oct 14 Kajo-Keji civil hospital 0 0 0 0 -

Ss 9303 Ee Kapoeta North Cou
SOUTH SUDAN Kapoeta North County reference map SUDAN Pibor JONGLEI ETHIOPIA CAR DRC KENYA UGANDA EASTERN EQUATORIA Kenyi Lafon Kapoeta East Akitukomoi Kangitabok Lomokori Kapoeta North Ngigalingatun Kangibun Kalopedet Lokidangoai Nomogonjet Nawitapal Mogos Chokagiling Lorutuk Lokoges Nakwa Owetiani Nawabei Natatur Kamaliato Kanyowokol Karibungura Lokale Nagira Belengtobok Tuliabok Lokorechoke Kadapangolol Akoribok Nakwaparich Kalobeliang Wana Kachinga Lomus Lotiakara Pucwa Lopetet Nawao Lokorilam Naduket Tingayta Lodomei Kibak Nakatiti International boundary Nakapangiteng Napusiret Napulak State boundary Loriwo County boundary Kochoto Naminitotit Parpar Undetermined boundary Napusireit Nakwamoru Abyei region Kotak Kasotongor Napochorege Katiakin Nawayareng Riwoto Lokorumor Country capital Nangoletire Lokualem Lumeyen Logerain Lomidila Takankim Lobei Administrative centre/County capital Lokwamor Nacukut Naronyi Nakoret Lotiekar Namukeris Principal town Napotit Naoyatir Nakore Napureit Secondary town Lokwamiro Narubui Barach Lolepon Lotiri Paima Village Loregai Narongyet Lochuloit Kabuni Primary road Kudule Locheler Napusiria Napotpot Secondary road Nacholobo Tertiary road Budi Idong Main river Kapoeta South 0 5 10 km The administrative boundaries and names shown and the designations used on this map do not imply official endorsement or acceptance by the United Nations. Final boundary between the Republic of Sudan and the Republic of South Sudan has not yet been determined. Final status of Abyei area is not yet determined. Created: March 2020 | Code: SS-9303 | Sources: OCHA, SSNBS | Feedback: [email protected] | unocha.org/south-sudan | reliefweb.int/country/ssd | southsudan.humanitarianresponse.info . -

The Black Christs of the Black Christs of by J. Penn De
The Black Christs of Africa A Bible of Poems By J. Penn de Ngong Above all, I am not concerned with Poetry. My subject is War, and the pity of War. The Poetry is in the pity. Wilfred Owen, British Poet Poem 22 petition for partition We, the auto-government of the Republic of Ruralia, Voicing the will of the democratic public of Ruralia, Are writing to your Theocratic Union of Urbania. Our grievances are on the following discontentment: Firstly, your purely autocratic Government of Urbania, Has solely dishonoured and condemned the document That we all signed – and codenamed – “Bible of Peace”. You’ve violated its gospel, the cause of our fatal disagreement; Wealth: You’re feeding our autonomous nation with ration apiece. In your annual tour, compare our city – Metropollutant – of Ruralia With its posh sister city of Urbania, proudly dubbed Metropolitania. All our resources, on our watching, are consumed up in Urbania. Our intellectuals and workforce are abundant but redundant. Henceforth, right here, we demarcate to be independent! You are busy strategizing to turn Ruralia into Somalia: Yourselves landlords, creating warlords, tribal militia, And bribing our politicians to speak out your voice, And turning our villages into large ghettos of slum, And our own towns into large cities of Islam. With these experiences, we’ve no choice, But t’ ask, demand, fight... for our voice. They oft’ say the end justifies the means, We, Ruralians, must reform all our ruins; The first option: thru the ballot, Last action: bullet! J. Penn de Ngong (John Ngong Alwong Alith as known in his family) came into this world on a day nobody knows. -

South Sudan Village Assessment Survey
IOM DISPLACEMENT TRACKING MATRIX VILLAGE ASSESSMENT SURVEY SOUTH SUD AN IOM DISPLACEMENT TRACKING MATRIX SOUTH SUDAN SOUTH SUDAN VILLAGE ASSESSMENT SURVEY DATA COLLECTION: August-November 2019 COUNTIES: Bor South, Rubkona, Wau THEMATIC AREAS: Shelter and Land Ownership, Access and Communications, Livelihoods, Markets, Food Security and Coping Strategies, Health, WASH, Education, Protection 1 IOM DISPLACEMENT TRACKING MATRIX VILLAGE ASSESSMENT SURVEY SOUTH SUD AN CONTENTS RUBKONA COUNTY OVERVIEW 15 DISPLACEMENT DYNAMICS 15 RETURN PATTERNS 15 PAYAM CONTEXTUAL INFORMATION 16 KEY FINDINGS 17 Shelter and Land Ownership 17 EXECUTIVE SUMMARY 4 Access and Communications 17 LIST OF ACRONYMS 3 Markets, Food Security and Coping Strategies 17 EXECUTIVE SUMMARY 4 Livelihoods 18 BACKROUND 6 Health 19 WASH 19 METHODOLOGY 6 Education 20 LIMITATIONS 7 Protection 20 WAU COUNTY OVERVIEW 8 BOR SOUTH COUNTY OVERVIEW 21 DISPLACEMENT DYNAMICS 8 RETURN PATTERNS 8 DISPLACEMENT DYNAMICS 21 PAYAM CONTEXTUAL INFORMATION 9 RETURN PATTERNS 21 KEY FINDINGS 10 PAYAM CONTEXTUAL INFORMATION 22 KEY FINDINGS 23 Shelter and Land Ownership 10 Access and Communications 10 Shelter and Land Ownership 23 Markets, Food Security and Coping Strategies 10 Access and Communications 23 Livelihoods 11 Markets, Food Security and Coping Strategies 23 Health 12 Livelihoods 24 WASH 13 Health 25 Protection 13 Education 26 Education 14 WASH 27 Protection 27 2 3 IOM DISPLACEMENT TRACKING MATRIX VILLAGE ASSESSMENT SURVEY SOUTH SUD AN LIST OF ACRONYMS AIDS: Acquired Immunodeficiency Syndrome -

The Greater Pibor Administrative Area
35 Real but Fragile: The Greater Pibor Administrative Area By Claudio Todisco Copyright Published in Switzerland by the Small Arms Survey © Small Arms Survey, Graduate Institute of International and Development Studies, Geneva 2015 First published in March 2015 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without prior permission in writing of the Small Arms Survey, or as expressly permitted by law, or under terms agreed with the appropriate reprographics rights organi- zation. Enquiries concerning reproduction outside the scope of the above should be sent to the Publications Manager, Small Arms Survey, at the address below. Small Arms Survey Graduate Institute of International and Development Studies Maison de la Paix, Chemin Eugène-Rigot 2E, 1202 Geneva, Switzerland Series editor: Emile LeBrun Copy-edited by Alex Potter ([email protected]) Proofread by Donald Strachan ([email protected]) Cartography by Jillian Luff (www.mapgrafix.com) Typeset in Optima and Palatino by Rick Jones ([email protected]) Printed by nbmedia in Geneva, Switzerland ISBN 978-2-940548-09-5 2 Small Arms Survey HSBA Working Paper 35 Contents List of abbreviations and acronyms .................................................................................................................................... 4 I. Introduction and key findings .............................................................................................................................................. -
LC SS 706 A1 EEQ 20130301.Pdf
pp p ! ! p ! p (! ! !( 32°0'0"E 33°0'0"E 34°0'0"E 35°0'0"E Gwalla Awan KolnyangAluk Katanich Titong Munini Beru ! R . K Wowa ang en Logoda N Rigl Chilimun N " " 0 0 p' Bor South County ' 0 Pibor County Lowelli Katchikan River Bellel Kichepo 0 ° Maktiweng J O N G L E I ° 6 Kaigo 6 Lochiret R. Naro Kenamuke Swamp R Ngechele . S Neria u p Kanopir Natibok Kabalatigo i r i ( B Moru Kimod a Rongada h r Yebisak e g l- n Tombi J o e b b l Shogle e a l) Buka h C . Gwojo-Adung Kassangor R Baro ! E T H I O P I A Moru Kerri KURON Kuron Gigging p Bojo-Ajut Gemmaiza ! Karn Ethi Kerkeng Moru Ethi Nakadocwa Poko Wani Terekeka County Kobowen Swamp Borichadi Bokuna Poko Kassengo Selemani Pagar Nabwel Wani Mika Chabong Tukara C E N T R A L p River Nakua p Kenyi E Q U A T O R I A Moru Angbin Mukajo Gali Owiyabong Kursomba Lotimor Bulu Koli Kalaruz Awakot Katima Waha ! Akitukomoi River Gera Tumu Nanyangachor Nyabongi Napalap ! Namoropus Natilup Swamp ) it Wanyang Kangitabok Lomokori le Eyata Moru Kolinyagkopil il ! Terakeka ri Lozut Lomongole t iti o (! S L Magara p R. ( n Umm Gura Mwanyakapin a p y l Abuilingakine Lomareng Plateau a Dogora R Ngigalingatun k o . L Jelli L o p Rambo Djie Navi . Lokodopotok Nyaginei Kangeleng p R Biyara Nai A o Kworijik Kangibun Lomuleye Katirima t o Simsima Badigeru Swamp River Lokuja Losagam k Musha Lukwatuk Pass Doinyoro East p o p l Balala Legeri Buboli Kalopedet Pongo River Lokorowa Watha Peth Hills Bume E A S T E R N E Q U A T O R I A Lokidangoai Nawitapal Lopokori Lokomarukest Kolobeleng Yakara Dogatwan Nomogonjet Kagethi ! Mogos Bala Pool Lapon County Lotakawa Kanyabu Moru Ethi Donyiro West Donyiro Cliff Kedowa Kothokan a l l i Chokagiling t Karakamuge o Mangalla Bwoda L Mediket Kaliapus Nyangatom !( . -
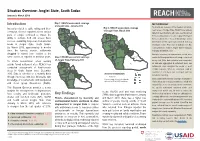
Jonglei State, South Sudan Introduction Key Findings
Situation Overview: Jonglei State, South Sudan January to March 2019 Introduction Map 1: REACH assessment coverage METHODOLOGY of Jonglei State, January 2019 To provide an overview of the situation in hard-to- Insecurity related to cattle raiding and inter- Map 3: REACH assessment coverage of Jonglei State, March 2019 reach areas of Jonglei State, REACH uses primary communal violence reported across various data from key informants who have recently arrived parts of Jonglei continued to impact the from, recently visited, or receive regular information ability to cultivate food and access basic Fangak Canal/Pigi from a settlement or “Area of Knowledge” (AoK). services, sustaining large-scale humanitarian Nyirol Information for this report was collected from key needs in Jonglei State, South Sudan. Ayod informants in Bor Protection of Civilians site, Bor By March 2019, approximately 5 months Town and Akobo Town in Jonglei State in January, since the harvest season, settlements February and March 2019. Akobo Duk Uror struggled to extend food rations to the In-depth interviews on humanitarian needs were Twic Pochalla same extent as reported in previous years. Map 2: REACH assessment coverage East conducted throughout the month using a structured of Jonglei State, February 2019 survey tool. After data collection was completed, To inform humanitarian actors working Bor South all data was aggregated at settlement level, and outside formal settlement sites, REACH has Pibor settlements were assigned the modal or most conducted assessments of hard-to-reach credible response. When no consensus could be areas in South Sudan since December found for a settlement, that settlement was not Assessed settlements 2015. -

UNICEF South Sudan Humanitarian Situation August 2019
UNICEF SOUTH SUDAN SITUATION REPORT August 2019 South Sudan Humanitarian Lunch time at Juba Na Bari primary school in Juba. School meals provide at least one nutritious meal a Situation Report day for the children and give them the energy they need to concentrate. Photo: UNICEF South Sudan/De La Guardia AUGUST 2019: SOUTH SUDAN SITREP #135 SITUATION IN NUMBERS Highlights •UNICEF and implementing partners distributed essential educational 1.83 million supplies (exercise books, pens, pencils, rulers, school bags, hygiene Internally displaced persons (IDPs) supplies) to 9,326 learners (including 3,989 girls) in 13 schools in Eastern (OCHA South Sudan Humanitarian Snapshot, July 2019) Equatoria. In Yambio teaching and learning materials, including students’ kits and other supplies were distributed to 6,380 children (3,334 girls; 3046 boys). 2.32 million South Sudanese refugees in •Additionally, all 32 released children from opposition forces in July 2019 neighbouring countries have begun receiving reintegration services in their communities through (UNHCR Regional Portal, South Sudan Situation coordinated case management services. 31 August 2019) •In 2019, no suspected cases of cholera have been reported. Cholera prevention activities continue to mitigate the risk of cholera outbreaks in 6.35 million hotspots. UNICEF and partners have reviewed the cholera preparedness South Sudanese facing acute food plan for 2019 in readiness for expected events in the country. insecurity or worse (August 2019 Projection, Integrated Food Security Phase Classification) -
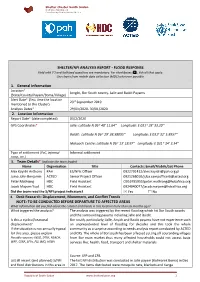
SHELTER/NFI ANALYSIS REPORT - FLOOD RESPONSE Field with (*) and Italicized Questions Are Mandatory
Shelter Cluster South Sudan sheltersouthsudan.org Coordinating Humanitarian Shelter SHELTER/NFI ANALYSIS REPORT - FLOOD RESPONSE Field with (*) and italicized questions are mandatory. For checkboxes (☐), tick all that apply. Use charts from mobile data collection (MDC) wherever possible. 1. General Information Location* Jonglei, Bor South county- Jalle and Baidit Payams (State/County/Payam/Boma/Village) Alert Date* (first time the location 23rd September 2019 mentioned to the Cluster) Analysis Dates* 29/01/2020- 30/01/2020 2. Location Information Report Date* (date completed) 03/2/2020 GPS Coordinates* Jalle: Latitude N 06 o 40’ 11.64’’ Longitude: E 031 o 28’ 33.20’’ Baidit: Latitude N 06 o 29’ 38.58095’’ Longitude: E 031o 32’ 5.8957’’ Makuach Centre: Latitude N 06 o 13’ 18.97’’ Longitude: E 031 o 34’ 3.34’’ Type of settlement (PoC, informal Informal settlement camp, etc.) 3. Team Details* (Indicate the team leader) Name Organisation Title Contacts: Email/Mobile/Sat Phone Alex Kayidri Anthony PAH ES/NFIs Officer 0922791412/[email protected] Juma John Benjamin ACTED Senior Project Officer 0921268010/[email protected] Peter Mathiang HDC Field Assistant O916795955/[email protected] Jacob Mayom Yuot HDC Field Assistant 0924040077/[email protected] Did the team read the S/NFI project indicators? ☒ Yes ☐ No 4. Desk Research: Displacement, Movement, and Conflict Trends NOTE: TO BE CONDUCTED BEFORE DEPARTURE TO AFFECTED AREAS What information did you find about the context and trends in this location more than six months ago? What triggered the analysis? The analysis was triggered by the recent flooding which hit Bor South county and the surrounding payams including Jalle and Baidit. -

LOCATION: WFP Tukul Conference Room DATE: 25 September, 2014
SOUTH SUDAN FSL JONGLEI COORDINATION – MEETING MINUTES LOCATION: WFP Tukul Conference Room DATE: 25 September, 2014 CHAIR: George Mvula, FSL Area Cluster Coordinator AGENDA: The following was the agenda of the meeting: 1. Introductions; 2. Review and endorsing previous minutes; 3. Recap of the FSL Partners meeting; 4. Key challenges to humanitarian response interventions in Jonglei; 5. Partners’ presentation of county level information (planned versus actual) and where; 6. Presentation by SAADO on elevated Hunger Situation in Twic East; 7. Presentation by Oxfam Intermon on Urban Livelihood assessment in Bor Town; 8. Review of gaps per county; 9. Briefing on the IPC report September 2014 and implications on response programming; 10. AOB Monthly Updates from Partners Church and Development Key achievements in the month of September: Trained 150 women headed households on construction and usage of energy efficient stoves (Rocket Lorena model). Trained 300 fish folks (277 male, 03 female) on fish processing and preservation, this also involved construction of improved fish drying ovens using local materials. 60 households trained on village savings and loans association methodology and equipping them with startup kits. 400 beneficiaries from Bor Town registered and verified for unconditional cash transfer. http://foodsecuritycluster.net/operations/south-sudan SOUTH SUDAN FSL JONGLEI COORDINATION – MEETING MINUTES Plans for October 600 households in Bor targeted to receive ganny bags and assorted tools for construction of secondary dykes around their homesteads Cash transfer to verified 400 vulnerable households Post cash transfer assessment in Bor main market and other markets in the Payam. Catholic Relief Services (Jonglei Food Security Programme) General Food Distribution: CRS has been doing general food distributions in Bor and Twic East. -

Cholera in South Sudan Situation Report # 93 As at 23:59 Hours, 15-21 September 2014
Republic of South Sudan Cholera in South Sudan Situation Report # 93 as at 23:59 Hours, 15-21 September 2014 Situation Update As of 21 September 2014, a total of 6,128 cholera cases including 139 deaths (CFR 2.27%) had beenTable reported1. Summary in of South cholera Sudan cases asreported summarized in Juba in County Tables, 23 1 April and –2.21 September 2014 New New New deaths Total cases Total Total admisions discharges Total Total cases Reporting Sites 15-21 Sept currently facility community Total cases 15-21 Sept 15-21 Sept deaths discharged 2014 admitted deaths deaths 2014 2014 JTH CTC 3 3 0 0 16 0 16 1455 1479 Gurei CTC (changed to ORP) Closed 28 July 2 0 2 365 367 Tongping CTC 0 2 1 3 69 72 Closed August Jube 3/UN House CTC Closed August 0 0 0 0 97 97 Nyakuron West CTC Closed 15 July 0 0 0 18 18 Gumbo CTC Closed 5 July 0 0 0 48 48 Nyakuron ORP Closed 5 July 0 0 0 20 20 Munuki ORP Closed 5 July 0 0 0 8 8 Gumbo ORP Closed 15 July 0 3 3 67 70 Pager PHCU 1 1 0 0 1 5 6 42 48 Other sites 0 0 0 1 15 16 1 17 Total 4 4 0 0 22 24 46 2190 2244 N.B. To prevent double counting of patients, transferred cases from ORPs to CTCs are not counted in the ORPs. Table 2: Summary of cholera cases reported outside Juba County, 23 April –21 September 2014 New New New Total cases Total Total admisions discharges deaths Total Total cases Total States Reporting Sites currently facility community 15-21 Sept 15-21 Sept 15-21 deaths discharged cases admitted deaths deaths 2014 2014 Sept 2014 Kajo-Keji civil hospital 0 0 0 0 3 4 7 86 93 CES Yei Hospital -- 0 -
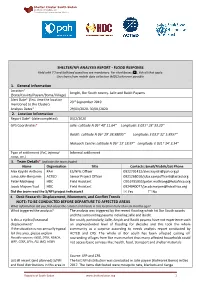
SHELTER/NFI ANALYSIS REPORT - FLOOD RESPONSE Field with (*) and Italicized Questions Are Mandatory
Shelter Cluster South Sudan sheltersouthsudan.org Coordinating Humanitarian Shelter SHELTER/NFI ANALYSIS REPORT - FLOOD RESPONSE Field with (*) and italicized questions are mandatory. For checkboxes (☐), tick all that apply. Use charts from mobile data collection (MDC) wherever possible. 1. General Information Location* Jonglei, Bor South county- Jalle and Baidit Payams (State/County/Payam/Boma/Village) Alert Date* (first time the location 23rd September 2019 mentioned to the Cluster) Analysis Dates* 29/01/2020- 30/01/2020 2. Location Information Report Date* (date completed) 03/2/2020 GPS Coordinates* Jalle: Latitude N 06 o 40’ 11.64’’ Longitude: E 031 o 28’ 33.20’’ Baidit: Latitude N 06 o 29’ 38.58095’’ Longitude: E 031o 32’ 5.8957’’ Makuach Centre: Latitude N 06 o 13’ 18.97’’ Longitude: E 031 o 34’ 3.34’’ Type of settlement (PoC, informal Informal settlement camp, etc.) 3. Team Details* (Indicate the team leader) Name Organisation Title Contacts: Email/Mobile/Sat Phone Alex Kayidri Anthony PAH ES/NFIs Officer 0922791412/[email protected] Juma John Benjamin ACTED Senior Project Officer 0921268010/[email protected] Peter Mathiang HDC Field Assistant O916795955/[email protected] Jacob Mayom Yuot HDC Field Assistant 0924040077/[email protected] Did the team read the S/NFI project indicators? ☒ Yes ☐ No 4. Desk Research: Displacement, Movement, and Conflict Trends NOTE: TO BE CONDUCTED BEFORE DEPARTURE TO AFFECTED AREAS What information did you find about the context and trends in this location more than six months ago? What triggered the analysis? The analysis was triggered by the recent flooding which hit Bor South county and the surrounding payams including Jalle and Baidit.