Complete Blood Count.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Markers of Carotid Atherosclerosis in Type 2 Diabetes Mellitus? Riya M Waghale, Rajashree Sanjay Khot, Prashant P Joshi Impact of Smoking and Nicotine Addiction
2020, Vol. 9, No. 2 ISSN 2450–7458 Platelet volume indices: markers of carotid atherosclerosis in type 2 diabetes mellitus? Riya M Waghale, Rajashree Sanjay Khot, Prashant P Joshi Impact of smoking and nicotine addiction on HbA1c levels and diabetic microvascular complication Hüseyin Akkuzulu, Cenk Aypak, Ayşe Özdemir, Süleyman Görpelioğlu Sugary beverages consumption and latent autoimmune diabetes in adults: systematic review and meta-analysis Ahmed Mahmoud El-Malky, Ramachandra G Naik, Azza A Elnouman The effect of low dose glargine U 300 on uncontrolled type 2 diabetes mellitus. An observational study in Indian patients Asis Mitra, Saswati Ray, Sushma Jayan Coffee in the diet and prevention of diabetes Regina Wierzejska Editor-in-Chief Scientific Board dr hab. n. med. Leszek Czupryniak, prof. nadzw. (Poland) prof. Antionio Ceriello (Spain) prof. dr hab. n. med. Edward Franek (Poland) Deputy Editor-in-Chief prof. dr hab. n. med. Władysław Grzeszczak (Poland) prof. dr hab. n. med. Wojciech Młynarski (Poland) prof. Martin Haluzík (Czech Republic) prof. dr hab. n. med. Krzysztof Strojek (Poland) prof. dr hab. n. med. Przemysława Jarosz-Chobot (Poland) prof. Nebojsa Lalic (Serbia and Montenegro) Editorial Board prof. Pierre Lefebvre (Belgium) prof. dr hab. n. med. Katarzyna Cypryk (Poland) prof. dr hab. n. med. Maciej Małecki (Poland) prof. Larisa Danilova (Belarus) prof. dr hab. n. med. Andrzej Milewicz (Poland) prof. dr hab. n. med. Janusz Gumprecht (Poland) prof. dr hab. n. med. Dariusz Moczulski (Poland) prof. dr hab. n. med. Krzysztof Narkiewicz (Poland) prof. dr hab. n. med. Irina Kowalska (Poland) dr Katherine Owen (United Kingdom) prof. dr hab. n. med. -

Interpreting Your Child's Lab Results
www.ComplexChild.com Interpreting Your Child’s Lab Results When you get a list of labs back from your doctor or hospital, your eye is drawn immediately to the starred or highlighted results that came back abnormal. Knowing that any of your child’s results have come back abnormal can be disconcerting. Much of the time, however, there is no need to worry. But how do you know when abnormal results indicate a little problem, a big problem, or not a problem at all? Reference Ranges The first thing you need to do is look at the reference ranges that are given along with the results. Each lab has its own equipment that is calibrated uniquely, and results vary depending on the lab. While most tests have similar reference ranges from lab to lab, there are some, such as the test for Lipase, that use different testing systems with very different reference ranges. Results from one lab may not be equivalent to results at another lab. The Slightly High or Low Result In many cases, the abnormal result is ever so slightly high or low. Since reference ranges usually represent two standard deviations above or below the average mean value in healthy people, it is still normal for about five percent of the population to be ever so slightly higher or lower than the reference range. Keeping this in mind, a slightly low or high result is rarely concerning. Tests may also be slightly off due to illness, food or drink consumed, or many other factors. Many doctors will advise repeating the tests at a later time to see if the value has normalized, remains the same, or is trending upward or downward. -

Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant
Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease 1 Produced by St. Jude Children’s Research Hospital Departments of Hematology, Patient Education, and Biomedical Communications. Funds were provided by St. Jude Children’s Research Hospital, ALSAC, and a grant from the Plough Foundation. This document is not intended to take the place of the care and attention of your personal physician. Our goal is to promote active participation in your care and treatment by providing information and education. Questions about individual health concerns or specifi c treatment options should be discussed with your physician. For more general information on sickle cell disease, please visit our Web site at www.stjude.org/sicklecell. Copyright © 2009 St. Jude Children’s Research Hospital How did bone marrow (stem cell) transplants begin for children with sickle cell disease? Bone marrow (stem cell) transplants have been used for the treatment and cure of a variety of cancers, immune system diseases, and blood diseases for many years. Doctors in the United States and other countries have developed studies to treat children who have severe sickle cell disease with bone marrow (stem cell) transplants. How does a bone marrow (stem cell) transplant work? 2 In a person with sickle cell disease, the bone marrow produces red blood cells that contain hemoglobin S. This leads to the complications of sickle cell disease. • To prepare for a bone marrow (stem cell) transplant, strong medicines, called chemotherapy, are used to weaken or destroy the patient’s own bone marrow, stem cells, and infection fi ghting system. -
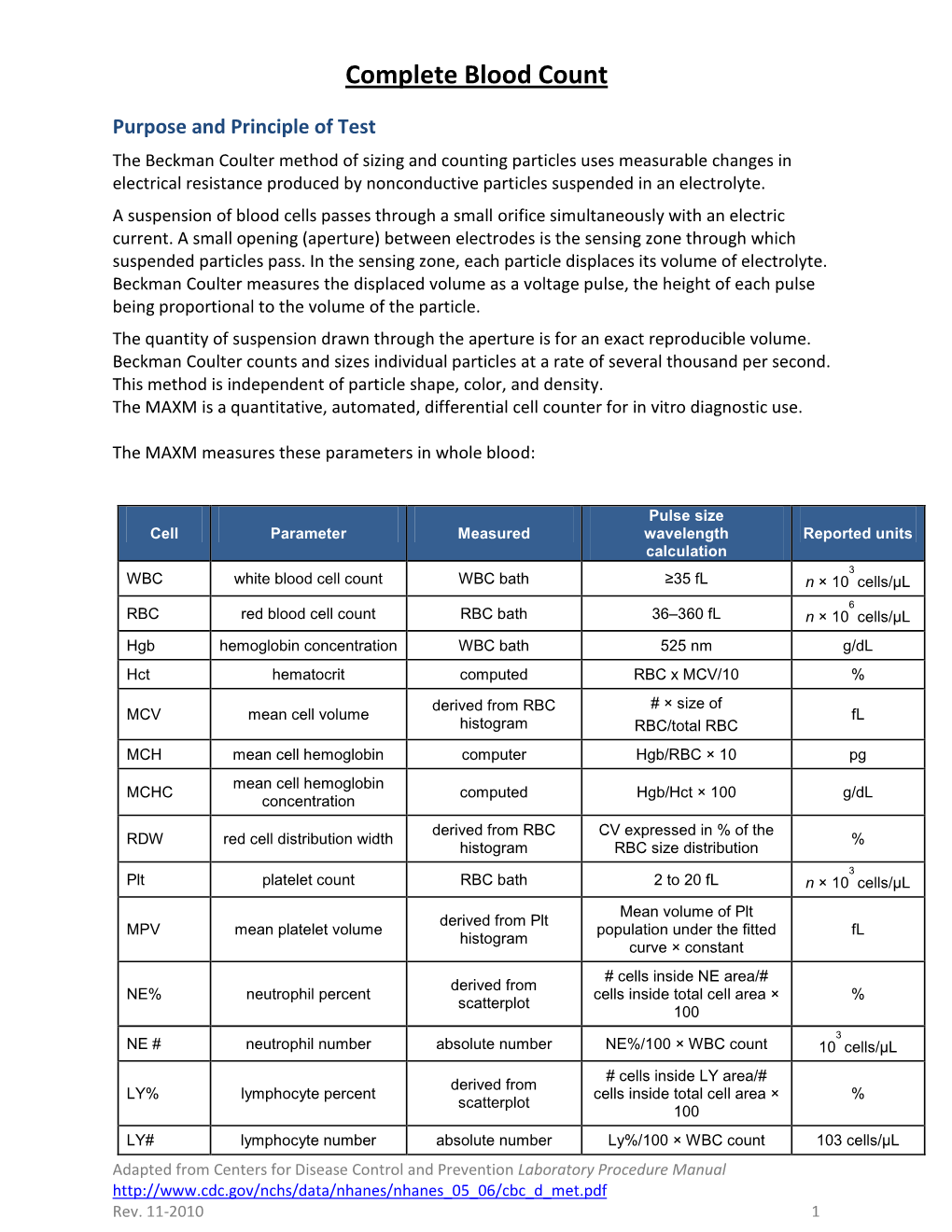
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -
Myelodysplastic Syndromes Overview and Types
cancer.org | 1.800.227.2345 About Myelodysplastic Syndromes Overview and Types If you have been diagnosed with a myelodysplastic syndrome or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Are Myelodysplastic Syndromes? ● Types of Myelodysplastic Syndromes Research and Statistics See the latest estimates for new cases of myelodysplastic syndromes in the US and what research is currently being done. ● Key Statistics for Myelodysplastic Syndromes ● What's New in Myelodysplastic Syndrome Research? What Are Myelodysplastic Syndromes? Myelodysplastic syndromes (MDS) are conditions that can occur when the blood- forming cells in the bone marrow become abnormal. This leads to low numbers of one or more types of blood cells. MDS is considered a type of cancer1. Normal bone marrow 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Bone marrow is found in the middle of certain bones. It is made up of blood-forming cells, fat cells, and supporting tissues. A small fraction of the blood-forming cells are blood stem cells. Stem cells are needed to make new blood cells. There are 3 main types of blood cells: red blood cells, white blood cells, and platelets. Red blood cells pick up oxygen in the lungs and carry it to the rest of the body. These cells also bring carbon dioxide back to the lungs. Having too few red blood cells is called anemia. It can make a person feel tired and weak and look pale. Severe anemia can cause shortness of breath. White blood cells (also known as leukocytes) are important in defending the body against infection. -
Understanding Your Blood Test Lab Results
Understanding Your Blood Test Lab Results A comprehensive "Health Panel" has been designed specifically to screen for general abnormalities in the blood. This panel includes: General Chemistry Screen or (SMAC), Complete Blood Count or (CBC), and Lipid examination. A 12 hour fast from all food and drink (water is allowed) is required to facilitate accurate results for some of the tests in this panel. Below, is a breakdown of all the components and a brief explanation of each test. Abnormal results do not necessarily indicate the presence of disease. However, it is very important that these results are interpreted by your doctor so that he/she can accurately interpret the findings in conjunction with your medical history and order any follow-up testing if needed. The Bernards Township Health Department and the testing laboratory cannot interpret these results for you. You must speak to your doctor! 262 South Finley Avenue Basking Ridge, NJ 07920 www.bernardshealth.org Phone: 908-204-2520 Fax: 908-204-3075 1 Chemistry Screen Components Albumin: A major protein of the blood, albumin plays an important role in maintaining the osmotic pressure spleen or water in the blood vessels. It is made in the liver and is an indicator of liver disease and nutritional status. A/G Ratio: A calculated ratio of the levels of Albumin and Globulin, 2 serum proteins. Low A/G ratios can be associated with certain liver diseases, kidney disease, myeloma and other disorders. ALT: Also know as SGPT, ALT is an enzyme produced by the liver and is useful in detecting liver disorders. -
Evaluation of Complete Blood Count Parameters for Diagnosis In
Original Investigation / Özgün Araştırma DOI: 10.5578/ced.68886 • J Pediatr Inf 2020;14(2):e55-e62 Evaluation of Complete Blood Count Parameters for Diagnosis in Children with Sepsis in the Pediatric Intensive Care Unit Pediatrik Yoğun Bakım Ünitesinde Sepsisli Çocuklarda Tanı İçin Tam Kan Sayımı Parametrelerinin Değerlendirilmesi Fatih Aygün1(İD), Cansu Durak1(İD), Fatih Varol1(İD), Haluk Çokuğraş2(İD), Yıldız Camcıoğlu2(İD), Halit Çam1(İD) 1 Department of Pediatric Intensive Care, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey 2 Department of Pediatric Infectious Diseases, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey Cite this article as: Aygün F, Durak C, Varol F, Çokuğraş H, Camcıoğlu Y, Çam H. Evaluation of complete blood count parameters for diagnosis in children with sepsis in the pediatric intensive care unit. J Pediatr Inf 2020;14(2):e55-e62. Abstract Öz Objective: Early diagnosis of sepsis is important for effective treatment Giriş: Erken tanı sepsiste etkili tedavi ve iyi prognoz için önemlidir. C-re- and improved prognosis. C-reactive protein (CRP) and procalcitonin aktif protein (CRP) ve prokalsitonin (PKT) sepsiste en sık kullanılan bi- (PCT) are the most commonly used biomarkers for sepsis. However, their yobelirteçlerdir. Fakat rutinde kullanımı maliyet etkin değildir. Tam kan routine usage is not cost-effective. Complete Blood Count (CBC) param- sayımı (TKS) parametrelerinden eritrosit dağılım genişliği (EDG), nötrofil eters including red cell distribution width (RDW), neutrophil to lympho- lenfosit oranı (NLO), trombosit lenfosit oranı (TLO), ortalama trombosit cyte ratios (NLR), platelet to lymphocyte ratios (PLR), mean platelet vol- hacmi (OTH) basit ve kolay olarak hesaplanmaktadır. Bu çalışmanın ama- ume (MPV), and hemoglobin are simple and easily calculated. -

Your Blood Cells
Page 1 of 2 Original Date The Johns Hopkins Hospital Patient Information 12/00 Oncology ReviseD/ RevieweD 6/14 Your Blood Cells Where are Blood cells are made in the bone marrow. The bone marrow blood cells is a liquid that looks like blood. It is found in several places of made? the body, such as your hips, chest bone and the middle part of your arm and leg bones. What types of • The three main types of blood cells are the red blood cells, blood cells do the white blood cells and the platelets. I have? • Red blood cells carry oxygen to all parts of the body. The normal hematocrit (or percentage of red blood cells in the blood) is 41-53%. Anemia means low red blood cells. • White blood cells fight infection. The normal white blood cell count is 4.5-11 (K/cu mm). The most important white blood cell to fight infection is the neutrophil. Forty to seventy percent (40-70%) of your white blood cells should be neutrophils. Neutropenia means your neutrophils are low, or less than 40%. • Platelets help your blood to clot and stop bleeding. The normal platelet count is 150-350 (K/cu mm). Thrombocytopenia means low platelets. How do you Your blood cells are measured by a test called the Complete measure my Blood Count (CBC) or Heme 8/Diff. You may want to keep track blood cells? of your blood counts on the back of this sheet. What When your blood counts are low, you may become anemic, get happens infections and bleed or bruise easier. -

Automatic Blood Cell and CRP Counter with Three-Part Differential
FEATURE ARTICLE Automatic Blood Cell and CRP Counter with Three-Part Differential Measurement of White Blood Cells The LC-170 CRP FEATURE ARTICLE Automatic Blood Cell and CRP Counter with Three-Part Differential Measurement of White Blood Cells, The LC-170 CRP Yasuo Yamao WBC, RBC, Hct Electrical impedance method Hgb CRP Cyanmethemoglobin method Latex immunoturbidmetry WBC (White blood cells) LYM% MON% GRA% CRP quantitative LC-170CRP (Lymphocyte %) (Monocyte %) (Granulocyte %) analysis LYM# MON# GRA# (C-reactive protein) (Lymphocyte No.) (Monocyte No.) (Granulocyte No.) RBC (Red blood cells) PLT (Platelets) Hgb(Hemoglobin) Pct (Plateletcrit) Hct (Hematocrit) MPV (Mean Platelet Volume) MCV (Mean Corpuscular Volume) PDW (Platelet Distribution Width) MCH (Mean Corpuscular Hemoglobin) MCHC (Mean Corpuscular Hemoglobin Concentration) RDW (Red Blood Cell Distribution Width) Example of results Abstract The LC-l70 CRP automatic blood cell and CRP counter, developed by Horiba, is capable of simultaneously measuring all 19 C-reactive protein (CRP) density parameters and counting red blood cells, platelets, and three types of white blood cell: lymphocytes, monocytes, and granulocytes. As clinicians demand ever-higher precision measurements, a need has developed for clinical test machines having excellent operational and cost performance. This compact machine should make a powerful tool for initial diagnosis of inflammatory and infectious diseases, especially at small- and mid-size medical institutions. 20 Technical Reports 1 Introduction 2 Measurement Principles To prevent an explosion of medical costs as Japanese The LC-170 CRP uses the electrical impedance method society ages and fewer children are born, the Ministry of to count blood cells, the cyanmethemoglobin method to Health, Labor, and Welfare is pursuing a thorough reform measure hemoglobin concentration, and latex of the medical insurance system, including “preventing immunoturbidimetry to measure CRP concentration. -

Complete Blood Count in Primary Care
Complete Blood Count in Primary Care bpac nz better medicine Editorial Team bpacnz Tony Fraser 10 George Street Professor Murray Tilyard PO Box 6032, Dunedin Clinical Advisory Group phone 03 477 5418 Dr Dave Colquhoun Michele Cray free fax 0800 bpac nz Dr Rosemary Ikram www.bpac.org.nz Dr Peter Jensen Dr Cam Kyle Dr Chris Leathart Dr Lynn McBain Associate Professor Jim Reid Dr David Reith Professor Murray Tilyard Programme Development Team Noni Allison Rachael Clarke Rebecca Didham Terry Ehau Peter Ellison Dr Malcolm Kendall-Smith Dr Anne Marie Tangney Dr Trevor Walker Dr Sharyn Willis Dave Woods Report Development Team Justine Broadley Todd Gillies Lana Johnson Web Gordon Smith Design Michael Crawford Management and Administration Kaye Baldwin Tony Fraser Kyla Letman Professor Murray Tilyard Distribution Zane Lindon Lyn Thomlinson Colleen Witchall All information is intended for use by competent health care professionals and should be utilised in conjunction with © May 2008 pertinent clinical data. Contents Key points/purpose 2 Introduction 2 Background ▪ Haematopoiesis - Cell development 3 ▪ Limitations of reference ranges for the CBC 4 ▪ Borderline abnormal results must be interpreted in clinical context 4 ▪ History and clinical examination 4 White Cells ▪ Neutrophils 5 ▪ Lymphocytes 9 ▪ Monocytes 11 ▪ Basophils 12 ▪ Eosinophils 12 ▪ Platelets 13 Haemoglobin and red cell indices ▪ Low haemoglobin 15 ▪ Microcytic anaemia 15 ▪ Normocytic anaemia 16 ▪ Macrocytic anaemia 17 ▪ High haemoglobin 17 ▪ Other red cell indices 18 Summary Table 19 Glossary 20 This resource is a consensus document, developed with haematology and general practice input. We would like to thank: Dr Liam Fernyhough, Haematologist, Canterbury Health Laboratories Dr Chris Leathart, GP, Christchurch Dr Edward Theakston, Haematologist, Diagnostic Medlab Ltd We would like to acknowledge their advice, expertise and valuable feedback on this document. -

Essential Thrombocythemia Facts No
Essential Thrombocythemia Facts No. 12 in a series providing the latest information for patients, caregivers and healthcare professionals www.LLS.org • Information Specialist: 800.955.4572 Introduction Highlights Essential thrombocythemia (ET) is one of several l Essential thrombocythemia (ET) is one of a related “myeloproliferative neoplasms” (MPNs), a group of closely group of blood cancers known as “myeloproliferative related blood cancers that share several features, notably the neoplasms” (MPNs) in which cells in the bone “clonal” overproduction of one or more blood cell lines. marrow that produce the blood cells develop and All clonal disorders begin with one or more changes function abnormally. (mutations) to the DNA in a single cell; the altered cells in l ET begins with one or more acquired changes the marrow and the blood are the offspring of that one (mutations) to the DNA of a single blood-forming mutant cell. Other MPNs include polycythemia vera and cell. This results in the overproduction of blood cells, myelofibrosis. especially platelets, in the bone marrow. The effects of ET result from uncontrolled blood cell l About half of individuals with ET have a mutation production, notably of platelets. Because the disease arises of the JAK2 (Janus kinase 2) gene. The role that this from a change to an early blood-forming cell that has the mutation plays in the development of the disease, capacity to form red cells, white cells and platelets, any and the potential implications for new treatments, combination of these three cell lines may be affected – and are being investigated. usually each cell line is affected to some degree. -

Neutrophils (A.K.A
Neutrophils (a.k.a. leukocyte, granulocyte, white blood cell, WBC) blood cells on a microscope slide showing the lobed nucleus of two neutrophils a 3-d drawing of a neutrophil This chart shows how blood cells are produced in the bone marrow from “stem cells” and how we organize them into groups. By Mikael Häggström The Mul(faceted Func(ons of Neutrophils Tanya N. Mayadas,1 Xavier Cullere,1 and Clifford A. Lowell2 “Neutrophils and neutrophil-like cells are the major pathogen-fighKng immune cells in organisms ranging from slime molds to mammals. Central to their funcKon is their ability to be recruited to sites of infecKon, to recognize and phagocytose (eang foreign objects like bacteria) microbes, and then to kill pathogens through a combinaon of cytotoxic mechanisms.” Form • average diameter of 12-15 micrometers (µm) in peripheral blood smears • in suspension, neutrophils have an average diameter of 8.85 µm • mulK-lobed shape nucleus • survive for only 8–12 h in the circulaon and up to 1–2 days in Kssues • Neutrophils will show increasing segmentaon (many segments of nucleus) as they mature. A normal neutrophil should have 3-5 segments. • Neutrophils account for approximately 50-70% of all white blood cells (leukocytes) Func(on • first line of host defense against a wide range of infecKous pathogens including bacteria, fungi, and protozoa • Neutrophils are generated at a rate of 1011 per day, which can increase to 1012 per day during bacterial infection. • Researchers once believed that neutrophils were present only during the most acKve phase of an infecKon, funcKoning as pathogen killers.