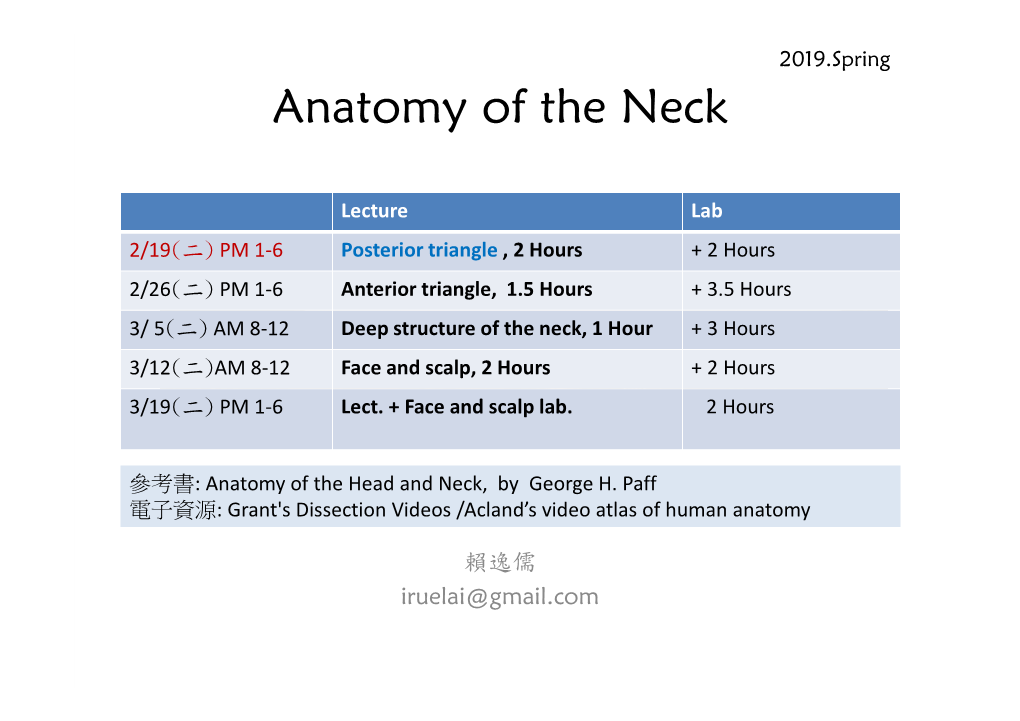
Anatomy of the Neck
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supraclavicular Artery Island Flap in Head and Neck Reconstruction
European Annals of Otorhinolaryngology, Head and Neck diseases 132 (2015) 291–294 View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Available online at ScienceDirect www.sciencedirect.com Technical note Supraclavicular artery island flap in head and neck reconstruction a b a,c a,∗,c S. Atallah , A. Guth , F. Chabolle , C.-A. Bach a Service de chirurgie ORL et cervico-faciale, hôpital Foch, 40 rue Worth, 92150 Suresnes, France b Service de radiologie, hôpital Foch, 40, rue Worth, 92150 Suresnes, France c Université de Versailles Saint-Quentin en Yvelines, UFR de médecine Paris Ouest Saint-Quentin-en-Yvelines, 78280 Guyancourt, France a r t i c l e i n f o a b s t r a c t Keywords: Due to the complex anatomy of the head and neck, a wide range of pedicled or free flaps must be available Supraclavicular artery island flap to ensure optimal reconstruction of the various defects resulting from cancer surgery. The supraclavi- Fasciocutaneous flap cular artery island flap is a fasciocutaneous flap harvested from the supraclavicular and deltoid regions. Head and neck cancer The blood supply of this flap is derived from the supraclavicular artery, a direct cutaneous branch of the Reconstructive surgery transverse cervical artery in 93% of cases or the supraclavicular artery in 7% of cases. The supraclavicular artery is located in a triangle delineated by the posterior border of the sternocleidomastoid muscle medi- ally, the external jugular vein posteriorly, and the median portion of the clavicle anteriorly. -

Superior Laryngeal Nerve Identification and Preservation in Thyroidectomy
ORIGINAL ARTICLE Superior Laryngeal Nerve Identification and Preservation in Thyroidectomy Michael Friedman, MD; Phillip LoSavio, BS; Hani Ibrahim, MD Background: Injury to the external branch of the su- recorded and compared on an annual basis for both be- perior laryngeal nerve (EBSLN) can result in detrimen- nign and malignant disease. Overall results were also com- tal voice changes, the severity of which varies according pared with those found in previous series identified to the voice demands of the patient. Variations in its ana- through a 50-year literature review. tomic patterns and in the rates of identification re- ported in the literature have discouraged thyroid sur- Results: The 3 anatomic variations of the distal aspect geons from routine exploration and identification of this of the EBSLN as it enters the cricothyroid were encoun- nerve. Inconsistent with the surgical principle of pres- tered and are described. The total identification rate over ervation of critical structures through identification, mod- the 20-year period was 900 (85.1%) of 1057 nerves. Op- ern-day thyroidectomy surgeons still avoid the EBSLN erations performed for benign disease were associated rather than identifying and preserving it. with higher identification rates (599 [86.1%] of 696) as opposed to those performed for malignant disease Objectives: To describe the anatomic variations of the (301 [83.4%] of 361). Operations performed in recent EBSLN, particularly at the junction of the inferior con- years have a higher identification rate (over 90%). strictor and cricothyroid muscles; to propose a system- atic approach to identification and preservation of this Conclusions: Understanding the 3 anatomic variations nerve; and to define the identification rate of this nerve of the distal portion of the EBSLN and its relation to the during thyroidectomy. -

Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch
411 Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch John Holder1 Five cases are reported of left subclavian steal syndrome associated with anomalous Eugene F. Binet2 origin of the left vertebral artery from the aortic arch. In all five instances blood flow at Bernard Thompson3 the origin of the left vertebral artery was in an antegrade direction contrary to that usually reported in this condition. The distal subclavian artery was supplied via an extensive collateral network of vessels connecting the vertebral artery to the thyro cervical trunk. If a significant stenosis or occlusion is present within the left subc lavi an artery proximal to the origin of the left vertebral artery, the direction of the bl ood fl ow within the vertebral artery will reverse toward the parent vessel (retrograde flow). This phenomenon occurs when a negative pressure gradient of 20-40 torr exists between the vertebral-basilar artery junction and th e vertebral-subc lavian artery junction [1-3]. We describe five cases of subclavian steal confirmed by angiography where a significant stenosis or occlusion of the left subclavian artery was demonstrated in association with anomalous origin of th e left vertebral artery directly from the aortic arch. In all five cases blood flow at the origin of the left vertebral artery was in an antegrade direction contrary to that more commonly reported in the subclavian steal syndrome. Materials and Methods The five patients were all 44- 58-year-old men. Three sought medical attention for symptoms specificall y related to th e left arm . -

7-Khyati Santram
J. Anat. Sciences, 24(2): Dec. 2016, 33-35 Case Report ANATOMICAL VARIATION OF THE TRAPEZIUS MUSCLE- A CASE REPORT Khayati Sant Ram*, Anjali Aggarwal*,Tulika Gupta *,Amandeep kaur*,Jyoti Rajput*, Daisy Sahni* *Department of Anatomy, Post Graduate Institute of Medical Education and Research, Chandigarh, ABSTRACT During routine cadaveric dissection for undergraduate teaching variation in the course and insertion of fibers left trapezius muscle was noticed in two embalmed male cadavers. Some of the occipital fibers while descending towards clavicle got separated from rest of the muscle, inclined medially and inserted on the 1cm area of middle third of superior surface of clavicle. The remaining occipital fibers got inserted after a gap of on 1.5cm on the superior surface of lateral part of clavicle. Detached portion of trapezius muscles was tendinous in insertion. Two structures namely external jugular vein and supraclavicular nerves were seen passing through the gap in one cadaver (Case 1) whereas in other cadaver (Case 2) only external jugular vein was passing through the gap. Knowledge of this variation is clinically important in surgical exploration of posterior triangle.supraclavicular nerve entrapment syndrome and in various approaches involving external jugular vein. Key words: - trapezius muscle, cleidoccipital, supraclavicular nerves INTRODUCTION insertion of clavicular fibers left trapezius muscle of Trapezius muscle(TM) is a flat triangular muscle left side was noticed in two adult male cadavers. which extends over back of the neck and upper Case 1- In 78- years-old male cadaver trapezius thorax. On either side the muscle is attached to muscle of left side took usual origin from the medial medial third of superior nuchal line, external occipital portion of superior nuchal line, external occipital protuberance, ligamentum nuchae and apices of the protuberance, ligamentum nuchae and apices of the spinous processes and their supraspinous ligament spinous processes of thoracic vertebrae. -

Neck Dissection Using the Fascial Planes Technique
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY NECK DISSECTION USING THE FASCIAL PLANE TECHNIQUE Patrick J Bradley & Javier Gavilán The importance of identifying the presence larised in the English world in the mid-20th of metastatic neck disease with head and century by Etore Bocca, an Italian otola- neck cancer is recognised as a prominent ryngologist, and his colleagues 5. factor determining patients’ prognosis. The current available techniques to identify Fascial compartments allow the removal disease in the neck all have limitations in of cervical lymphatic tissue by separating terms of accuracy; thus, elective neck dis- and removing the fascial walls of these section is the usual choice for management “containers” along with their contents of the clinically N0 neck (cN0) when the from the underlying vascular, glandular, risk of harbouring occult regional metasta- neural, and muscular structures. sis is significant (≥20%) 1. Methods availa- ble to identify the N+ (cN+) neck include Anatomical basis imaging (CT, MRI, PET), ultrasound- guided fine needle aspiration cytology The basic understanding of fascial planes (USGFNAC), and sentinel node biopsy, in the neck is that there are two distinct and are used depending on resource fascial layers, the superficial cervical fas- availability, for the patient as well as the cia, and the deep cervical fascia (Figures local health service. In many countries, 1A-C). certainly in Africa and Asia, these facilities are not available or affordable. In such Superficial cervical fascia circumstances patients with head and neck cancer whose primary disease is being The superficial cervical fascia is a connec- treated surgically should also have the tive tissue layer lying just below the der- neck treated surgically. -

Unusual Morphology of the Superior Belly of Omohyoid Muscle
Case Report http://dx.doi.org/10.5115/acb.2014.47.4.271 pISSN 2093-3665 eISSN 2093-3673 Unusual morphology of the superior belly of omohyoid muscle Rajesh Thangarajan, Prakashchandra Shetty, Srinivasa Rao Sirasanagnadla, Melanie Rose D’souza Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Manipal, Karnataka, India Abstract: Though anomalies of the superior belly of the omohyoid have been described in medical literature, absence of superior belly of omohyoid is rarely reported. Herein, we report a rare case of unilateral absence of muscular part of superior belly of omohyoid. During laboratory dissections for medical undergraduate students, unusual morphology of the superior belly of the omohyoid muscle has been observed in formalin embalmed male cadaver of South Indian origin. The muscular part of the superior belly of the omohyoid was completely absent. The inferior belly originated normally from the upper border of scapula, and continued with a fibrous tendon which ran vertically lateral to sternohyoid muscle and finally attached to the lower border of the body of hyoid bone. The fibrous tendon was about 1 mm thick and received a nerve supply form the superior root of the ansa cervicalis. As omohyoid mucle is used to achieve the reconstruction of the laryngeal muscles and bowed vocal folds, the knowledge of the possible anomalies of the omohyoid muscle is important during neck surgeries. Key words: Superior belly, Fibrous tendon, Omohyoid, Neck surgery Received March 12, 2014; Revised April 3, 2014; Accepted April 28, 2014 Introduction bellies, absence and adhesion to sternohyoid are the reported anomalies of the superior belly of the OH [2]. -

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -

A Pocket Manual of Percussion And
r — TC‘ B - •' ■ C T A POCKET MANUAL OF PERCUSSION | AUSCULTATION FOB PHYSICIANS AND STUDENTS. TRANSLATED FROM THE SECOND GERMAN EDITION J. O. HIRSCHFELDER. San Fbancisco: A. L. BANCROFT & COMPANY, PUBLISHEBS, BOOKSELLEBS & STATIONEB3. 1873. Entered according to Act of Congress, in the year 1872, By A. L. BANCROFT & COMPANY, Iii the office of the Librarian of Congress, at Washington. TRAN jLATOR’S PREFACE. However numerou- the works that have been previously published in the Fi 'lish language on the subject of Per- cussion and Auscultation, there has ever existed a lack of a complete yet concise manual, suitable for the pocket. The translation of this work, which is extensively used in the Universities of Germany, is intended to supply this want, and it is hoped will prove a valuable companion to the careful student and practitioner. J. 0. H. San Francisco, November, 1872. PERCUSSION. For the practice of percussion we employ a pleximeter, or a finger, upon which we strike with a hammer, or a finger, producing a sound, the character of which varies according to the condition of the organs lying underneath the spot percussed. In order to determine the extent of the sound produced, we may imagine the following lines to be drawr n upon the chest: (1) the mammary line, which begins at the union of the inner and middle third of the clavicle, and extends downwards through the nipple; (2) the paraster- nal line, which extends midway between the sternum and nipple ; (3) the axillary line, which extends from the centre of the axilla to the end of the 11th rib. -

3 Approach-Related Complications Following Anterior Cervical Spine Surgery: Dysphagia, Dysphonia, and Esophageal Perforations
3 Approach-Related Complications Following Anterior Cervical Spine Surgery: Dysphagia, Dysphonia, and Esophageal Perforations Bharat R. Dave, D. Devanand, and Gautam Zaveri Introduction This chapter analyzes the problems of dysphagia, dysphonia, and esophageal tears during the Pathology involving the anterior subaxial anterior approach to the cervical spine and cervical spine is most commonly accessed suggests ways of prevention and management. through an anterior retropharyngeal approach (Fig. 3.1). While this approach uses tissue planes to access the anterior cervical spine, visceral Dysphagia structures such as the trachea and esophagus and nerves such as the recurrent laryngeal Dysphagia or difficulty in swallowing is a nerve (RLN), superior laryngeal nerve (SLN), and symptom indicative of impairment in the ability pharyngeal plexus are vulnerable to direct or to swallow because of neurologic or structural traction injury (Table 3.1). Complaints such as problems that alter the normal swallowing dysphagia and dysphonia are not rare following process. Postoperative dysphagia is labeled as anterior cervical spine surgery. The treating acute if the patient presents with difficulty in surgeon must be aware of these possible swallowing within 1 week following surgery, complications, must actively look for them in intermediate if the presentation is within 1 to the postoperative period, and deal with them 6 weeks, and chronic if the presentation is longer expeditiously to avoid secondary complications. than 6 weeks after surgery. Common carotid artery Platysma muscle Sternohyoid muscle Vagus nerve Recurrent laryngeal nerve Longus colli muscle Internal jugular artery Anterior scalene muscle Middle scalene muscle External jugular vein Posterior scalene muscle Fig. 3.1 Anterior retropharyngeal approach to the cervical spine. -

Unusual Organization of the Ansa Cervicalis: a Case Report
CASE REPORT ISSN- 0102-9010 UNUSUAL ORGANIZATION OF THE ANSA CERVICALIS: A CASE REPORT Ranjana Verma1, Srijit Das2 and Rajesh Suri3 Department of Anatomy, Maulana Azad Medical College, New Delhi-110002, India. ABSTRACT The superior root of the ansa cervicalis is formed by C1 fibers carried by the hypoglossal nerve, whereas the inferior root is contributed by C2 and C3 nerves. We report a rare finding in a 40-year-old male cadaver in which the vagus nerve fused with the hypoglossal nerve immediately after its exit from the skull on the left side. The vagus nerve supplied branches to the sternohyoid, sternothyroid and superior belly of the omohyoid muscles and also contributed to the formation of the superior root of the ansa cervicalis. In this arrangement, paralysis of the infrahyoid muscles may result following lesion of the vagus nerve anywhere in the neck. The cervical location of the vagus nerve was anterior to the common carotid artery within the carotid sheath. This case report may be of clinical interest to surgeons who perform laryngeal reinnervation and neurologists who diagnose nerve disorders. Key words: Ansa cervicalis, hypoglossal nerve, vagus nerve, variations INTRODUCTION cadaver. The right side was normal. The neck region The ansa cervicalis is a nerve loop formed was dissected and the neural structures in the carotid by the union of superior and inferior roots. The and muscular triangle regions were exposed, with superior root is a branch of the hypoglossal nerve particular attention given to the organization of the containing C1 fibers, whereas the inferior root is ansa cervicalis. -

Head & Neck Surgery Course
Head & Neck Surgery Course Parapharyngeal space: surgical anatomy Dr Pierfrancesco PELLICCIA Pr Benjamin LALLEMANT Service ORL et CMF CHU de Nîmes CH de Arles Introduction • Potential deep neck space • Shaped as an inverted pyramid • Base of the pyramid: skull base • Apex of the pyramid: greater cornu of the hyoid bone Introduction • 2 compartments – Prestyloid – Poststyloid Anatomy: boundaries • Superior: small portion of temporal bone • Inferior: junction of the posterior belly of the digastric and the hyoid bone Anatomy: boundaries Anatomy: boundaries • Posterior: deep fascia and paravertebral muscle • Anterior: pterygomandibular raphe and medial pterygoid muscle fascia Anatomy: boundaries • Medial: pharynx (pharyngobasilar fascia, pharyngeal wall, buccopharyngeal fascia) • Lateral: superficial layer of deep fascia • Medial pterygoid muscle fascia • Mandibular ramus • Retromandibular portion of the deep lobe of the parotid gland • Posterior belly of digastric muscle • 2 ligaments – Sphenomandibular ligament – Stylomandibular ligament Aponeurosis and ligaments Aponeurosis and ligaments • Stylopharyngeal aponeurosis: separates parapharyngeal spaces to two compartments: – Prestyloid – Poststyloid • Cloison sagittale: separates parapharyngeal and retropharyngeal space Aponeurosis and ligaments Stylopharyngeal aponeurosis Muscles stylohyoidien Stylopharyngeal , And styloglossus muscles Prestyloid compartment Contents: – Retromandibular portion of the deep lobe of the parotid gland – Minor or ectopic salivary gland – CN V branch to tensor -

HUMAN ANATOMY: a Prosection Guide
HUMAN ANATOMY: A Prosection Guide 3rd Edition Frank J. Daly Cover image www.kendallhunt.com Send all inquiries to: 4050 Westmark Drive Dubuque, IA 52004-1840 Copyright © 2010 by Frank J. Daly. ISBN 978-0-7575- All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the copyright owner. Printed in the United States of America 10 9 8 7 6 5 4 3 2 1 iii GROSS ANATOMY LABORATORY PROCEDURES 1. Appropriate laboratory attire is required: Scrubs (full-length, scrub pants), close-toed shoes (no Crocs), safety glasses, and Nitrile gloves. Scrubs are available in the campus bookstore (no specific color required). NO shorts or skirts permitted, even if made from scrub material. Safety glasses for splash protection are available in the lab. Gloves will be provided; please try to limit use to ~ 1 pair/session. Long hair must be tied back, away from the face. Long necklaces should be removed. Contact Lenses are NOT advised, as they are permeable to volatile compounds and may result in injury. Students should bring their lab manual to lab sessions. 2. No food or beverages are allowed in the laboratory - EVER. Smoking and/or chewing gum is prohibited in the laboratory. 3. No cadaveric materials (or models) are EVER to be removed from the Gross Anatomy lab. This is a State and a Federal law. You WILL be prosecuted to the fullest extent of the law.