Balfour Hospital Unannounced Inspection Report Nov 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Bus Route X1
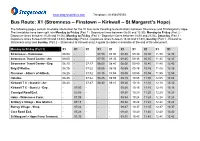
www.stagecoachbus.com Telephone: 01856870555. Bus Route: X1 (Stromness – Finstown – Kirkwall – St Margaret’s Hope) The following pages contain timetable information for the X1 bus route travelling to destinations between Stromness and St Margaret’s Hope. The timetables have been split into Monday to Friday (Part 1 - Departure times between 06:00 and 12:30), Monday to Friday (Part 2 - Departure times between 13:20 and 18:00), Monday to Friday (Part 3 - Departure times between 18:30 and 21:05), Saturday (Part 1 - Departure times between 07:00 and 13:30), Saturday (Part 2 - Departure times between 14:30 and 01:30), Sunday (Part 1 - Kirkwall to Stromness only) and Sunday (Part 2 – Stromness to Kirkwall only) A guide to codes is available at the end of this document. Monday to Friday (Part 1) X1 X1 X1 X1 X1 X1 X1 X1 X1 X1 Stromness - Hamnavoe. 06:00 - - 07:50 08:30 08:40 09:30 10:30 11:30 12:30 Stromness Travel Centre - Arr. 06:05 - - 07:55 08:35 08:45 09:35 10:35 11:35 12:35 Stromness Travel Centre - Dep. 06:10 - 07:17 08:00 08:40 08:50 09:40 10:40 11:40 12:40 Brig O’Waithe. 06:15 - 07:22 08:05 08:45 08:55 09:45 10:45 11:45 12:45 Finstown - Allan’s of Gillock. 06:25 - 07:32 08:15 08:55 09:05 09:55 10:55 11:55 12:55 Hatston. 06:35 - 07:42 08:25 09:05 09:15 10:05 11:05 12:05 13:05 Kirkwall T C - Stand 2 - Arr. -

Service St Margaret's Hope (Ferry Terminal) - Stromness (Hamnavoe) X1 Monday - Friday (Not Bank Holidays)
Service St Margaret's Hope (Ferry Terminal) - Stromness (Hamnavoe) X1 Monday - Friday (not Bank Holidays) Operated by: OC Stagecoach Highlands Timetable valid from 5 Sep 2021 until further notice Service: X1 X1 X1 X1 X1 X1 X1 X1 X1 X1 X1 Notes: XPrd1 Operator: OC OC OC OC OC OC OC OC OC OC OC St Margarets Hope, Ferry terminal Depart: .... .... .... .... .... .... 07:37 .... .... 08:47 09:47 Burray, Shop .... .... .... .... .... .... 07:45 .... .... 08:55 09:55 St Marys, Graeme Park .... .... .... .... .... .... 07:54 .... .... 09:04 10:04 Kirkwall, Hospital Entrance .... .... 06:21 .... .... 07:45 08:05 .... .... 09:15 10:15 Kirkwall, Travel Centre (Stand 2) Arrive: .... .... 06:24 .... .... 07:48 08:08 .... .... 09:18 10:18 Kirkwall, Travel Centre (Stand 2) Depart: 05:05 06:05 06:25 06:55 .... 07:50 .... 08:50 .... 09:20 10:20 Kirkwall, Hatston Bus Garage 05:10 06:10 06:30 07:00 07:10 07:55 .... 08:55 09:00 09:25 10:25 Finstown, Allan's of Gillock 05:20 06:20 06:40 07:10 07:20 08:05 .... 09:05 09:10 09:35 10:35 Stenness, Garage 05:27 06:27 06:47 07:17 07:27 08:12 .... 09:12 09:17 09:42 10:42 Stromness, Travel Centre Arrive: 05:35 .... 06:55 07:25 .... 08:20 .... 09:20 09:30 09:50 10:50 Stromness, Travel Centre Depart: 05:36 .... 06:56 07:26 .... 08:22 .... 09:22 .... 09:52 10:52 Stromness, Hamnavoe Estate Arrive: 05:39 06:35 06:59 07:29 07:35 08:25 ... -

The Kirk in the Garden of Evie
THE KIRK IN THE GARDEN OF EVIE A Thumbnail Sketch of the History of the Church in Evie Trevor G Hunt Minister of the linked Churches of Evie, Firth and Rendall, Orkney First Published by Evie Kirk Session Evie, Orkney. 1987 Republished 1996 ComPrint, Orkney 908056 Forward to the 1987 Publication This brief history was compiled for the centenary of the present Evie Church building and I am indebted to all who have helped me in this work. I am especially indebted to the Kirk’s present Session Clerk, William Wood of Aikerness, who furnished useful local information, searched through old Session Minutes, and compiled the list of ministers for Appendix 3. Alastair Marwick of Whitemire, Clerk to the Board, supplied a good deal of literature, obtained a copy of the Title Deeds, gained access to the “Kirk aboon the Hill”, and conducted a tour (even across fields in his car) to various sites. He also contributed valuable local information and I am grateful for all his support. Thanks are also due to Margaret Halcro of Lower Crowrar, Rendall, for information about her name sake, and to the Moars of Crook, Rendall, for other Halcro family details. And to Sheila Lyon (Hestwall, Sandwick), who contributed information about Margaret Halcro (of the seventeenth century!). TREVOR G HUNT Finstown Manse March 1987 Foreword to the 1996 Publication Nearly ten years on seemed a good time to make this history available again, and to use the advances in computer technology to improve its appearance and to make one or two minor corrections.. I was also anxious to include the text of the history as a page on the Evie, Firth and Rendall Churches’ Internet site for reference and, since revision was necessary to do this, it was an opportunity to republish in printed form. -

The Significance of the Ancient Standing Stones, Villages, Tombs on Orkney Island
The Proceedings of the International Conference on Creationism Volume 5 Print Reference: Pages 561-572 Article 43 2003 The Significance of the Ancient Standing Stones, Villages, Tombs on Orkney Island Lawson L. Schroeder Philip L. Schroeder Bryan College Follow this and additional works at: https://digitalcommons.cedarville.edu/icc_proceedings DigitalCommons@Cedarville provides a publication platform for fully open access journals, which means that all articles are available on the Internet to all users immediately upon publication. However, the opinions and sentiments expressed by the authors of articles published in our journals do not necessarily indicate the endorsement or reflect the views of DigitalCommons@Cedarville, the Centennial Library, or Cedarville University and its employees. The authors are solely responsible for the content of their work. Please address questions to [email protected]. Browse the contents of this volume of The Proceedings of the International Conference on Creationism. Recommended Citation Schroeder, Lawson L. and Schroeder, Philip L. (2003) "The Significance of the Ancient Standing Stones, Villages, Tombs on Orkney Island," The Proceedings of the International Conference on Creationism: Vol. 5 , Article 43. Available at: https://digitalcommons.cedarville.edu/icc_proceedings/vol5/iss1/43 THE SIGNIFICANCE OF THE ANCIENT STANDING STONES, VILLAGES AND TOMBS FOUND ON THE ORKNEY ISLANDS LAWSON L. SCHROEDER, D.D.S. PHILIP L. SCHROEDER 5889 MILLSTONE RUN BRYAN COLLEGE STONE MOUNTAIN, GA 30087 P. O. BOX 7484 DAYTON, TN 37321-7000 KEYWORDS: Orkney Islands, ancient stone structures, Skara Brae, Maes Howe, broch, Ring of Brodgar, Standing Stones of Stenness, dispersion, Babel, famine, Ice Age ABSTRACT The Orkney Islands make up an archipelago north of Scotland. -

Galeed, 6.38 Acres Or Thereby, Stenness
T: 01856 873151 F: 01856 875450 E: [email protected] W: www.lowsorkney.co.uk Galeed, extending to 6.38 acres or thereby, Stenness, KW16 3LD Galeed enjoys an outstanding panoramic view, including the Ring of Brodgar and Standing Stones of Stenness together with the Stenness and Harray Lochs, from its elevated position. The building site will have mains water and electricity connection and there is OFFERS OVER planning consent (OIC ref 19/091/PIP) to £120,000 replace the existing ruin with a new dwellinghouse. Access is from the Ireland road to the south and the land outwith the building site may especially appeal to horse or other livestock owners. Galeed, 6.38 acres or thereby, Stenness © Crown Copyright. All rights reserved. Licence number SR 100001231 SERVICES – The site will have a mains water supply and electricity supply with the purchaser only liable for the final connection charges to their new house. ENTRY – By arrangement. VIEWING - For an appointment to view please contact Lows Property Department. PRICE – Offers over £120,000. Further enquires should be directed to Lows Property Department, with whom all offers should be lodged in writing. DJMF The following notes are of crucial importance to intending viewers and/or purchasers of the property. 1. These particulars do not form part of any offer or contract and all statements and measurements contained herein are believed to be correct but are not guaranteed, and any intending purchaser must satisfy themselves as to their accuracy. Prospective purchasers are advised to have their interest noted through their solicitors as soon as possible in order that they may be informed in the event of an early Lows Solicitors – Estate Agents closing date being set for receipt of offers. -

NHS Orkney Asset Management Summary 2019 to 2029
Appendix 5 NHS Orkney Asset Management Summary 2019 to 2029 Planning Regionally, Delivering Locally 1. Introduction NHS Orkney is the smallest territorial health board in Scotland and is responsible for the health care of the population of Orkney. The Board employs around 620 staff and provides a comprehensive range of primary, community-based and acute hospital services. This year has seen the handover of the new Balfour hospital and healthcare facility. This exciting opportunity provides state of the art facilities which is matched by ambitious plans for services and staff across Orkney. 2018-2019 was the last complete financial year prior to the completion of the new Balfour hospital and healthcare facility. It was not however, the sole focus of attention and many other aspects of service delivery have continued to be developed. Although small in scale, NHS Orkney delivers a full range of clinical services, hospital and community based and in common with many other health systems across Scotland face challenges in terms of meeting rising demand, rising costs and perhaps most significantly recruitment to key posts, clinical and non-clinical. 2. Strategic Plan The full scale of NHS Orkney’s priorities for investment aimed at responding to both the current and future challenges it faces, and to deliver its emerging service model include: • Development of integrated hospital and health care facilities incorporating a Rural General Hospital supported by appropriate community rehabilitation and enablement services. • Development of two new primary care hubs to the East and West Mainland. • Improvements to primary and community care facilities to ensure they support the provision of safe and sustainable clinical services to each local community. -

3 Bus Time Schedule & Line Route
3 bus time schedule & line map 3 Kirkwall (Travel Centre) - Deerness (Lighthouse View In Website Mode Corner) The 3 bus line (Kirkwall (Travel Centre) - Deerness (Lighthouse Corner)) has 2 routes. For regular weekdays, their operation hours are: (1) Deerness: 7:15 AM (2) Kirkwall: 7:45 AM - 5:25 PM Use the Moovit App to ƒnd the closest 3 bus station near you and ƒnd out when is the next 3 bus arriving. Direction: Deerness 3 bus Time Schedule 42 stops Deerness Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:15 AM Travel Centre, Kirkwall West Castle Street, Kirkwall Tuesday 7:15 AM Hornesquoy Road, Kirkwall Wednesday 7:15 AM New Balfour Hospital, Kirkwall Thursday 7:15 AM Friday 7:15 AM Macmillan, Kirkwall Saturday Not Operational Hospital Entrance, Kirkwall Macmillan, Kirkwall Upper Crantit Road, Kirkwall 3 bus Info Holm Branch Road, Kirkwall Direction: Deerness Stops: 42 Easdale Close, Kirkwall Trip Duration: 30 min Easdale Close, Kirkwall Line Summary: Travel Centre, Kirkwall, Hornesquoy Road, Kirkwall, New Balfour Hospital, Kirkwall, Lynn Road, Kirkwall Macmillan, Kirkwall, Hospital Entrance, Kirkwall, Macmillan, Kirkwall, Upper Crantit Road, Kirkwall, Heathery Loan East End, St Ola Easdale Close, Kirkwall, Lynn Road, Kirkwall, Heathery Loan East End, St Ola, Wideford Cottages, Wideford Cottages, St Ola St Ola, Airport Terminal, Kirkwall Airport, Road End, Kirkwall Airport, Bossack Junction, Tankerness, Longtownmail, Tankerness, Mossclair, Tankerness, Airport Terminal, Kirkwall Airport Swarsquoy Road End, Tankerness, -

Lower Quoys, Evie
T: 01856 873151 F: 01856 875450 E: [email protected] W: www.lowsorkney.co.uk Lower Quoys, extending to 3.1 acres or thereby, Evie, KW17 2PH Lower Quoys comprises 3 well-appointed dwellinghouses the largest of which is presently a family home with the others being successful holiday lets. The dwellings have been completely renovated, to a high standard, over the last 5 years. OFFERS OVER The attractive property is set in well-maintained garden grounds and has substantial traditional £450,000 outbuildings, offering potential for further development, to the rear and paddocks. The property offers an excellent life style changing opportunity and enjoys beautiful sea views. LOWER QUOYS - LIVING ROOM • Lower Quoys – 3 bedroom semi-detached two LOWER QUOYS - DINING ROOM storey house. Multi-fuel stoves in living room and dining room. Modern kitchen. Bathroom. UPVC framed double glazed window, oil-fired central heating. • Lower Quoys Holiday Cottage – 2 bedroom semi-detached two storey house. Multi-fuel stoves in living room and dining room. Modern kitchen. Modern electric panel heaters. • Mole End – one bedroom detached bungalow. LOWER QUOYS - KITCHEN Open plan living room/kitchen. Aga multi-fuel stove. Modern kitchen. Bathroom. Large decked area with views across to Eynhallow Sound. • Outbuildings include a former byre and a barn with loft and store offer potential for further development subject to the necessary planning consents. Large garage. Several garden stores. LOCATION Lower Quoys is located in the parish of Evie where there is a modern primary school, post office/shop, local café & wildlife centre at Tingwall. Kirkwall lies approximately 15 miles away. -

Download the Orkney Sailing Guide
Sailing notes downloaded from the Orkney Marinas website. www.orkneymarinas.co.uk Westray to Kirkwall We hope you find these notes helpful and of interest to you while planning your sailing trip to Orkney. Please note they are not intended to be used for navigation The quickest journey is to leave Westray so that the last of the flood takes you into Kirkwall Bay. If the weather is okay and you do not go to early the tide should be going west through Weatherness and Fersness. Unless the wind is strong there should be no problem crossing the Westray Firth on the flood. There can be a bit if a roost during strong SE wind and flood tide running SE from Kili Holm. If the weather is suitable and you go west of Rusk Holm give Rusk Holm a good berth and let the flood help you down the middle towards the Galt Buoy. Do not go too near the Egilsay shore as there will be a strong eddy running north (very handy if you are going out against the flood). If you come down the west side of Pharay or out through Fersness hold up for the SW corner of Rusk Holm before standing out across the firth. When going from Westray to Kirkwall during ebbing water after passing through either Weatherness or Fersness keep down along the west side of Eday to Seal Skerry here you will meet a strong ebb tide. If you can crab across to the Muckle Green Holm you will get some benefit from an eddy until you again come into a strong tide at the SW corner of the little Green Holm this one will help a bit as you hold up toward the Galt buoy. -

Pierowall Church Statement of Significance
Property in Care (PIC) ID: PIC310 Designations: Scheduled Monument (SM13416) Taken into State care: 1911 (Guardianship) Last reviewed: 2004 STATEMENT OF SIGNIFICANCE PIEROWALL CHURCH We continually revise our Statements of Significance, so they may vary in length, format and level of detail. While every effort is made to keep them up to date, they should not be considered a definitive or final assessment of our properties. Historic Environment Scotland – Scottish Charity No. SC045925 Principal Office: Longmore House, Salisbury Place, Edinburgh EH9 1SH © Historic Environment Scotland 2019 You may re-use this information (excluding logos and images) free of charge in any format or medium, under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit http://nationalarchives.gov.uk/doc/open- government-licence/version/3/ or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned. Any enquiries regarding this document should be sent to us at: Historic Environment Scotland Longmore House Salisbury Place Edinburgh EH9 1SH +44 (0) 131 668 8600 www.historicenvironment.scot You can download this publication from our website at www.historicenvironment.scot Historic Environment Scotland – Scottish Charity No. SC045925 Principal Office: Longmore House, Salisbury Place, Edinburgh EH9 1SH PIEROWALL CHURCH BRIEF DESCRIPTION The monument comprises the remains of a medieval parish church (Ladykirk). It is situated in the village of Pierowall, the main settlement on the northern Orcadian island of Westray. -

Kirkwall (Potentially Vulnerable Area 03/05)
Kirkwall (Potentially Vulnerable Area 03/05) Local Plan District Local authority Main catchment Orkney Orkney Islands Council Orkney coastal Summary of flooding impacts Summary of flooding impactsSummary At risk of flooding • 490 residential properties • 460 non-residential properties • £2.5 million Annual Average Damages (damages by flood source shown left) Summary of objectives to manage flooding Objectives have been set by SEPA and agreed with flood risk management authorities. These are the aims for managing local flood risk. The objectives have been grouped in three main ways: by reducing risk, avoiding increasing risk or accepting risk by maintaining current levels of management. Objectives Many organisations, such as Scottish Water and energy companies, actively maintain and manage their own assets including their risk from flooding. Where known, these actions are described here. Scottish Natural Heritage and Historic Environment Scotland work with site owners to manage flooding where appropriate at designated environmental and/or cultural heritage sites. These actions are not detailed further in the Flood Risk Management Strategies. Summary of actions to manage flooding The actions below have been selected to manage flood risk. Flood Natural flood New flood Community Property level Site protection protection management warning flood action protection plans scheme/works works groups scheme Actions Flood Natural flood Maintain flood Awareness Surface water Emergency protection management warning raising plan/study plans/response study study Maintain flood Strategic Flood Planning Self help Maintenance protection mapping and forecasting policies scheme modelling 59 Section 2 Orkney Local Plan District Kirkwall (Potentially Vulnerable Area 03/05) Local Plan District Local authority Main catchment Orkney Orkney Islands Council Orkney coastal Background This Potentially Vulnerable Area The airport is located in this Potentially includes the south-east of Orkney Vulnerable Area. -

Ports Handbook for Orkney 6Th Edition CONTENTS
Ports Handbook for Orkney 6th Edition CONTENTS General Contact Details 4 Introduction 5 Orkney Harbour Authority Area Map 6 Pilotage Services & Pilotage Index to PIERS & HARBOURS 45 Exemption Certificates 7 Main Piers Data 46-47 Orkney VTS 8 Piers: Reporting Points 9 Burray 48-49 Radar & AIS Coverage 10-11 Burwick 50-51 Port Passage Planning 12 Backaland 52-53 Suggested tracks Egilsay 54-55 Scapa Flow, Kirkwall, Stromness 13-15 Gibraltar 56-57 Prior notification requirements 16 Sutherland 58-59 Preparations for Port Entry 17 Graemsay 60-61 Harbour Craft 18 Holm 62-63 Port Security - (ISPS code) 19 Houton 64-65 Port Health 20 Longhope 66-67 Port Medical Officers Services 21 Lyness 68-71 Port Waste Reception Facilities 22 Moaness 72-73 Traffic Movements in Orkney 23 Kirkwall 74-78 Ferry Routes in & around Orkney 24 Hatston 79-83 Fishing Vessel Facilities 25 Hatston Slipway 84-85 Diving Support Boats 26 Nouster 86-87 Principal Wreck & Dive Sites Moclett 88-89 in Scapa Flow 27 Trumland 90-91 Towage & Tugs 28-31 Kettletoft 92-93 Ship to Ship Cargo Transhipments 32 Loth 94-95 Flotta Oil Terminal 34-38 Scapa 96-97 Guide to good practice for small Scapa Flow 98-99 vessel bunkering operations 39 Balfour 100-101 Guide to good practice for the Stromness 102-106 disposal of waste materials 40 Copland’s Dock 107-111 Fixed Navigation lights 41-44 Pole Star 112-113 Stronsay 114-115 Whitehall 116-117 Tingwall 118-119 Marinas 126-130 Pierowall 120-121 Tidal Atlas 131-144 Rapness 122-123 Pollution Prevention Guidelines 145 Wyre 124-125 2 3 PORTS HANDBOOK – 6TH EDITION The Orkney County Council Act of 1974 As a Harbour Authority, the Council’s aim, authorised the Orkney Islands Council through Marine Services, is to ensure that to exercise jurisdiction as a Statutory Orkney’s piers and harbours are operated Harbour Authority and defined the in a safe and cost effective manner.