The Chronological History of the Rotunda Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
On the Structure of the Roman Pantheon 25
College Art Association http://www.jstor.org/stable/3050861 . Your use of the JSTOR archive indicates your acceptance of JSTOR's Terms and Conditions of Use, available at . http://www.jstor.org/page/info/about/policies/terms.jsp. JSTOR's Terms and Conditions of Use provides, in part, that unless you have obtained prior permission, you may not download an entire issue of a journal or multiple copies of articles, and you may use content in the JSTOR archive only for your personal, non-commercial use. Please contact the publisher regarding any further use of this work. Publisher contact information may be obtained at . http://www.jstor.org/action/showPublisher?publisherCode=caa. Each copy of any part of a JSTOR transmission must contain the same copyright notice that appears on the screen or printed page of such transmission. JSTOR is a not-for-profit service that helps scholars, researchers, and students discover, use, and build upon a wide range of content in a trusted digital archive. We use information technology and tools to increase productivity and facilitate new forms of scholarship. For more information about JSTOR, please contact [email protected]. College Art Association is collaborating with JSTOR to digitize, preserve and extend access to The Art Bulletin. http://www.jstor.org On the Structureof the Roman Pantheon Robert Mark and Paul Hutchinson Since the time of its construction, the bold, brilliantly simple schema of Hadrian's Pantheon has inspired much emulation, commendation, and even fear. Modern commentators tend to view the building as a high point in an "architectural rev- olution" brought about mainly through the Roman development of a superior poz- zolana concrete that lent itself to the forming of unitary, three-dimensional struc- tures. -
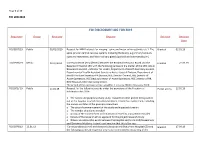
Foi Disclosure Log for 2019
Page 1 of 17 FOI LOG 2019 FOI DISCLOSURE LOG FOR 2019 Requester Group Received Request Decision Decision Date FOI/3957/19 Public 02/01/2019 Request for MRI Protocols for imaging - spine and major salivary glands, etc 1. The Granted 02.01.19 spine (and/or central nervous systems including the brain), e.g primary tumours, cysts and metastasis; and Major salivary glands (parotid and sub-mandibular). FOI/3970/19 Media 09.01/2019 Correspondence (email/letter) between the Beaumont Hospital Board and the Granted 27.03.19 Beaumont Hospital CEO with the following parties on the matter of the CEO role at Beaumont Hospital – Minister for Health, Department of Health Secretary General, Department of Health Assistant Secretary-Acute Hospital Division, Department of Health Assistant Secretary-HR Division, HSE Director General, HSE Director of Acute Operations, HSE Deputy Director of Acute Operations, HSE Director of HR, RCSI Hospitals Chief Operating Officer. The period of the correspondence would be 1 January 2018 to 9 January 2019. FO/3972/ 19 Public 14.01.19 Request for the following records under the provisions of the Freedom of Partial access 12.02.19 Information Act 2014: o The names and purposes of any study, research or other project being carried out at the hospital in which Genomics Medicine Ireland has involvement, including the names and titles of the principal researchers o The date of commencement of the study and expected duration o The number of patients enrolled o A copy of the consent form and information issued to any patients enrolled -

The Ombudsman and Public Hospitals
The Ombudsman and the Public Hospitals The Ombudsman is Impartial Independent A free service 2 Who is the Ombudsman and what does the Ombudsman do? Peter Tyndall is the Ombudsman. The Ombudsman can examine complaints about the actions of a range of public bodies, including public hospitals. All hospitals providing public health services come within the Ombudsman’s remit. The Ombudsman can examine complaints about how hospital staff carry out their everyday administrative activities when providing public health services. These include complaints about delays or failing to take action. However, there are certain complaints that the Ombudsman cannot examine. These include complaints about: private health care regardless of where it is provided and clinical judgment by the HSE (diagnoses or decisions about treatment Is the Ombudsman independent? Yes. The Ombudsman is independent and impartial when examining complaints. 1 What can I complain to the Ombudsman about? You can complain about your experience in dealing with a hospital. This might include, among other issues, a hospital: applying an incorrect charge failing to follow approved administrative procedures, protocols or reasonable rules failing to communicate clearly failing to seek your informed consent to a procedure keeping poor records failing to respect your privacy and dignity having staff who are rude or unhelpful or who discriminate against you being reluctant to correct an error failing to deal with your complaint in accordance with the complaints process. 2 Which -

A Study of the Pantheon Through Time Caitlin Williams
Union College Union | Digital Works Honors Theses Student Work 6-2018 A Study of the Pantheon Through Time Caitlin Williams Follow this and additional works at: https://digitalworks.union.edu/theses Part of the Ancient History, Greek and Roman through Late Antiquity Commons, and the Classical Archaeology and Art History Commons Recommended Citation Williams, Caitlin, "A Study of the Pantheon Through Time" (2018). Honors Theses. 1689. https://digitalworks.union.edu/theses/1689 This Open Access is brought to you for free and open access by the Student Work at Union | Digital Works. It has been accepted for inclusion in Honors Theses by an authorized administrator of Union | Digital Works. For more information, please contact [email protected]. A Study of the Pantheon Through Time By Caitlin Williams * * * * * * * Submitted in partial fulfillment of the requirements for Honors in the Department of Classics UNION COLLEGE June, 2018 ABSTRACT WILLIAMS, CAITLIN A Study of the Pantheon Through Time. Department of Classics, June, 2018. ADVISOR: Hans-Friedrich Mueller. I analyze the Pantheon, one of the most well-preserVed buildings from antiquity, through time. I start with Agrippa's Pantheon, the original Pantheon that is no longer standing, which was built in 27 or 25 BC. What did it look like originally under Augustus? Why was it built? We then shift to the Pantheon that stands today, Hadrian-Trajan's Pantheon, which was completed around AD 125-128, and represents an example of an architectural reVolution. Was it eVen a temple? We also look at the Pantheon's conversion to a church, which helps explain why it is so well preserVed. -

The Book of the Rotunda Hospital
.'<••'',- '.' '': ,( I' /' 'v%. THE 8G»K ':my\- iOSPITAL KlRtPATRICK JELLETT THE LIBRARY OF THE UNIVERSITY OF CALIFORNIA LOS ANGELES THE BOOK OF THE ROTUNDA HOSPITAL BARTHOLOMEW MOSSE (fROM THE PORTRAIT IN THE BOARD ROOM OF THE HOSPITAL). THE BOOK OP THE ROTUNDA HOSPITAL AN ILLUSTRATED HISTORY OF THE DUBLIN LYING-IN HOSPITAL FROM ITS FOUNDATION IN 1745 TO THE PRESENT TIME T. PERCY C. [KIRKPATRICK, M.D., M.R.LA. FELLOW AND REGIS TEAE OP THE EOYAL COLLEGE OP PHYSICIANS OF IRELAND EDITED BY HENRY JELLETT, M.D., F.R.C.P.L MASTER OF THE HOSPITAL XonDon ADLARD & SON, BARTHOLOMEW PRESS BARTHOLOMEW" CLOSE, E.G. 1913 PRINTED BY ADLAKD AND SON LONDON AND DOEKINO tl/st:.T)iV. 1^/5 MISERIS • SOLAMEN • INSTITUIT M • DCC • L • VII Great hearted Founder, to whose prescient care we owe a debt that never can be paid, Accept the duteous thanks that love inspires, accept the tribute of a nation's praise. You worked to save the sick, to soothe the pain of those who heavy laden called for help, But, e'er the work was finished, passed away, leaving the future in Another's hands. Your statue stands within our ancient halls, your portrait looks upon our daily work. Poor dead and useless things, where every stone brings back again your living memory. What need have we of bronze or sculptor's skill to call back those who leave such work as you Whose sacrifice lives on—an endless spring of healing water on a thirsty earth ? J. PEEFACE rilHB Dublin Lying-in Hospital stands pre-eminent among similar "*- institutions of Great Britain and Ireland, whether one regards it from the point of view of its age, or the mag-nitude of the work it has done and is still doing. -

Operational Plan 2017 RCSI Hospital Group
Operational Plan 2017 RCSI Hospital Group 1. Introduction RCSI Hospital Group was established in The RCSI Hospital Budget outturn 2015 comprising the following hospitals: Group 2017 2016 Beaumont Hospital Connolly Hospital €M €M Cavan and Monaghan Hospital Net Total 686.2 685.4 Our Lady of Lourdes Hospital Increase Year on Year 0.8 Louth County Hospital 0.1% Rotunda Hospital Key challenges 2017 The Academic Partner for the Group is the €M Royal College of Surgeons in Ireland Pay policy pressures 13.8 (RCSI). Efficiency savings target 10.8 Increased income target 8.9 The RCSI Hospital Group serves populations in five counties – North Dublin, Meath, Louth, Cavan and Monaghan. The area stretches from the north banks of the River Liffey in Dublin City Centre, north to the border with Northern Ireland, and west to the border with County Donegal. It comprises urban, rural and commuter belt areas, and covers approximately 6,817 square kilometres in total. There is considerable variation in population density from a low of 39 persons per square kilometre in Cavan to a high of 4,139 persons per square kilometre in north Dublin city. Residents of neighbouring areas such as South Dublin and Kildare also access hospitals for secondary care and maternity services. Beaumont Hospital, which is the largest hospital in the group, in addition to providing emergency and acute Secondary Care services to the local community is also a designated Cancer Centre, the Regional Treatment Centre for Ear, Nose and Throat and Gastroenterology and also the National Referral Centre for Neurosurgery and Neurology, Renal Transplantation, and Cochlear Implantation - as such treating patients from all parts of the country. -

Directory of Hospitals (And Treatment Centres)
Directory of Hospitals (and Treatment Centres) How to use this directory: The directory below summarises the various approved hospitals and treatment centres we cover. These are organised by type of facility and category cover type. The categories are not a reflection of the level or quality of care provided. To determine the level of cover for a particular hospital and treatment centre, check the facility type, find the category cover type from the directory below and refer to your Table of Benefits. We have organised the directory by county to make it easier for you to find those near you. The directory changes from time to time. Please refer to www.vhi.ie/downloads for the most up-to-date list. FACILITY TYPE CATEGORY ADDITIONAL INFORMATION Hospitals (and Treatment Centres) COVER TYPE CAVAN HOSPITALS General Hospital, Cavan Public Hospital Public 1 CLARE HOSPITALS Cahercalla Community Hospital Private hospital Private 1 Mid-Western Hospital, Ennis Public hospital Public 1 OTHER MEDICAL FACILITIES Bushypark Treatment Centre, Ennis Private treatment centre Private 1 Covered for specified treatment programmes only CORK HOSPITALS Bon Secours Hospital, Cork ● Private hospital Private 2 Cork University Hospital Public hospital Public 2 Cork University Maternity Hospital Public hospital Public 2 General Hospital, Bantry Public hospital Public 1 General Hospital, Mallow Public hospital Public 1 Mercy University Hospital Public hospital Public 2 Shanakiel Hospital ● ■ u Private hospital Private 2 South Infirmary/Victoria University Hospital Ltd. Public hospital Public 2 St. Mary’s Orthopaedic Hospital Public hospital Public 1 OTHER MEDICAL FACILITIES Marymount Hospice Hospice Contact us for details Tabor Lodge, Belgooly Private treatment centre Private 1 Covered for specified treatment programmes only DONEGAL HOSPITALS General Hospital, Letterkenny Public hospital Public 1 OTHER MEDICAL FACILITIES White Oaks Rehabilitation Centre, Muff, Co. -

Rotunda ROM Magazine Subject Index V. 1 (1968) – V. 42 (2009)
Rotunda ROM Magazine Subject Index v. 1 (1968) – v. 42 (2009) 2009.12.02 Adam (Biblical figure)--In art: Hickl-Szabo, H. "Adam and Eve." Rotunda 2:4 (1969): 4-13. Aesthetic movement (Art): Kaellgren, P. "ROM answers." Rotunda 31:1 (1998): 46-47. Afghanistan--Antiquities: Golombek, L. "Memories of Afghanistan: as a student, our writer realized her dream of visiting the exotic lands she had known only through books and slides: thirty-five years later, she recalls the archaeoloigical treasures she explored in a land not yet ruined by tragedy." Rotunda 34:3 (2002): 24-31. Akhenaton, King of Egypt: Redford, D.B. "Heretic Pharoah: the Akhenaten Temple Project." Rotunda 17:3 (1984): 8-15. Kelley, A.L. "Pharoah's temple to the sun: archaeologists unearth the remains of the cult that failed." Rotunda 9:4 (1976): 32-39. Alabaster sculpture: Hickl-Szabo, H. "St. Catherine of Alexandria: memorial to Gerard Brett." Rotunda 3:3 (1970): 36-37. Keeble, K.C. "Medieval English alabasters." Rotunda 38:2 (2005): 14-21. Alahan Manastiri (Turkey): Gough, M. "They carved the stone: the monastery of Alahan." Rotunda 11:2 (1978): 4-13. Albertosaurus: Carr, T.D. "Baby face: ROM Albertosaurus reveals new findings on dinosaur development." Rotunda 34:3 (2002): 5. Alexander, the Great, 356-323 B.C.: Keeble, K.C. "The sincerest form of flattery: 17th-century French etchings of the battles of Alexander the Great." Rotunda 16:1 (1983): 30-35. Easson, A.H. "Macedonian coinage and its Hellenistic successors." Rotunda 15:4 (1982): 29-31. Leipen, N. "The search for Alexander: from the ROM collections." Rotunda 15:4 (1982): 23-28. -

Czech Republic Today
Rich in History 1 2 Magic Crossroads Whenever European nations were set in motion, they met in a rather small area called the Czech Republic today. Since the early Middle Ages, this area was crossed by long trade routes from the severe North to the sunny South; at the beginning of the first millennium, Christianity emerged from the West, and at its end communism arrived from the East. For six hundred years, the country was an independent Czech kingdom, for three hundred years, it belonged among Austro-Hungarian Empire lands, and since 1918 it has been a republic. In the 14th century, under the Bohemian and German King and Roman Emperor Charles IV, as well as in the 16th century under the Emperor Rudolf II, the country enjoyed a favourable position in European history and also played a great role internationally in the arts and in social affairs. In 1989, the whole world admired the Czechoslovak “velvet revolution” lead by charismatic dramatist Václav Havel, which put an end to socialist experimentation. Numerous famous architects, who built Romanesque churches in Germany but were no longer commissioned to build in their home countries due to the coming Gothic period, succeeded there; at the same time, the French type of Gothic architecture took root in Bohemia. A number of Italian Renaissance or Baroque architects, painters and sculptors, who crossed the Alps to find new opportunity for creating master works and look for well-paid jobs, were hired by members of Czech nobility and clergy; astonished by the mastery of Czech builders and craftsmen with whom they cooperated, they created wonderful castles and breathtaking Catholic churches. -

List of Approved Hospitals, Scan Centres & Treatment Centres
Cover For Me Cover For Us Cover For All Of Us Cover For Me Cover For Us Cover For All Of Us Hospital Maternity Out-Patient Activate Hospital & Core Plan Ranges Hospital Maternity Out-Patient Cover For Me Cover For Us Cover For All Of Us List Of Approved Hospitals, International Health & Travel Scan CentresSports Cover & Out-Patient Scan Treatment Centres September 2015 International Health & Travel Sports Cover Out-Patient Scan Hospital Maternity Out-Patient Women’s & Men's Health Complementary Therapy Dental & Optical Women’s & Men's Health Complementary Therapy Dental & Optical International Health & Travel Sports Cover Out-Patient Scan Women’s & Men's Health Complementary Therapy Dental & Optical 01 List Of Approved Hospitals Name of Hospital Type Cavan Cavan General Hospital Public Cover For Me Cover For Us Cover For All Of Us Clare Bushypark Treatment Centre, Ennis Addiction Centre Mid Western Regional Hospital, Ennis Public Cork Bantry General Hospital Public Bon Secours Hospital Private Cork University Hospital Public Hospital Maternity Out-Patient Cork University Maternity Hospital Public Cuan Mhuire, Farnanes Addiction Centre Mallow General Hospital Public Mater Private Cork Private Mercy University Hospital Public South Infirmary Victoria University Hospital Public St Mary’s Orthopaedic Hospital Public Tabor Lodge, Belgooly Addiction Centre International Health & Travel Sports Cover Out-Patient Scan Donegal Letterkenny General Hospital Public White Oaks Treatment Centre Addiction Centre Dublin Beacon Cancer Centre Private Beacon Hospital, Dublin 18 - Cardiac Procedures - All Plans High Tech - Private Beacon Hospital, Dublin 18 - All other procedures Private* Women’s & Men's Health Complementary Therapy Dental & Optical Beacon Hospital, Dublin 18 - Basic & Good Plans High Tech - Private * Beacon Hospital is classified as a private hospital (excluding cardiac procedures) for all plans in the Activate Hospital & Core plan ranges apart from Basic plan, Good plan & Activate Hospital plan. -

Health Cash Plans
Health Cash Plans Directory of Hospitals (and Treatment Centres) Applicable to new registrations or renewals on/or after 22nd July 2015. Postal Address: IDA Business Park, Purcellsinch, Dublin Road, Kilkenny. Telephone Number: 1890 44 44 44 Lines open: 8am – 6pm Monday – Friday 9am – 3pm Saturday Contact: Vhi.ie Vhi.ie/contact Offices Dublin: Vhi House, Lower Abbey Street, Dublin 1. Fax (01) 873 4004 Cork: Vhi House, 70 South Mall, Cork. Fax (021) 427 7901 Kilkenny: IDA Business Park, Purcellsinch, Dublin Road, Kilkenny. Fax (056) 776 1741 Vhi Healthcare Limited trading as Vhi Healthcare is regulated by the Central Bank of Ireland. 1 Directory of Hospitals (and Treatment Centres) Health Cash Plans How to use this directory: The directory below summarises the various approved hospitals and treatment centres which we cover under your Health Cash Plan. These are organised by type of facility. To determine the level of cover for a particular hospital and treatment centre, check the facility type and refer to your Table of Benefits and Terms and Conditions. We have organised the directory by county to make it easier for you to find those near you. The directory changes from time to time. Please refer to Vhi.ie/downloads for the most up-to-date list. Hospitals (and Treatment Centres) FACILITY TYPE ADDITIONAL INFORMATION CAVAN HOSPITALS General Hospital, Cavan Public Hospital CLARE HOSPITALS Mid-Western Hospital, Ennis Public hospital CORK HOSPITALS Bon Secours Hospital, Cork Private hospital Cork University Hospital Public hospital Cork University Maternity Hospital Public hospital General Hospital, Bantry Public hospital General Hospital, Mallow Public hospital Mercy University Hospital Public hospital Mater Private Hospital, Cork Private hospital South Infirmary/Victoria University Hospital Ltd. -

The Rotunda Hospital Ambulatory Hysteroscopy Service at Connolly Hospital
The Rotunda Hospital Ambulatory Hysteroscopy Service at Connolly Hospital Gynaecology Service Development Phase 1 FFiiinnaalll VVeerrrssiiioonn Date: 11th February 2016 1 CONTRIBUTORS Ms Pauline Treanor Secretary General Manager Rotunda Hospital Ms Margaret Philbin DOM/N Rotunda Hospital Ms Marie Keane ADOM/N Rotunda Hospital Dr. Eve Gaughan Consultant Obstetrician/Gynaecologist, Rotunda Hospital Ms Judy McEntee DON Connolly Hospital Ms Patricia Meade ADON Connolly Hospital Ms. Louise Collins Director of Clinical Services, Connolly Hospital Mr. Jim Hussey Director of Finance, Rotunda Hospital Mr. Sean Williamson Materials Manager, Rotunda Hospital 2 CONTENTS Page 1. Introduction 5 2. Background 5 3. Proposal 6 4. Current Gynaecological Service Overview 6 4.1 RCSI Hospital Group 6 4.2 Rotunda Hospital Gynaecological Activity 2014 7 5. Ambulatory Hysteroscopy Service Phase 1 Proposal 8 5.1 Ambulatory Outpatient Service – Resource 8 Requirement 6. Patient Pathway 9 7. Cherry Ward Ambulatory Procedure Room 9 8. Decontamination 9 9. ICT Support 10 10. Medical Emergency Management 10 11. Waste Management 10 12. Technical Services 10 13. Portering Services 10 14. Security Services 10 15. Laboratory 11 16. Cherry Ward Facility Requirements 11 17.Discharge Protocol 11 18.GP Communication 11 19. Breakdown of Total Costs both once off and recurring 12 3 APPENDICES Appendix 1 Rotunda Ambulatory Hysteroscopy Service – Patient Flow Pathway 14 Appendix 2 Standard Operating Procedure Medication Management 15 Appendix 3 Standard Operating Procedure Checking