TAVLESSE, INN-Fostamatinib
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Deregulated Gene Expression Pathways in Myelodysplastic Syndrome Hematopoietic Stem Cells
Leukemia (2010) 24, 756–764 & 2010 Macmillan Publishers Limited All rights reserved 0887-6924/10 $32.00 www.nature.com/leu ORIGINAL ARTICLE Deregulated gene expression pathways in myelodysplastic syndrome hematopoietic stem cells A Pellagatti1, M Cazzola2, A Giagounidis3, J Perry1, L Malcovati2, MG Della Porta2,MJa¨dersten4, S Killick5, A Verma6, CJ Norbury7, E Hellstro¨m-Lindberg4, JS Wainscoat1 and J Boultwood1 1LRF Molecular Haematology Unit, NDCLS, John Radcliffe Hospital, Oxford, UK; 2Department of Hematology Oncology, University of Pavia Medical School, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; 3Medizinische Klinik II, St Johannes Hospital, Duisburg, Germany; 4Division of Hematology, Department of Medicine, Karolinska Institutet, Stockholm, Sweden; 5Department of Haematology, Royal Bournemouth Hospital, Bournemouth, UK; 6Albert Einstein College of Medicine, Bronx, NY, USA and 7Sir William Dunn School of Pathology, University of Oxford, Oxford, UK To gain insight into the molecular pathogenesis of the the World Health Organization.6,7 Patients with refractory myelodysplastic syndromes (MDS), we performed global gene anemia (RA) with or without ringed sideroblasts, according to expression profiling and pathway analysis on the hemato- poietic stem cells (HSC) of 183 MDS patients as compared with the the French–American–British classification, were subdivided HSC of 17 healthy controls. The most significantly deregulated based on the presence or absence of multilineage dysplasia. In pathways in MDS include interferon signaling, thrombopoietin addition, patients with RA with excess blasts (RAEB) were signaling and the Wnt pathways. Among the most signifi- subdivided into two categories, RAEB1 and RAEB2, based on the cantly deregulated gene pathways in early MDS are immuno- percentage of bone marrow blasts. -

Systematic Screening for Potential Therapeutic Targets in Osteosarcoma Through a Kinome-Wide CRISPR-Cas9 Library
Cancer Biol Med 2020. doi: 10.20892/j.issn.2095-3941.2020.0162 ORIGINAL ARTICLE Systematic screening for potential therapeutic targets in osteosarcoma through a kinome-wide CRISPR-Cas9 library Yuanzhong Wu*, Liwen Zhou*, Zifeng Wang, Xin Wang, Ruhua Zhang, Lisi Zheng, Tiebang Kang Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou 510060, China ABSTRACT Objective: Osteosarcoma is the most common primary malignant bone tumor. However, the survival of patients with osteosarcoma has remained unchanged during the past 30 years, owing to a lack of efficient therapeutic targets. Methods: We constructed a kinome-targeting CRISPR-Cas9 library containing 507 kinases and 100 nontargeting controls and screened the potential kinase targets in osteosarcoma. The CRISPR screening sequencing data were analyzed with the Model-based Analysis of Genome-wide CRISPR/Cas9 Knockout (MAGeCK) Python package. The functional data were applied in the 143B cell line through lenti-CRISPR-mediated gene knockout. The clinical significance of kinases in the survival of patients with osteosarcoma was analyzed in the R2: Genomics Analysis and Visualization Platform. Results: We identified 53 potential kinase targets in osteosarcoma. Among these targets, we analyzed 3 kinases, TRRAP, PKMYT1, and TP53RK, to validate their oncogenic functions in osteosarcoma. PKMYT1 and TP53RK showed higher expression in osteosarcoma than in normal bone tissue, whereas TRRAP showed no significant difference. High expression of all 3 kinases was associated with relatively poor prognosis in patients with osteosarcoma. Conclusions: Our results not only offer potential therapeutic kinase targets in osteosarcoma but also provide a paradigm for functional genetic screening by using a CRISPR-Cas9 library, including target design, library construction, screening workflow, data analysis, and functional validation. -
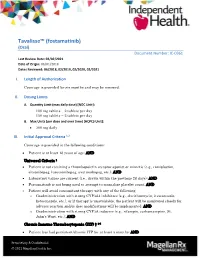
Tavalisse™ (Fostamatinib) (Oral) Document Number: IC-0361 Last Review Date: 02/02/2021 Date of Origin: 06/01/2018 Dates Reviewed: 06/2018, 02/2019, 02/2020, 02/2021
Tavalisse™ (fostamatinib) (Oral) Document Number: IC-0361 Last Review Date: 02/02/2021 Date of Origin: 06/01/2018 Dates Reviewed: 06/2018, 02/2019, 02/2020, 02/2021 I. Length of Authorization Coverage is provided for six months and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: 100 mg tablets – 2 tablets per day 150 mg tablets – 2 tablets per day B. Max Units (per dose and over time) [HCPCS Unit]: 300 mg daily III. Initial Approval Criteria 1,2 Coverage is provided in the following conditions: Patient is at least 18 years of age; AND Universal Criteria 1 Patient is not receiving a thrombopoietin receptor agonist or mimetic (e.g., romiplostim, eltrombopag, lusutrombopag, avatrombopag, etc.); AND Laboratory values are current (i.e., drawn within the previous 28 days); AND Fostamatinib is not being used to attempt to normalize platelet count; AND Patient will avoid concomitant therapy with any of the following: o Coadministration with strong CYP3A4 inhibitors (e.g., clarithromycin, itraconazole, ketoconazole, etc.), or if therapy is unavoidable, the patient will be monitored closely for adverse reaction and/or dose modifications will be implemented; AND o Coadministration with strong CYP3A inducers (e.g., rifampin, carbamazepine, St. John’s Wort, etc.); AND Chronic Immune Thrombocytopenia (ITP) † 1-5 Patient has had persistent/chronic ITP for at least 3 months; AND Proprietary & Confidential © 2021 Magellan Health, Inc. Patient has previously failed any of the following treatments for ITP: Patient has failed previous therapy with corticosteroids (i.e., patient had no response to at least a 3-month trial or is corticosteroid-dependent); OR Patient has failed previous therapy with immunoglobulins; OR Patient has had a splenectomy; OR Patient has failed previous therapy with a thrombopoietin receptor agonist; AND The patient is at increased risk for bleeding as indicated by platelet count of less than 30 × 109/L (30,000/mm³) † FDA Approved Indication(s) IV. -

Profiling Data
Compound Name DiscoveRx Gene Symbol Entrez Gene Percent Compound Symbol Control Concentration (nM) JNK-IN-8 AAK1 AAK1 69 1000 JNK-IN-8 ABL1(E255K)-phosphorylated ABL1 100 1000 JNK-IN-8 ABL1(F317I)-nonphosphorylated ABL1 87 1000 JNK-IN-8 ABL1(F317I)-phosphorylated ABL1 100 1000 JNK-IN-8 ABL1(F317L)-nonphosphorylated ABL1 65 1000 JNK-IN-8 ABL1(F317L)-phosphorylated ABL1 61 1000 JNK-IN-8 ABL1(H396P)-nonphosphorylated ABL1 42 1000 JNK-IN-8 ABL1(H396P)-phosphorylated ABL1 60 1000 JNK-IN-8 ABL1(M351T)-phosphorylated ABL1 81 1000 JNK-IN-8 ABL1(Q252H)-nonphosphorylated ABL1 100 1000 JNK-IN-8 ABL1(Q252H)-phosphorylated ABL1 56 1000 JNK-IN-8 ABL1(T315I)-nonphosphorylated ABL1 100 1000 JNK-IN-8 ABL1(T315I)-phosphorylated ABL1 92 1000 JNK-IN-8 ABL1(Y253F)-phosphorylated ABL1 71 1000 JNK-IN-8 ABL1-nonphosphorylated ABL1 97 1000 JNK-IN-8 ABL1-phosphorylated ABL1 100 1000 JNK-IN-8 ABL2 ABL2 97 1000 JNK-IN-8 ACVR1 ACVR1 100 1000 JNK-IN-8 ACVR1B ACVR1B 88 1000 JNK-IN-8 ACVR2A ACVR2A 100 1000 JNK-IN-8 ACVR2B ACVR2B 100 1000 JNK-IN-8 ACVRL1 ACVRL1 96 1000 JNK-IN-8 ADCK3 CABC1 100 1000 JNK-IN-8 ADCK4 ADCK4 93 1000 JNK-IN-8 AKT1 AKT1 100 1000 JNK-IN-8 AKT2 AKT2 100 1000 JNK-IN-8 AKT3 AKT3 100 1000 JNK-IN-8 ALK ALK 85 1000 JNK-IN-8 AMPK-alpha1 PRKAA1 100 1000 JNK-IN-8 AMPK-alpha2 PRKAA2 84 1000 JNK-IN-8 ANKK1 ANKK1 75 1000 JNK-IN-8 ARK5 NUAK1 100 1000 JNK-IN-8 ASK1 MAP3K5 100 1000 JNK-IN-8 ASK2 MAP3K6 93 1000 JNK-IN-8 AURKA AURKA 100 1000 JNK-IN-8 AURKA AURKA 84 1000 JNK-IN-8 AURKB AURKB 83 1000 JNK-IN-8 AURKB AURKB 96 1000 JNK-IN-8 AURKC AURKC 95 1000 JNK-IN-8 -

Blood Modifier Agents Policy #: Rx.01.208
Pharmacy Policy Bulletin Title: Blood Modifier Agents Policy #: Rx.01.208 Application of pharmacy policy is determined by benefits and contracts. Benefits may vary based on product line, group, or contract. Some medications may be subject to precertification, age, quantity, or formulary restrictions (ie limits on non-preferred drugs). Individual member benefits must be verified. This pharmacy policy document describes the status of pharmaceutical information and/or technology at the time the document was developed. Since that time, new information relating to drug efficacy, interactions, contraindications, dosage, administration routes, safety, or FDA approval may have changed. This Pharmacy Policy will be regularly updated as scientific and medical literature becomes available. This information may include new FDA-approved indications, withdrawals, or other FDA alerts. This type of information is relevant not only when considering whether this policy should be updated, but also when applying it to current requests for coverage. Members are advised to use participating pharmacies in order to receive the highest level of benefits. Intent: The intent of this policy is to communicate the medical necessity criteria for eltrombopag olamine (Promacta®), fostamatinib disodium (Tavalisse™), avatrombopag (Doptelet®), lusutrombopag (Mulpleta®) as provided under the member's prescription drug benefit. Description: Idiopathic thrombocytopenia purpura (ITP): ITP is an immune disorder in which the blood doesn't clot normally. ITP can cause excessive bruising and bleeding and can be characterized as an unusually low level of platelets, or thrombocytes, in the blood results in ITP. Thrombocytopenia in patients with hepatitis C: Thrombocytopenia can occur in patients with chronic hepatitis C virus (HCV) infection. -

Circrna-006258 Sponge-Adsorbs Mir-574-5P to Regulate Cell Growth and Milk Synthesis Via EVI5L in Goat Mammary Epithelial Cells
G C A T T A C G G C A T genes Article CircRNA-006258 Sponge-Adsorbs miR-574-5p to Regulate Cell Growth and Milk Synthesis via EVI5L in Goat Mammary Epithelial Cells Meng Zhang y , Li Ma y, Yuhan Liu, Yonglong He, Guang Li, Xiaopeng An and Binyun Cao * College of Animal Science and Technology, Northwest A&F University, Yangling 712100, Shanxi, China; [email protected] (M.Z.); [email protected] (L.M.); [email protected] (Y.L.); [email protected] (Y.H.); [email protected] (G.L.); [email protected] (X.A.) * Correspondence: [email protected]; Tel.: +86-29-87092102 These authors contributed equally to this work. y Received: 28 May 2020; Accepted: 25 June 2020; Published: 28 June 2020 Abstract: The development of the udder and the milk yield are closely related to the number and vitality of mammary epithelial cells. Many previous studies have proved that non-coding RNAs (ncRNAs) are widely involved in mammary gland development and the physiological activities of lactation. Our laboratory previous sequencing data revealed that miR-574-5p was differentially expressed during the colostrum and peak lactation stages, while the molecular mechanism of the regulatory effect of miR-574-5p on goat mammary epithelial cells (GMECs) is unclear. In this study, the targeting relationship was detected between miR-574-5p or ecotropic viral integration site 5-like (EVI5L) and circRNA-006258. The results declared that miR-574-5p induced the down-regulation of EVI5L expression at both the mRNA and protein levels, while circRNA-006258 relieved the inhibitory effect through adsorbing miR-574-5p. -

Farmaatsia- Terminoloogia Teine, Täiendatud Trükk
Farmaatsia- terminoloogia Teine, täiendatud trükk Graanulid Suspensioon Lahus Emulsioon Pillid Pulber Salv Kreem Aerosool Plaaster Sprei Pastill Tampoon Oblaat Emulsioon Kontsentraat Silmageel Tablett Haavapulk Ninatilgad Kapsel Lakukivi Inhalaator Farmaatsia- terminoloogia Teine, täiendatud trükk Tartu 2019 Koostajad: Toivo Hinrikus, Karin Kogermann, Ott Laius, Signe Leito, Ain Raal, Andres Soosaar, Triin Teppor, Daisy Volmer Keeletoimetaja: Tiina Kuusk Kirjastanud: Ravimiamet Nooruse 1, 50411 Tartu Telefon: +372 737 4140 Faks: +372 737 4142 E-post: [email protected] Esimene trükk 2010 Teine, täiendatud trükk 2019 Raamat on leitav Ravimiameti veebilehelt: www.ravimiamet.ee/farmaatsiaterminoloogia Väljaande refereerimisel või tsiteerimisel palume viidata allikale. ISBN 978-9949-9697-3-9 Sisukord Farmaatsiaterminoloogia Eestis..........................................................................................5 Üldised farmaatsiaalased terminid ...................................................................................10 Euroopa farmakopöa ......................................................................................................... 21 Euroopa farmakopöa sõnastik ..........................................................................................24 Standardterminid ..............................................................................................................29 Ravimvormid .....................................................................................................................29 -

Frequent Somatic Mutations in MAP3K5 and MAP3K9 in Metastatic Melanoma Identified by Exome Sequencing
LETTERS Frequent somatic mutations in MAP3K5 and MAP3K9 in metastatic melanoma identified by exome sequencing Mitchell S Stark1,9, Susan L Woods1,9, Michael G Gartside1,9, Vanessa F Bonazzi1,9, Ken Dutton-Regester1,2,9, Lauren G Aoude1,3, Donald Chow4, Chris Sereduk4, Natalie M Niemi5, Nanyun Tang4, Jonathan J Ellis6, Jeffrey Reid7, Victoria Zismann4, Sonika Tyagi1, Donna Muzny7, Irene Newsham7, YuanQing Wu7, Jane M Palmer1, Thomas Pollak1, David Youngkin4, Bradford R Brooks5, Catherine Lanagan1, Christopher W Schmidt1, Bostjan Kobe6, Jeffrey P MacKeigan5, Hongwei Yin4, Kevin M Brown4,8, Richard Gibbs7, Jeffrey Trent4,5 & Nicholas K Hayward1 We sequenced eight melanoma exomes to identify new Using whole-exome capture, we sequenced eight melanoma cell lines somatic mutations in metastatic melanoma. Focusing on (Supplementary Table 1) and matched normal lymphoblastoid cell the mitogen-activated protein (MAP) kinase kinase kinase lines (LCLs) using two NGS platforms (Illumina Genome Analyzer II (MAP3K) family, we found that 24% of melanoma cell and Life Technologies SOLiD) and mapped reads with platform- lines have mutations in the protein-coding regions of either appropriate alignment programs (Online Methods). The schematic of MAP3K5 or MAP3K9. Structural modeling predicted that how the analysis was performed is shown in Supplementary Figure 1. mutations in the kinase domain may affect the activity To maximize the chance of finding bona fide mutations, we applied and regulation of these protein kinases. The position of strict filtering criteria (described in Supplementary Fig. 1 and in the the mutations and the loss of heterozygosity of MAP3K5 Online Methods) to minimize the false positive rate without overly and MAP3K9 in 85% and 67% of melanoma samples, inflating the false negative rate. -

New Drug Evaluation Monograph Template
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-2596 Drug Class Review: Thrombocytopenia Date of Review: January 2019 End Date of Literature Search: 11/05/2018 Purpose for Class Review: Treatments for thrombocytopenia are being reviewed for the first time, prompted by the recent approval of three new drugs; avatrombopag (Doptelet®), fostamatinib (Tavalisse™) and lusutrombopag (Mulpleta®). Research Questions: 1. What is the evidence for efficacy and harms of thrombocytopenia treatments (avatrombopag, eltrombopag, lusutrombopag, fostamatinib, and romiplostim)? 2. Is there any comparative evidence for therapies for thrombocytopenia pertaining to important outcomes such as mortality, bleeding rates, and platelet transfusions? 3. Is there any comparative evidence based on the harms outcomes of thrombocytopenia treatments? 4. Are there subpopulations of patients for which specific thrombocytopenia therapies may be more effective or associated with less harm? Conclusions: Three guidelines, six randomized clinical trials and five high-quality systematic reviews and meta-analyses met inclusion criteria for this review. There was insufficient direct comparative evidence between different therapies to treat thrombocytopenia. A majority of trials were small and of short duration. Guidelines recommend corticosteroids and intravenous immunoglobulin (IVIg) as first-line therapy for most adults with idiopathic thrombocytopenia (ITP). Thrombopoietin receptor agonists (TPOs) and the tyrosine kinase inhibitor, fostamatinib, are recommended as second-line treatments after failure of at least one other treatment.1–3 Avatrombopag and lusutrombopag are only approved for short-term use before procedures in patients with chronic liver failure. -

PRODUCTS and SERVICES Target List
PRODUCTS AND SERVICES Target list Kinase Products P.1-11 Kinase Products Biochemical Assays P.12 "QuickScout Screening Assist™ Kits" Kinase Protein Assay Kits P.13 "QuickScout Custom Profiling & Panel Profiling Series" Targets P.14 "QuickScout Custom Profiling Series" Preincubation Targets Cell-Based Assays P.15 NanoBRET™ TE Intracellular Kinase Cell-Based Assay Service Targets P.16 Tyrosine Kinase Ba/F3 Cell-Based Assay Service Targets P.17 Kinase HEK293 Cell-Based Assay Service ~ClariCELL™ ~ Targets P.18 Detection of Protein-Protein Interactions ~ProbeX™~ Stable Cell Lines Crystallization Services P.19 FastLane™ Structures ~Premium~ P.20-21 FastLane™ Structures ~Standard~ Kinase Products For details of products, please see "PRODUCTS AND SERVICES" on page 1~3. Tyrosine Kinases Note: Please contact us for availability or further information. Information may be changed without notice. Expression Protein Kinase Tag Carna Product Name Catalog No. Construct Sequence Accession Number Tag Location System HIS ABL(ABL1) 08-001 Full-length 2-1130 NP_005148.2 N-terminal His Insect (sf21) ABL(ABL1) BTN BTN-ABL(ABL1) 08-401-20N Full-length 2-1130 NP_005148.2 N-terminal DYKDDDDK Insect (sf21) ABL(ABL1) [E255K] HIS ABL(ABL1)[E255K] 08-094 Full-length 2-1130 NP_005148.2 N-terminal His Insect (sf21) HIS ABL(ABL1)[T315I] 08-093 Full-length 2-1130 NP_005148.2 N-terminal His Insect (sf21) ABL(ABL1) [T315I] BTN BTN-ABL(ABL1)[T315I] 08-493-20N Full-length 2-1130 NP_005148.2 N-terminal DYKDDDDK Insect (sf21) ACK(TNK2) GST ACK(TNK2) 08-196 Catalytic domain -

Nplate® (Romiplostim)
Nplate® (romiplostim) (Subcutaneous) Document Number: IC-0089 Last Review Date: 02/02/2021 Date of Origin: 01/01/2012 Dates Reviewed: 12/2011, 02/2013, 02/2014, 12/2014, 10/2015, 09/2016, 12/2016, 03/2017, 06/2017, 12/2017, 03/2018, 06/2018, 10/2018, 01/2019, 12/2019, 02/2020, 02/2021 I. Length of Authorization Coverage will be provided for 3 months and may be renewed, unless otherwise specified. • Coverage for use to treat Hematopoietic Syndrome of Acute Radiation Syndrome (HSARS) cannot be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: − Nplate 125 mcg SDV for injection: 4 vials per 28 days − Nplate 250 mcg SDV for injection: 20 vials per 28 days − Nplate 500 mcg SDV for injection: 12 vials per 28 days B. Max Units (per dose and over time) [HCPCS Unit]: • ITP: 125 billable units weekly • MDS: 100 billable units weekly • HSARS: 125 billable units x 1 dose III. Initial Approval Criteria 1,3,13,14 Coverage is provided in the following conditions: Universal Criteria 1 • Patient is not on any other thrombopoietin receptor agonist or mimetic (e.g., lusutrombopag, eltrombopag, avatrombopag, etc.) or fostamatinib; AND • Must not be used in an attempt to normalize platelet counts; AND • Laboratory value for platelet count is current (i.e., drawn within the previous 28 days); AND Immune (idiopathic) thrombocytopenia (ITP) † Ф 1,412 Proprietary & Confidential © 2021 Magellan Health, Inc. • The patient is at increased risk for bleeding as indicated by platelet count less than 30 × 109/L (30,000/mm³); AND o Patient has acute ITP; AND . -

Fostamatinib
Drug and Biologic Coverage Policy Effective Date ............................................ 8/1/2021 Next Review Date… ..................................... 8/1/2022 Coverage Policy Number ............................... IP0154 Fostamatinib Table of Contents Related Coverage Resources Overview .............................................................. 1 Immune Globulin Medical Necessity Criteria ................................... 1 Rituximab for Non-Oncology Indications Reauthorization Criteria ....................................... 2 Authorization Duration ......................................... 2 Conditions Not Covered....................................... 2 Background .......................................................... 3 References .......................................................... 3 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard