Post-Exposure Prophylaxis (PEP) for Human Immunodeficiency Virus (HIV) and Guidance for Staff on the Management of Community Exposure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Emergency Department Activity
NHS Scotland - Emergency Department Activity Attendances and Performance against the 4-hour Waiting Time Standard This is an ISD Scotland National Statistics release. The Scottish Government waiting time standard for emergency departments is that 98 % of all attendances should be seen within 4 hours. The figures presented in these tables detail the performance of each individual site and NHS board against the standard. Time Period: Apr-10 to Mar-11 Source: A&E data mart, ISD Scotland Date: 07 May 2012 List of Tables Table 1: Attendances and performance against 4-hour standard, Apr-10 to Mar-11 Total attendances, number of attendances breaching standard and attendances meeting standard (number and percentage). Figures are given at site and NHS Board level. Table 2: Attendances, Apr-10 to Mar-11 Summary table of attendances only. Figures are given at site and NHS Board level. Table 3: Performance against 4-hour standard, Apr-10 to Mar-11 Summary table of percentage of attendances meeting standard. Figures are given at site and NHS Board level. Notes: 1) The waiting time is defined as the time of arrival until the time of discharge, admission or transfer. 2) New presentations only; excludes planned return and recall attendances. 3) There are two types of site that provide emergency care; • ED - Emergency Departments; sites that provide a 24 hour emergency medicine consultant led service • MIU/Other - sites including minor injuries units (MIU), small hospitals and health centres in rural areas that carry out emergency department related activity and are GP or Nurse led. They may or may not be open 24 hours. -

Contract Between Scottish Ministers
CONTRACT BETWEEN SCOTTISH MINISTERS AND GEOAMEY PECS LTD FOR THE SCOTTISH COURT CUSTODY AND PRISONER ESCORT SERVICE (SCCPES) REFERENCE: 01500 MARCH 2018 Official No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of SPS and will be returned upon request. 1 | P a g e 01500 Scottish Court Custody and Prisoner Escort Service (SCCPES) FORM OF CONTRACT CONTRACT No. 01500 This Contract is entered in to between: The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service at the: Scottish Prison Service Calton House 5 Redheughs Rigg Edinburgh EH12 9HW (hereinafter called the “Purchaser”) OF THE FIRST PART And GEOAmey PECS Ltd (07556404) The Sherard Building, Edmund Halley Road Oxford OX4 4DQ (hereinafter called the “Service Provider”) OF THE SECOND PART The Purchaser hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Purchaser, the Services (as hereinafter defined) on the Conditions of Contract set out in this Contract. The Purchaser agrees to pay to the Service Provider the relevant sums specified in Schedule C and due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Purchaser for the due performance of the Contract and the Purchaser will be entitled to enforce this Contract on behalf of the Scottish Ministers. -

Turn to Your Dentist
WHEN YOU ARE ILL OR INJURED KNOW WHO TO TURN TO. SELF CARE PHARMACIST GP www.know-who-to-turn-to.com This publication is also available in large print NHS OUT OF OPTICIAN SELF MANAGEMENT and on computer disk. Other formats and HOURS SERVICE OPTOMETRIST languages can be supplied on request. Please call Equality and Diversity on 01224 551116 or 552245 or email [email protected] Ask for publication CGD 150869 December 2015 MINOR DENTIST MENTAL HEALTH INJURIES UNIT SELF CARE 4 - 5 PHARMACIST 6 - 7 WHEN YOU’RE ILL MENTAL HEALTH 8 - 9 GP 10 - 11 OR INJURED KNOW NHS OUT OF HOURS SERVICE 12 - 13 WHO TO TURN TO. SELF MANAGEMENT 14 - 15 www.know-who-to-turn-to.com OPTICIAN / OPTOMETRIST 16 - 17 This booklet has been produced to help you get the right DENTIST 18 - 19 medical assistance when you’re ill or injured. There are ten options to choose from. MINOR INJURIES UNIT 20 - 21 A&E / 999 22 - 23 Going directly to the person with the appropriate skills is important. This can help you to a speedier recovery and makes sure all NHS services are run efficiently. The following sections of this booklet give examples of common conditions, and provide information on who to turn to. Remember, getting the right help is in your hands. So please keep this booklet handy, and you’ll always know who to turn to when you’re ill or injured. Further information on all of the above services can be found at www.know-who-to-turn-to.com HANGOVER. -

Support Directory for Families, Authority Staff and Partner Agencies
1 From mountain to sea Aberdeenshirep Support Directory for Families, Authority Staff and Partner Agencies December 2017 2 | Contents 1 BENEFITS 3 2 CHILDCARE AND RESPITE 23 3 COMMUNITY ACTION 43 4 COMPLAINTS 50 5 EDUCATION AND LEARNING 63 6 Careers 81 7 FINANCIAL HELP 83 8 GENERAL SUPPORT 103 9 HEALTH 180 10 HOLIDAYS 194 11 HOUSING 202 12 LEGAL ASSISTANCE AND ADVICE 218 13 NATIONAL AND LOCAL SUPPORT GROUPS (SPECIFIC CONDITIONS) 223 14 SOCIAL AND LEISURE OPPORTUNITIES 405 15 SOCIAL WORK 453 16 TRANSPORT 458 SEARCH INSTRUCTIONS 1. Right click on the document and select the word ‘Find’ (using a left click) 2. A dialogue box will appear at the top right hand side of the page 3. Enter the search word to the dialogue box and press the return key 4. The first reference will be highlighted for you to select 5. If the first reference is not required, return to the dialogue box and click below it on ‘Next’ to move through the document, or ‘previous’ to return 1 BENEFITS 1.1 Advice for Scotland (Citizens Advice Bureau) Information on benefits and tax credits for different groups of people including: Unemployed, sick or disabled people; help with council tax and housing costs; national insurance; payment of benefits; problems with benefits. http://www.adviceguide.org.uk 1.2 Attendance Allowance Eligibility You can get Attendance Allowance if you’re 65 or over and the following apply: you have a physical disability (including sensory disability, e.g. blindness), a mental disability (including learning difficulties), or both your disability is severe enough for you to need help caring for yourself or someone to supervise you, for your own or someone else’s safety Use the benefits adviser online to check your eligibility. -

Emergency Departments
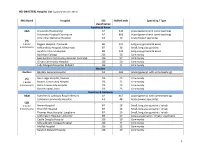
ED Site List 220711 v2.xls NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care File NHS Board Site Type Location Name Location Address Comments Type Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG -

Emergency Departments
ED-site-list NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care NHS Board Site Type Location Name Location Address File Type Comments Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG A Forth Valley -

When You're Ill, Know Who to Turn
SELF CARE WHEN YOU’RE PHARMACIST ILL, GP KNOW WHO NHS TO OUT OF HOURS SERVICE TURN MINOR TO. INJURIES UNIT A&E / 999 EMERGENCY SERVICE This booklet has been produced to help you get the right medical assistance when you’re ill or injured. There are six options to choose from. WHEN SELF CARE 4-5 YOU’RE ILL, PHARMACIST 6-7 GP 8-9 KNOW NHS OUT OF HOURS SERVICE 10 -11 WHO TO MINOR INJURIES UNIT 12 -13 TURN TO. A&E / 999 14 -15 www.know-who-to-turn-to.com Going directly to the person with the appropriate skills is important. This can help you to a speedier recovery and makes sure all NHS services are run efficiently. The following sections of this booklet give examples of common conditions, and provide information on who to turn to. Remember, getting the right help is in your hands. So please keep this booklet handy, and you’ll always know who to turn to when you’re ill or injured. Further information on all of the above services can be found at www.know-who-to-turn-to.com HANGOVER. GRAZED KNEE. SORE THROAT. COUGHS AND COLDS. TURN TO SELF CARE. For a speedy recovery, self care is the best option when you have a minor illness or injury. A well-stocked medicine cabinet means you’ll receive the right treatment immediately. You can find out more about illnesses, health related services and what to keep in your medicine cabinet by visiting www.know-who-to-turn-to.com Or you can call our free healthline on 0500 20 20 30. -

Public Consultations Template
Public Involvement Update Report Engagement & Participation Committee - February 2017 Contents page/s Multicultural Health and Wellbeing Forum 3 - 7 ‘Breaking the Silence’ – Domestic Violence in a Faith Context 3 Mindfullness Monday 5 Ethnic Minority Forum (EMF) – ‘Spotlight on the Polish Community’ 6 Holocaust Memorial Day 6 Multicultural Movie Night 7 Integration of Health and Social Care, Aberdeen City 8 - 11 ABCD Seaton Event 8 Continuing our ABCD Story 9 Aberdeen West Locality Leadership Group 9 Modernising Primary Care 10 Adult Mental Health Service Redesign 11 ------------------------------------------------------------------------------------------------------------------------ Keith and Speyside Pathfinder Project 12 Scottish Health Council Review 12 Monitoring of Cleaning Services 13 ------------------------------------------------------------------------------------------------------------------------ The Baird Family Hospital and The ANCHOR Centre 13 - 15 ------------------------------------------------------------------------------------------------------------------------ ViewPoint 16 Move of the ENT Head and Neck Outpatient Department and Audiology and Hearing Aid Services to Woodend Hospital 16 Revised map of the Woodend Hospital site 16 Primary Care: 16 Pre-application joint public consultation on a proposal to open a new community in Pitmedden 16 Changes at Northfield and Mastrick Medical Practice 17 An Caorann Medical Practice 17 Review of dispensing GP practices 18 Acute Care 18 ------------------------------------------------------------------------------------------------------------------------ -

ROH Representative Policy
Policy on Supplier Representatives Policy author Matthew Revell Accountable Executive Lead Jonathan Lofthouse Approving body Policy reference ROH/XXX/NNN [Assigned by Governance Team] POLICY APPROVAL DATE: ESSENTIAL READING FOR THE FOLLOWING STAFF GROUPS: May 2017 1 – All Trust Staff working in Theatres and Pharmacy POLICY 2 – Staff working in partnership with supplier IMPLEMENTATION DATE: representatives June 2016 DATE POLICY TO STAFF GROUPS WHICH SHOULD BE AWARE OF THE POLICY FOR BE REVIEWED: REFERENCE PURPOSES: June 2017 1 – Staff involved with purchasing or procurement DOCUMENT CONTROL AND HISTORY Version Date Date of Next Reason for change (e.g. full rewrite, No Approved implementation Review amendment to reflect new legislation, Date updated flowchart, etc.) 1 June 2017 New Policy Policy on Supplier Representation April 2017 2 | P a g e Policy on Supplier Representatives KEY POINTS 1. Supplier Representatives must not enter any area without an appointment. 2. Supplier Representatives must be registered on the Medical Industry Accredited System. 3. If the meeting is to discuss ANY new product or service then Procurement and Supplies must be informed. 4. Cold calling is not acceptable. 5. Pharmacy representatives must report to Pharmacy. 6. No electro-medical equipment can be used until tested by EBME. 7. Representatives visiting Theatre areas must comply with the Theatre protocol. 8. No sample products can be trialed until the appropriate trials and indemnity documentation has been completed. 9. Contractors undertaking work on the Trust’s sites must adhere to the Control of Contractors Policy. Do’s and Don’ts Do meet the supplier representative at an arranged point and don’t allow them to wander around clinical areas unaccompanied. -
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St. -

Etterkommere Av David Galt 07 Apr 2003
Etterkommere av David Galt 07 apr 2003 David Galt Catherine Mair Født: 1836 Født: 1843 Død: 8 aug 1917, 3 Fountain Street, Banff Død: 27 mai 1925, 3 Fountain Street, Banff George Gault Margaret Jane Gordon Goodbrand Født: 7 apr 1875, Painted Effie, Banff Født: 12 jan 1881, Whitehills, Parish of Død: 1952 Boyndie Død: 10 okt 1923, Chalmers Hospital, Banff Jessie Gault Johan Hilding Andersen Født: 18 aug 1919, 1 Fountain Street, Banff, Født: 7 jul 1915, Fagerholt, Idd Scotland Død: 1 mai 1986, Furuset sykehjem, Oslo Død: 11 apr 1999, Sagene sykehjem, Oslo Ivar George Gault Født: 19 feb 1947, Sarpsborg sykehus Dåp: 11 mai 1947, Tune kirke Lorna Irene Andersen Villy Storborg Født: 13 mai 1950, Ullevål sykehus, Oslo Født: 26 mai 1950, Betanien sykehus, Oslo Hilde Storborg Ole Jakob Hundstad Født: 18 jul 1972, Aker sykehus, Oslo Født: 25 sep 1971, Horten sykehus Mari Hundstad Født: 20 apr 2001, Ullevål sykehus, Oslo Nancy Azora Andersen Født: jul 1944, Scotland Død: 24 des 1944, Scotland Alexander Gault Elizabeth Sutherland Mcgregor Født: 9 sep 1913, 1 Fountain Street, Banff, Født: 17 des 1913 Scotland Død: 19 jun 1996, Glenesk Nursing Home, Død: 20 sep 1994, Royal Infirmary, Aberdeen Turriff, AB53 8AH. Alexander Gault Robyn Jones Født: 25 nov 1935, 9 Low Street, Portsoy Født: 18 jan 1947 Alistair Alexander Gault Født: 1967 Fiona Kathleen Gault James Matthew Gauci Født: 1969 Publisert av Ivar Gault, Øvrefoss 14, 0555 Oslo Side 1 Etterkommere av David Galt 07 apr 2003 Regan Kathleen Gauci Født: jun 1993 Alec James Gauci Født: apr 1995 Maddison -

Scotland) 15 June 2021
Version 1.6 (Scotland) 15 June 2021 ISARIC/WHO Clinical Characterisation Protocol UK (Scotland) Recruitment Procedures for FRONTLINE CLINICAL RESEARCH STAFF The most up to date versions of the protocol and case report form are available at isaric4c.net/protocols/ A virtual site visit is available at isaric4c.net/virtual_site_visit/ AIM: Please recruit the following patients only: • Vaccine failure (positive COVID test - rather than displaying symptoms – >28d after having received a vaccine) • Reinfection (proven after proven) • Co-infection (flu/RSV) • COVID associated hyper inflammation (MIS-A/MIS-C/PINS-TS) at any age • Samples from patients with pathogens of public health interest including people identified as infected with SARS-CoV “variants of concern” • All children CONSENT: once the form is signed by a participant it is hazardous. To record consent, we suggest an independent witness observes the completed form then signs a fresh copy outside of the isolation area. Consent can also be obtained by telephone from participants or from relatives for proxy consent. RECRUITMENT PACKS: Sample collection kits will be supplied to sites. Sample collections kits can be requested from: [email protected] Each kit will have a specific kit ID number, with each component within showing this kit ID and its own respective component ID for audit purposes. Pods and bio-bags for shipping will also be supplied to sites. These can be requested from [email protected] OBTAIN SAMPLES according to the schedule. You can find out which tier you are operating at in the front page of the site file. If you have capacity to recruit at TIER 2: Day 1 2 3 4 5 6 7 8 9 28 days after discharge Samples R S S C Sample priority 1 2 3 4 R: recruitment sample; S: serial sample; C: convalescent sample.