Neuronal and Immunological Basis of Action of Antidepressants in Chronic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Summary of Product Characteristics
Package leaflet: Information for the patient Fluoxetine 20mg Capsules, hard fluoxetine Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. • Keep this leaflet. You may need to read it again. • If you have further questions, ask your doctor or pharmacist. • This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. •If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. What is in this leaflet 1. What Fluoxetine is and what it is used for 2. What you need to know before you take Fluoxetine 3. How to take Fluoxetine 4. Possible side effects 5. How to store Fluoxetine 6. Contents of the pack and other information 1. What Fluoxetine is and what it is used for The name of your medicine is Fluoxetine 20mg Capsules, hard. It contains the active substance fluoxetine. Fluoxetine belongs to a group of medicines called selective serotonin reuptake inhibitor (SSRI) antidepressants. Fluoxetine can be given to treat the following conditions: Adults: • Major depressive episodes • The symptoms of a condition called obsessive-compulsive disorder (OCD). • The eating disorder bulimia nervosa. This medicine is used alongside psychotherapy for the reduction of binge-eating and purging. Children and adolescents aged 8 years and above: • Moderate to severe major depressive disorder, if the depression does not respond to psychological therapy after 4-6 sessions. Fluoxetine should be offered to a child or young person with moderate to severe major depressive disorder only in combination with psychological therapy. -

Tramadol (Ultram)
TRAMADOL (ULTRAM) Tramadol is FDA approved for the treatment of musculoskeletal pain. Studies have shown it is useful in treating the pain associated with diabetic neuropathy and other pain conditions. Tramadol comes in 50 mg tablets. The maximum dose is two tablets four times per day unless your kidney function is below normal or you are over 75 years old, in which case the maximum dose is two tablets three times per day. The main side effects of Tramadol are drowsiness, sedation, and stomach upset, all of which are minimized by slowly raising the dose. About 5% of patients have stomach upset at any dose of Tramadol and cannot take the medicine. Other risks include seizures (occur in less than 1/100,000 and are more likely if you have seizures) and possibly abuse (relevant if you have abused drugs in the past). Tramadol should be started at a low dose and raise the dose slowly toward the maximum dose. Start with one tablet at bedtime. After 3 - 7 days, increase to one tablet twice daily (morning and bedtime). After an additional 3 - 7 days, increase to one tablet three times per day (morning, noon, and bedtime). After an additional 3 - 7 days, increase to one tablet four times per day (1 tablet with each meal and 1 at bedtime). At that point, the dose may be increased or adjusted depending on how you are doing. To increase further, you will: Add a second tablet at bedtime (one tablet three times per day and two tablets at bedtime). After 3 - 7 days, add a second tablet to another dose (one tablet twice per day and two tablets twice per day). -

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

Interplay Between Gating and Block of Ligand-Gated Ion Channels
brain sciences Review Interplay between Gating and Block of Ligand-Gated Ion Channels Matthew B. Phillips 1,2, Aparna Nigam 1 and Jon W. Johnson 1,2,* 1 Department of Neuroscience, University of Pittsburgh, Pittsburgh, PA 15260, USA; [email protected] (M.B.P.); [email protected] (A.N.) 2 Center for Neuroscience, University of Pittsburgh, Pittsburgh, PA 15260, USA * Correspondence: [email protected]; Tel.: +1-(412)-624-4295 Received: 27 October 2020; Accepted: 26 November 2020; Published: 1 December 2020 Abstract: Drugs that inhibit ion channel function by binding in the channel and preventing current flow, known as channel blockers, can be used as powerful tools for analysis of channel properties. Channel blockers are used to probe both the sophisticated structure and basic biophysical properties of ion channels. Gating, the mechanism that controls the opening and closing of ion channels, can be profoundly influenced by channel blocking drugs. Channel block and gating are reciprocally connected; gating controls access of channel blockers to their binding sites, and channel-blocking drugs can have profound and diverse effects on the rates of gating transitions and on the stability of channel open and closed states. This review synthesizes knowledge of the inherent intertwining of block and gating of excitatory ligand-gated ion channels, with a focus on the utility of channel blockers as analytic probes of ionotropic glutamate receptor channel function. Keywords: ligand-gated ion channel; channel block; channel gating; nicotinic acetylcholine receptor; ionotropic glutamate receptor; AMPA receptor; kainate receptor; NMDA receptor 1. Introduction Neuronal information processing depends on the distribution and properties of the ion channels found in neuronal membranes. -

From NMDA Receptor Hypofunction to the Dopamine Hypothesis of Schizophrenia J
REVIEW The Neuropsychopharmacology of Phencyclidine: From NMDA Receptor Hypofunction to the Dopamine Hypothesis of Schizophrenia J. David Jentsch, Ph.D., and Robert H. Roth, Ph.D. Administration of noncompetitive NMDA/glutamate effects of these drugs are discussed, especially with regard to receptor antagonists, such as phencyclidine (PCP) and differing profiles following single-dose and long-term ketamine, to humans induces a broad range of exposure. The neurochemical effects of NMDA receptor schizophrenic-like symptomatology, findings that have antagonist administration are argued to support a contributed to a hypoglutamatergic hypothesis of neurobiological hypothesis of schizophrenia, which includes schizophrenia. Moreover, a history of experimental pathophysiology within several neurotransmitter systems, investigations of the effects of these drugs in animals manifested in behavioral pathology. Future directions for suggests that NMDA receptor antagonists may model some the application of NMDA receptor antagonist models of behavioral symptoms of schizophrenia in nonhuman schizophrenia to preclinical and pathophysiological research subjects. In this review, the usefulness of PCP are offered. [Neuropsychopharmacology 20:201–225, administration as a potential animal model of schizophrenia 1999] © 1999 American College of is considered. To support the contention that NMDA Neuropsychopharmacology. Published by Elsevier receptor antagonist administration represents a viable Science Inc. model of schizophrenia, the behavioral and neurobiological KEY WORDS: Ketamine; Phencyclidine; Psychotomimetic; widely from the administration of purportedly psychot- Memory; Catecholamine; Schizophrenia; Prefrontal cortex; omimetic drugs (Snyder 1988; Javitt and Zukin 1991; Cognition; Dopamine; Glutamate Jentsch et al. 1998a), to perinatal insults (Lipska et al. Biological psychiatric research has seen the develop- 1993; El-Khodor and Boksa 1997; Moore and Grace ment of many putative animal models of schizophrenia. -

Designing Inhibitors Via Molecular Modelling Methods for Monoamine Oxidase Isozymes a and B Filiz Varnali Kadir Has Universit
DESIGNING INHIBITORS VIA MOLECULAR MODELLING METHODS FOR MONOAMINE OXIDASE ISOZYMES A AND B FİLİZ VARNALI KADİR HAS UNIVERSITY 2012 DESIGNING INHIBITORS VIA MOLECULAR MODELLING METHODS FOR MONOAMINE OXIDASE ISOZYMES A AND B FİLİZ VARNALI M.S. in Computational Biology and Bioinformatics, Kadir Has University, 2012 Submitted to the Graduate School of Science and Engineering in partial fulfilment of the requirements for the degree of Master of Science in Computational Biology and Bioinformatics KADİR HAS UNIVERSITY 2012 DESIGNING INHIBITORS VIA MOLECULAR MODELING METHODS FOR MONOAMINE OXIDASE ISOZYMES A AND B Abstract In drug development studies, a large number of new drug candidates (leads) have to be synthesized and optimized by changing several moieties of the leads in order to increase efficacies and decrease toxicities. Each synthesis of these new drug candidates include multi-steps procedures. Overall, discovering a new drug is a very time-consuming and very costly works. The development of molecular modelling programs and their applications in pharmaceutical research have been formalized as a field of study known computer assisted drug design (CADD) or computer assisted molecular design (CAMD). In this study, using the above techniques, Monoamine Oxidase isozymes, which play an essential role in the oxidative deamination of the biogenic amines, were studied. Compounds that inhibit these isozymes were shown to have therapeutic value in a variety of conditions including several psychiatric and neurological as well as neurodegenerative diseases. First, a series of new pyrazoline derivatives were screened using molecular modelling and docking methods and promising lead compounds were selected, and proposed for synthesis as novel selective MAO-A or –B inhibitors. -
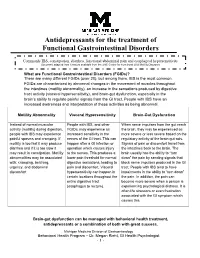
Antidepressants for Functional Gastrointestinal Disorders
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

Nialamide; SOCIETIES and LECTURES CORRECTION
414 BRITISH MEDICAL JOURNAL 15 MAY 1971 care, and administration of health services. A. Clements, P. A. Connell, Patricia A. Crawford, G. A. Cupper, M. R. Dean, L. L. Dom- "It is, in short, medicine applied to a group SOCIETIES AND LECTURES bey, D. P. De Bono, J. P. Delamere, Gil- than to an individual patient." The lean P. Duncan, D. B. Dunger, C. E. G. Farqu- rather Br Med J: first published as 10.1136/bmj.2.5758.414 on 15 May 1971. Downloaded from statement adds that it is hoped that the pro- For attending lectures marked * a fee is charged or harson, Pamela C. Fenney, Daphne C. Fielding, a ticket is required. Applications should be made I. R. Fletcher, M. S. Fletcher, Po-Kai Fok, G. J. visional Faculty will be in a position to re- Frost, R. M. Galbraith, Elizabeth A. S. Galvin, first to the institution concerned. D. J. Giraldi, Jenifer I. Glover, B. A. Greenway, ceive applications from those wishing to be- Mary Griffin, J. F. Hamlyn, M. H. Hampton, come founder members later in the year. Monday, 17 May G. P. Harris, P. B. Harvey, A. C. Hillyard, Gillian M. M. Hodge, N. Holmes, Sheilagh M. Further announcements will be made. ABERDEEN UNIVERSITY.-At Medical Buildings, Hope, C. C. Hugh, Joanna E. Ide, Alison Ironside, Foresterhill, 5.30 p.m., dentj centennial lecture Keatley E. James, W. J. Jarrett, Celia A. Jenkins, by Sir Robert Bradlaw: Pigmentation. J. R. Jenner, P. D. Jones, C. L. Kennedy, N. D. Monoamine-oxidase Inhibitors INSTITUTE OF DERMATOLOGY.-4.30 p.m., Mr. -

Managing Cancer Pain
The British Pain Society's Managing cancer pain - information for patients From the British Pain Society, supported by the Association of Palliative Medicine and the Royal College of General Practitioners January 2010 To be reviewed January 2013 2 Cancer Pain Management Published by: The British Pain Society 3rd floor Churchill House 35 Red Lion Square London WC1R 4SG Website: www.britishpainsociety.org ISBN: 978-0-9551546-8-3 © The British Pain Society 2010 Information for Patients 3 Contents Page What can be done for people with cancer pain 4 Understanding cancer pain 4 Knowing what to expect 6 Options for pain control – most pain can be controlled 6 Coping with cancer pain 8 Describing pain – communicating with your doctors 9 Talking to others with cancer pain 12 Finding help managing cancer pain 12 References 12 Methods 12 Competing Interests 13 Membership of the group and expert contributors 13 4 Cancer Pain Management What can be done for people with cancer pain? There are medicines and expertise available that can help to control cancer pain. However, surveys show that cancer pain is still poorly controlled in many cases. As a result, patients must know what is available, what they have a right to and how to ask for it. Cancer itself and the treatments for cancer, including both medicines and surgery, can cause pain. Treatments can be directed either at the cause of the pain (for example, the tumour itself) or at the pain itself. Understanding cancer pain Cancer pain can be complicated, involving pain arising from inflammation (swelling), nerve damage and tissue damage from many sites around the body. -

Diabetic Neuropathy: a Position Statement by the American
136 Diabetes Care Volume 40, January 2017 Diabetic Neuropathy: A Position Rodica Pop-Busui,1 Andrew J.M. Boulton,2 Eva L. Feldman,3 Vera Bril,4 Roy Freeman,5 Statement by the American Rayaz A. Malik,6 Jay M. Sosenko,7 and Dan Ziegler8 Diabetes Association Diabetes Care 2017;40:136–154 | DOI: 10.2337/dc16-2042 Diabetic neuropathies are the most prevalent chronic complications of diabetes. This heterogeneous group of conditions affects different parts of the nervous system and presents with diverse clinical manifestations. The early recognition and appropriate man- agement of neuropathy in the patient with diabetes is important for a number of reasons: 1. Diabetic neuropathy is a diagnosis of exclusion. Nondiabetic neuropathies may be present in patients with diabetes and may be treatable by specific measures. 2. A number of treatment options exist for symptomatic diabetic neuropathy. 3. Up to 50% of diabetic peripheral neuropathies may be asymptomatic. If not recognized and if preventive foot care is not implemented, patients are at risk for injuries to their insensate feet. 4. Recognition and treatment of autonomic neuropathy may improve symptoms, POSITION STATEMENT reduce sequelae, and improve quality of life. Among the various forms of diabetic neuropathy, distal symmetric polyneurop- athy (DSPN) and diabetic autonomic neuropathies, particularly cardiovascular au- tonomic neuropathy (CAN), are by far the most studied (1–4). There are several 1 atypical forms of diabetic neuropathy as well (1–4). Patients with prediabetes may Division of Metabolism, Endocrinology & Diabe- – tes, Department of Internal Medicine, University also develop neuropathies that are similar to diabetic neuropathies (5 10). -

Ayahuasca Characterization, Metabolism in Humans, And
Louisiana State University LSU Digital Commons LSU Doctoral Dissertations Graduate School 2012 Ayahuasca characterization, metabolism in humans, and relevance to endogenous N,N- dimethyltryptamines Ethan Hamilton McIlhenny Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_dissertations Part of the Medicine and Health Sciences Commons Recommended Citation McIlhenny, Ethan Hamilton, "Ayahuasca characterization, metabolism in humans, and relevance to endogenous N,N- dimethyltryptamines" (2012). LSU Doctoral Dissertations. 2049. https://digitalcommons.lsu.edu/gradschool_dissertations/2049 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Doctoral Dissertations by an authorized graduate school editor of LSU Digital Commons. For more information, please [email protected]. AYAHUASCA CHARACTERIZATION, METABOLISM IN HUMANS, AND RELEVANCE TO ENDOGENOUS N,N-DIMETHYLTRYPTAMINES A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and School of Veterinary Medicine in partial fulfillment of the requirements for the degree of Doctor of Philosophy in The Interdepartmental Program in Veterinary Medical Sciences through the Department of Comparative Biomedical Sciences by Ethan Hamilton McIlhenny B.A., Skidmore College, 2006 M.S., Tulane University, 2008 August 2012 Acknowledgments Infinite thanks, appreciation, and gratitude to my mother Bonnie, father Chaffe, brother Matthew, grandmothers Virginia and Beverly, and to all my extended family, friends, and loved ones. Without your support and the visionary guidance of my friend and advisor Dr. Steven Barker, none of this work would have been possible. Special thanks to Dr. -

Psychotropic Medication Concerns When Treating Individuals with Developmental Disabilities
Tuesday, 2:30 – 4:00, C2 Psychotropic Medication Concerns when Treating Individuals with Developmental Disabilities Richard Berchou 248-613-6716 [email protected] Objective: Identify effective methods for the practical application of concepts related to improving the delivery of services for persons with developmental disabilities Notes: Medication Assistance On-Line Resources OBTAINING MEDICATION: • Needy Meds o Needymeds.com • Partnership for Prescriptions Assistance o Pparx.org • Patient Assistance Program Center o Rxassist.org • Insurance coverage & Prior authorization forms for most drug plans o Covermymeds.com REMINDERS TO TAKE MEDICATION: • Medication reminder by Email, Phone call, or Text message o Sugaredspoon.com ANSWER MOST QUESTIONS ABOUT MEDICATIONS: • Univ. of Michigan/West Virginia Schools of Pharmacy o Justaskblue.com • Interactions between medications, over-the-counter (OTC) products and some foods; also has a pictorial Pill Identifier: May input an entire list of medications o Drugs.com OTHER TRUSTED SITES: • Patient friendly information about disease and diagnoses o Mayoclinic.com, familydoctor.org • Package inserts, boxed warnings, “Dear Doctor” letters (can sign up to receive e- mail alerts) o Dailymed.nlm.nih.gov • Communications about drug safety o www.Fda.gov/cder/drug/drugsafety/drugindex.htm • Purchasing medications on-line o Pharnacychecker.com Updated 2013 Psychotropic Medication for Persons with Developmental Disabilities April 23, 2013 Richard Berchou, Pharm. D. Assoc. Clinical Prof., Dept. Psychiatry & Behavioral