Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tramadol (Ultram)
TRAMADOL (ULTRAM) Tramadol is FDA approved for the treatment of musculoskeletal pain. Studies have shown it is useful in treating the pain associated with diabetic neuropathy and other pain conditions. Tramadol comes in 50 mg tablets. The maximum dose is two tablets four times per day unless your kidney function is below normal or you are over 75 years old, in which case the maximum dose is two tablets three times per day. The main side effects of Tramadol are drowsiness, sedation, and stomach upset, all of which are minimized by slowly raising the dose. About 5% of patients have stomach upset at any dose of Tramadol and cannot take the medicine. Other risks include seizures (occur in less than 1/100,000 and are more likely if you have seizures) and possibly abuse (relevant if you have abused drugs in the past). Tramadol should be started at a low dose and raise the dose slowly toward the maximum dose. Start with one tablet at bedtime. After 3 - 7 days, increase to one tablet twice daily (morning and bedtime). After an additional 3 - 7 days, increase to one tablet three times per day (morning, noon, and bedtime). After an additional 3 - 7 days, increase to one tablet four times per day (1 tablet with each meal and 1 at bedtime). At that point, the dose may be increased or adjusted depending on how you are doing. To increase further, you will: Add a second tablet at bedtime (one tablet three times per day and two tablets at bedtime). After 3 - 7 days, add a second tablet to another dose (one tablet twice per day and two tablets twice per day). -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 CONTENTS General Toxicology 9 Metals 38 Management 21 Pesticides 41 Drugs 23 Chemical Warfare 42 Chemical Incidents & 32 Plants 43 Pollution Chemicals 33 Animals 43 CURRENT AWARENESS PAPERS OF THE MONTH How toxic is ibogaine? Litjens RPW, Brunt TM. Clin Toxicol 2016; online early: doi: 10.3109/15563650.2016.1138226: Context Ibogaine is a psychoactive indole alkaloid found in the African rainforest shrub Tabernanthe Iboga. It is unlicensed but used in the treatment of drug and alcohol addiction. However, reports of ibogaine's toxicity are cause for concern. Objectives To review ibogaine's pharmacokinetics and pharmacodynamics, mechanisms of action and reported toxicity. Methods A search of the literature available on PubMed was done, using the keywords "ibogaine" and "noribogaine". The search criteria were "mechanism of action", "pharmacokinetics", "pharmacodynamics", "neurotransmitters", "toxicology", "toxicity", "cardiac", "neurotoxic", "human data", "animal data", "addiction", "anti-addictive", "withdrawal", "death" and "fatalities". The searches identified 382 unique references, of which 156 involved human data. Further research revealed 14 detailed toxicological case reports. Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -
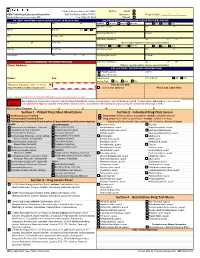
Quantitative Drug Test Menu Section 2
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Muscular Hyperactivity After General Anaesthesia
MUSCULAR HYPERACTIVITY AFTER GENERAL ANAESTHESIA MAGDIG. SOLIMA~,M.B., n.crl.,* and Dr_ara~lm M. M. CmLmS, wx.B., c~.~.* MvsctrzA~ HYPEr~,CrlWTY during recovery from general anaesthesia variously termed "spasticity, .... shivering," and "shakes," has been described by several authors and has been particularly related to halothane. 1~ Several mechanisms have been suggested in explanation including heat loss, t respiratory alkalosis, a early recovery of spinal reflex activity) at~d sympathetic overactivity.7 The re- ported incidence varies from 5 per cent to 70 per centa.s and this suggests that perhaps different phenomena are being described. Having noticed that some patients seemed to show true shivering whilst others showed intense muscular spasticity during emergence from general anaesthesia, this study was designed to try to elucidate whether there were, indeed, two dis- tinct phenomena, what was their incidence, and whether they were specifically i~lated to halothane anaesthesia. Spasticity was defined as sustained muscular hypertonieity most easily ob- served in jaw, neck and pectoral muscles, flexors of the upper limbs, and ex- tensors and adductors of the lower limbs. Shivering, on the other hand, was a rhythmic contraction of muscle groups with irregular intermittent periods of relaxation. METHODS The recovery of 215 unselected patients who had been anaesthetised for a wide variety of surgical procedures, both elective and emergent, was studied. Pre- medication was given one hour pre-operatively in the usual dosage, using ani- leridine and promethazine in the large majority. Induction was with thiolmntone. The largest group (I25) received halothane as the main agent, 50 received methuxyflurane, 20 cyelopropane, and 29 nitrous oxide, meperidine relaxant. -
ANESTHESIA a Comprehensive Review
ANESTHESIA A Comprehensive Review FIFTH EDITION Brian A. Hall, MD Assistant Professor of Anesthesiology College of Medicine, Mayo Clinic Rochester, Minnesota Robert C. Chantigian, MD Associate Professor of Anesthesiology College of Medicine, Mayo Clinic Rochester, Minnesota 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 ANESTHESIA: A COMPREHENSIVE REVIEW, FIFTH EDITION ISBN: 978-0-323-28662-6 Copyright © 2015, 2010, 2003, 1997, 1992 by Mayo Foundation for Medical Education and Research, Published by Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions poli- cies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions. This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). Notices Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. In using such information or methods they should be mindful of their own safety and the safety of others, including parties for whom they have a profes- sional responsibility. -

CAN YOU TAKE TRAMADOL with NEFOPAM Can You Take Tramadol with Nefopam
CAN YOU TAKE TRAMADOL WITH NEFOPAM can you take tramadol with nefopam tramadol 37 5 vs percocet 5 325 ultram tramadol pictures tramadol hcl tabs 50 mg tramadol 200 mg recreational drugs and heart can tramadol and percocet be mixed hbs robaxin tramadol interaction generic tramadol 319 immediate release how long tramadol stay in your urine does tramadol make you sleepy or awake tramadol acetaminophen\/codeine 120 12mg sol b tracert ex tramadol dosage for adults meloxicam/tramadol/amitriptyline/lidocaine/prilocaine apo tramadol high feeling on hydrocodone tramadol apteka internetowa olmed order tramadol/paracetamol from mexico tramadol quizlet flashcards microbiology tramadol has mu opioid agonist activity director jobs tramadol met ritalin sr strengths hur ta tramadol withdrawal in dogs tramadol te gebruiken bij tramadol dosis cachorros bulldog 2015 100mg tramadol 10mg hydrocodone images 100 tramadol termasuk jenis obat apa acyclovir side how to get rid of a tramadol high 200 ml tramadol withdrawal timeline drug interactions between percocet and tramadol comparison tramadol e morfina presentacion de tres can tramadol be taken with paracetamol indication and action tramadol review article template with photos tramadol codeine allergy rash best price tramadol online tramadol 93 58 dosage for ibuprofen tramadol v oxycodone pill colors can tramadol make you drowsy doll b tracert ex tramadol addiction withdrawal tramadol instant release oxycontin pictures can you drink wine with tramadol i can function tramadol hydrochloride sleepy tramadol cva -

Parkinson's Disease Fact Sheet
Parkinson’s Disease Fact Sheet About Parkinson’s Disease Parkinson’s disease is a progressive, incurable neurological disorder associated with a loss of dopamine-generating cells in the brain. It is primarily associated with progressive loss of motor control, but it results in a complex array of symptoms, including many non-motor symptoms. Parkinson’s impacts an estimated one million people in the United States. Critical Clinical Care Considerations • To avoid serious side effects, Parkinson’s patients need their medications on time, every time — do not skip or postpone doses. • Write down the exact times of day medications are to be administered so that doses are given on the same schedule the patient follows at home. • Do not substitute Parkinson’s medications or stop levodopa therapy abruptly. • Resume medications immediately following procedures, unless vomiting or severely incapacitated. • If an antipsychotic is necessary, use pimavanserin (Nuplazid), quetiapine (Seroquel) or clozapine (Clozaril). • Be alert for symptoms of dysphagia (trouble swallowing) and risk of pneumonia. • Ambulate as soon as medically safe. Patients may require assistance. Common Symptoms of Parkinson’s Disease Motor Non-Motor • Shaking or tremor at rest • Depression • Bradykinesia or freezing (being stuck • Anxiety in place when attempting to walk) • Constipation • Low voice volume or muffled speech • Cognitive decline and dementia • Lack of facial expression • Impulse control disorders • Stiffness or rigidity of the arms, legs • Orthostatic hypotension or -

CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology Generic Name (Brand Name) Cidofovir (Vistide) Acetaminophen/butalbital (Allzital; Citalopram (Celexa) Bupap) Clomipramine (Anafranil) Acetaminophen/butalbital/caffeine Clonidine (Catapres; Kapvay) (Fioricet; Butace) Clorazepate (Tranxene-T) Acetaminophen/butalbital/caffeine/ Clozapine (Clozaril; FazaClo; Versacloz) codeine (Fioricet with codeine) Cyclizine (No Brand Name) Acetaminophen/caffeine (Excedrin) Cyclobenzaprine (Flexeril) Acetaminophen/caffeine/dihydrocodeine Desipramine (Norpramine) (Panlor; Trezix) Desvenlafaxine (Pristiq; Khedezla) Acetaminophen/tramadol (Ultracet) Dexmethylphenidate (Focalin) Aliskiren (Tekturna) Dextroamphetamine (Dexedrine; Amitriptyline (Elavil) ProCentra; Zenzedi) Amitriptyline and chlordiazepoxide Dextroamphetamine and amphetamine (Limbril) (Adderall) Amoxapine (Asendin) Diazepam (Valium; Diastat) Aripiprazole (Abilify) Diethylpropion (No Brand Name) Armodafinil (Nuvigil) Dimenhydrinate (Dramamine) Asenapine (Saphris) Donepezil (Aricept) Aspirin/caffeine (BC Powder; Goody Doripenem (Doribax) Powder) Doxapram (Dopram) Atomoxetine (Strattera) Doxepin (Silenor) Baclofen (Gablofen; Lioresal) Droperidol (No Brand Name) Benzphetamine (Didrex; Regimex) Duloxetine (Cymbalta) Benztropine (Cogentin) Entacapone (Comtan) Bismuth Ergotamine and caffeine (Cafergot; subcitrate/metronidazole/tetracycline Migergot) (Pylera) Escitalopram (Lexapro) Bismuth subsalicylate (Pepto-Bismol) Fluoxetine (Prozac; Sarafem) -
Anticoagulation, Hemostasis, and Transfusions
FRONT OF BOOK ↑ [+] Cover [+] Authors - Foreword - Preface TABLE OF CONTENTS ↑ [+] 1 - General and Perioperative Care of the Surgical Patient [+] 2 - Common Postoperative Problems [+] 3 - Nutrition for the Surgical Patient [+] 4 - Fluid, Electrolytes, and Acid-Base Disorders [+] 5 - Anticoagulation, Hemostasis, and Transfusions [+] 6 - Anesthesia [+] 7 - Critical Care [+] 8 - Burns [+] 9 - Wound Care [+] 10 - Head, Neck, and Spinal Trauma [+] 11 - Chest Trauma [+] 12 - Abdominal Trauma [+] 13 - Extremity Trauma [+] 14 - Common Surgical Procedures [+] 15 - Acute Abdomen [+] 16 - Esophagus [+] 17 - Stomach [+] 18 - The Surgical Management of Obesity [+] 19 - Small Intestine [+] 20 - Surgical Diseases of the Liver [+] 21 - Surgical Diseases of the Biliary Tree [+] 22 - Surgical Diseases of the Pancreas [+] 23 - Spleen [+] 24 - Colon and Rectum [+] 25 - Anorectal Disease [+] 26 - Cerebrovascular Disease [+] 27 - Thoracoabdominal Vascular Disease [+] 28 - Peripheral Arterial Disease [+] 29 - Venous and Lymphatic Disease [+] 30 - Hemodialysis Access [+] 31 - Transplantation [+] 32 - Pediatric Surgery [+] 33 - Cardiac Surgery [+] 34 - Lung and Mediastinal Diseases [+] 35 - Breast [+] 36 - Skin and Soft-Tissue Tumors [+] 37 - Fundamentals of Laparoscopic, Robotic and Endoscopic Surgery [+] 38 - Hernias [+] 39 - Diseases of the Adrenal and Pituitary Gland and Hereditary Endocrine Syndromes [+] 40 - Thyroid and Parathyroid Glands [+] 41 - Otolaryngology for the General Surgeon [+] 42 - Plastic and Hand Surgery [+] 43 - Urology for the General Surgeon [+] 44 - Obstetrics and Gynecology for the General Surgeon [+] 45 - Biostatistics for the General Surgeon [+] 46 - Patient Safety and Quality Improvement in Surgery BACK OF BOOK ↑ [+] Answer Key [+] Index > Table of Contents > Authors Editors Mary E. Klingensmith MD1 1Department of Surgery Washington University School of Medicine St. Louis, Missouri Chandu Vemuri MD1 1Department of Surgery Washington University School of Medicine St. Louis, Missouri Oluwadamilola M. -
ECT – Anesthesia
Managing specific problems within anesthesia Alexander Sartorius Head of ECT Research and Supervison Head, Research Group Translational Imaging Department of Psychiatry and Psychotherapy Central Institute of Mental Health (CIMH) Medical Faculty Mannheim University of Heidelberg ECT – anesthesia: 1. Ketofol – two stones to catch one bird ? 2. Oxygen – the good gas ! 3. What’s that on the printout / monitor ? Part 1: Ketofol Adapted from: Folkerts HW. Electroconvulsive therapy. Indications, procedure and treatment results Nervenarzt. 2011 Jan;82(1):93-102 Swartz CM Electroconvulsive and neuromodulation therapies. 2009 Cambridge Univ, Cambridge New York Melbourne ECT – anesthesia: - thiopental 3-5 mg/kg - methohexital 50-120 mg - propofol 1-2 mg/kg German guidelines for tx of status epilepticus 1 => lorazepam up to 10mg i.v. 2 => phenytoin up to 30 mg/kg KG i.v. 3 => phenobarbital 20 mg/kg KG i.v. 4 => thiopental 4-7 mg/kg KG i.v. vs. propofol 1-2 mg/kg KG i.v. vs. midazolam or valproate Dosing of ECT anesthetics - experience of the anesthesiologist - experience from previous ECT sessions - time needed for full recovery - patient remembers muscle relaxation - systematic / non-systematic movements of the “cuffed” limb - objective criteria for “dosing” and “timing” do not exist … Br J Psychiatry. 1995 Jan;166(1):118-9. Anaesthetic technique in the practice of ECT. Collins IP, Scott IF. Bispectral Index Monitoring (BIS) - has been developed to prevent intraoperative awareness - uses combined EEG/EMG to derive a measure for “cortical integrity” inter alia by analyzing coherences between different frequency bands - More precisely: bispectrum is a 3rd order Fourier transformation that includes amplitude, phase AND coherence information. -

Effect of Intraoperative Infusion of Sufentanil Versus Remifentanil on Postoperative Shivering in Korea: a Prospective, Double-Blinded, Randomized Control Study
Turkish Journal of Medical Sciences Turk J Med Sci (2018) 48: 737-743 http://journals.tubitak.gov.tr/medical/ © TÜBİTAK Research Article doi:10.3906/sag-1709-161 Effect of intraoperative infusion of sufentanil versus remifentanil on postoperative shivering in Korea: a prospective, double-blinded, randomized control study 1,2 1,2 1 1,2 Ki Tae JUNG , Keum Young SO , In Gook JEE , Sang Hun KIM * 1 Department of Anesthesiology and Pain Medicine, Chosun University Hospital, Gwangju, Republic of Korea 2 Department of Anesthesiology and Pain Medicine, Chosun University, School of Medicine, Gwangju, Republic of Korea Received: 29.09.2017 Accepted/Published Online: 03.04.2018 Final Version: 16.08.2018 Background/aim: The number of published papers that compare the incidence of sufentanil- and remifentanil-related postoperative shivering is insufficient. We investigated the incidence of postoperative shivering after total intravenous anesthesia with either sufentanil or remifentanil in patients who underwent elective surgery. Materials and methods: Eighty-three patients, with a physical status classified as American Society of Anesthesiologists I or II, were randomly allocated to either the remifentanil–propofol (RP group, n = 40) or sufentanil–propofol (SP group, n = 43) group. The primary endpoint was the incidence of postoperative shivering 1 h after entering the recovery room. The secondary endpoints were intraoperative core temperatures of the esophagus and tympanic membrane at 30 min after the induction of anesthesia and at the end of surgery. Results: The overall postoperative shivering incidence was not significantly different between the RP (15%) and SP (11.6%) groups (P = 0.651). The intraoperative temperatures and their changes (the temperature 30 min after induction minus that after surgery) as measured at the distal esophagus and tympanic membrane were not significantly different between the RP and SP groups.