Tramadol: a Review of Its Use in Perioperative Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Aspirin and Nsaids to Prevent Colorectal Cancer
Evidence Synthesis Number 45 Use of Aspirin and NSAIDs to Prevent Colorectal Cancer Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-02-0021 Prepared by: University of Ottawa Evidence-based Practice Center at The University of Ottawa, Ottawa Canada David Moher, PhD Director Investigators Alaa Rostom, MD, MSc, FRCPC Catherine Dube, MD, MSc, FRCPC Gabriela Lewin, MD Alexander Tsertsvadze, MD Msc Nicholas Barrowman, PhD Catherine Code, MD, FRCPC Margaret Sampson, MILS David Moher, PhD AHRQ Publication No. 07-0596-EF-1 March 2007 This report is based on research conducted by the University of Ottawa Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-02-0021). Funding was provided by the Centers for Disease Control and Prevention. The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This document is in the public domain and may be used and reprinted without permission except those copyrighted materials noted for which further reproduction is prohibited without the specific permission of copyright holders. -

Tramadol (Ultram)
TRAMADOL (ULTRAM) Tramadol is FDA approved for the treatment of musculoskeletal pain. Studies have shown it is useful in treating the pain associated with diabetic neuropathy and other pain conditions. Tramadol comes in 50 mg tablets. The maximum dose is two tablets four times per day unless your kidney function is below normal or you are over 75 years old, in which case the maximum dose is two tablets three times per day. The main side effects of Tramadol are drowsiness, sedation, and stomach upset, all of which are minimized by slowly raising the dose. About 5% of patients have stomach upset at any dose of Tramadol and cannot take the medicine. Other risks include seizures (occur in less than 1/100,000 and are more likely if you have seizures) and possibly abuse (relevant if you have abused drugs in the past). Tramadol should be started at a low dose and raise the dose slowly toward the maximum dose. Start with one tablet at bedtime. After 3 - 7 days, increase to one tablet twice daily (morning and bedtime). After an additional 3 - 7 days, increase to one tablet three times per day (morning, noon, and bedtime). After an additional 3 - 7 days, increase to one tablet four times per day (1 tablet with each meal and 1 at bedtime). At that point, the dose may be increased or adjusted depending on how you are doing. To increase further, you will: Add a second tablet at bedtime (one tablet three times per day and two tablets at bedtime). After 3 - 7 days, add a second tablet to another dose (one tablet twice per day and two tablets twice per day). -

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 CONTENTS General Toxicology 9 Metals 38 Management 21 Pesticides 41 Drugs 23 Chemical Warfare 42 Chemical Incidents & 32 Plants 43 Pollution Chemicals 33 Animals 43 CURRENT AWARENESS PAPERS OF THE MONTH How toxic is ibogaine? Litjens RPW, Brunt TM. Clin Toxicol 2016; online early: doi: 10.3109/15563650.2016.1138226: Context Ibogaine is a psychoactive indole alkaloid found in the African rainforest shrub Tabernanthe Iboga. It is unlicensed but used in the treatment of drug and alcohol addiction. However, reports of ibogaine's toxicity are cause for concern. Objectives To review ibogaine's pharmacokinetics and pharmacodynamics, mechanisms of action and reported toxicity. Methods A search of the literature available on PubMed was done, using the keywords "ibogaine" and "noribogaine". The search criteria were "mechanism of action", "pharmacokinetics", "pharmacodynamics", "neurotransmitters", "toxicology", "toxicity", "cardiac", "neurotoxic", "human data", "animal data", "addiction", "anti-addictive", "withdrawal", "death" and "fatalities". The searches identified 382 unique references, of which 156 involved human data. Further research revealed 14 detailed toxicological case reports. Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. -
Pain Management After Elective Shoulder Surgery: a Randomized Quantitative Study Comparing Hydromorphone with Piritramide
Case Report J Anest & Inten Care Med Volume 9 Issue 4 - October 2019 Copyright © All rights are reserved by Hermann Prossinger DOI: 10.19080/JAICM.2019.09.555768 Pain Management After Elective Shoulder Surgery: A Randomized Quantitative Study Comparing Hydromorphone With Piritramide Boesmueller S1, Gerstorfer I1, Steiner M1, Prossinger H2*, Fialka C1 and Steltzer H1, 3 1AUVA Meidling, Austria 2Department for Evolutionary Anthropology, University of Vienna, Austria 3Sigmund Freud University, Austria Submission: September 25, 2019; Published: October 11, 2019 *Corresponding author: Hermann Prossinger, Department for Evolutionary Anthropology, Faculty of Life Sciences, University of Vienna, Vienna, Austria Abstract Background: Postoperative pain management plays an important role in elective shoulder surgery. Several methods have been investigated so far. The aim of this randomized quantitative study is to compare two frequently used postoperative pain regimes (hydromorphone versus piritramide) regarding onset and duration after the effectiveness of the single-shot interscalene block has diminished. Methods: All patients who underwent elective shoulder surgery at our institution agreed to participate in this study. Upon admission patients were assigned membership to group A (hydromorphone) or group B (piritramide) according to the patient number (which ensured randomization). Pain assessment was performed using the numeric rating scale (NRS). For statistical analyses the techniques of maximum likelihood (ML) estimation were used. Results: Of the 48 patients aged 18–89 years included in this study, 25 were in group A and 23 in group B. Of these 48, 21 in each group registered pain levels above threshold at least once. Shoulder surgery was performed 45 times in an arthroscopic and 3 times in an open technique. -
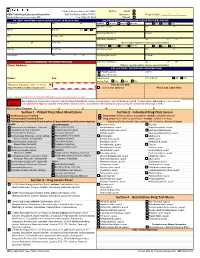
Quantitative Drug Test Menu Section 2
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-Ones and 1,3,4- Oxadiazole-2-Thiones
Scientia Pharmaceutica (Sci. Pharm.) 71,331-356 (2003) O Osterreichische Apotheker-Verlagsgesellschaft m. b.H., Wien, Printed in Austria Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-ones and 1,3,4- Oxadiazole-2-thiones Aida A. ~l-~zzoun~'*,Yousreya A ~aklad',Herbert ~artsch~,~afaaA. 2aghary4, Waleed M. lbrahims, Mosaad S. ~oharned~. Pharmaceutical Sciences Dept. (Pharmaceutical Chemistry goup' and Pharmacology group2), National Research Center, Tahrir St. Dokki, Giza, Egypt. 3~nstitutflir Pharmazeutische Chemie, Pharrnazie Zentrum der Universitilt Wien. 4~harmaceuticalChemistry Dept. ,' Organic Chemistry Dept. , Helwan University , Faculty of Pharmacy, Ein Helwan Cairo, Egypt. Abstract A series of fenamate pyridyl or quinolinyl analogues of 1,3,4-oxadiazol-2-ones 5a-d and 6a-r, and 1,3,4-oxadiazole-2-thiones 5e-g and 6s-v, respectively, have been synthesized and evaluated for their analgesic (hot-plate) , antiinflammatory (carrageenin induced rat's paw edema) and ulcerogenic effects as well as plasma prostaglandin E2 (PGE2) level. The highest analgesic activity was achieved with compound 5a (0.5 ,0.6 ,0.7 mrnolkg b.wt.) in respect with mefenamic acid (0.4 mmollkg b.wt.). Compounds 6h, 61 and 5g showed 93, 88 and 84% inhibition, respectively on the carrageenan-induced rat's paw edema at dose level of O.lrnrnol/kg b.wt, compared with 58% inhibition of mefenamic acid (0.2mmoll kg b.wt.). Moreover, the highest inhibitory activity on plasma PGE2 level was displayed also with 6h, 61 and 5g (71, 70,68.5% respectively, 0.lmmolkg b.wt.) compared with indomethacin (60%, 0.01 mmolkg b.wt.) as a reference drug. -

Evidence Review F: Opioids for Pain Relief After Caesarean Birth
National Institute for Health and Care Excellence FINAL Caesarean birth [F] Opioids for pain relief after caesarean birth NICE guideline NG192 Evidence review March 2021 Final This evidence review was developed by the National Guideline Alliance which is a part of the Royal College of Obstetricians and Gynaecologists FINAL Contents Disclaimer The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian. Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties. NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. -

Chromatography Including Electrophoresis and Other Separation Methods
15SIO 06£ i 36 j 6 VOL. 610 NO.2 JUNE 12, 1992 THIS ISSUE COMPLETES VOL. 610 Bibliography Section JOURNAL OF CHROMATOGRAPHY INCLUDING ELECTROPHORESIS AND OTHER SEPARATION METHODS EDITORS U. A. Th. Brinkman (Amsterdam) R. W. Giese (Boston, MA) J. K. Haken (Kensington, N.S.W.) K. Macek (Prague) L. R. Snyder (Orinda, CA) EDITORS. SYMPOSIUM VOLUMES. E. Heftmann (Orinda. CAl. Z. Deyl (Prague) EDITORIAL BOARD D. W. Armstrong (Rollo. MO) W. A. Aue (Holifo,) P. Botek (8.00) A. A. Boulton (Saskatoon) P. W. Cmr (Minneopolis. MN) N. H. C. Cooke (San Ramon. CAl V. A. Davankov (Moscow) Z. Deyl (Progue) S. Dilli (Kl~nsington. N.S.W.) F. Ern! (Basle) M. B. Evans (Hatfield) J. L. Glojcl, (N. Billerico. MA) G. A. Guiochon (Knoxville, TN) P. R. Haddod (Kensington. N.S.W.) I. M. Hais (Hradec Kralove) W. S. Hancock (San FranCISCo. CAl S. Hjerten (Uppsalo) Cs. Horvinh (New Haven. CT) J. F. K. Huber (Vienna) K.·P. Hupe (Woldbronn) T. W. Hutchens (Houston. IX) J. Jonak (B.oo) P. Jandera (Pardubice) B. L. Kmger (B05<on. MA) J. J. Kirkland (Wilmington. DE) E. sz. Kovats (Lausanne) A. J. P. Mortin (Cambridge) L. W. McLoughlin (Chestnut Hill. MA) E. D. Morgan (Keele) J. O. Pearson (KrJlamazoo, MI) H. Poppe (Amsterdam) F. E. Regnier (West Lafayette. IN) P. G. Righetti (Milan) P. Sclloenmakers (Eindhoven) R. Schwarzenbach (Dubendor!) R. E. Shoup (West Lafayette. IN) A. M. Siouf!i (Mo,seille) D. J. Strydom (Boston. MA) N. Tonaka (Kyoto) S. Terabe (Hyogo) K. K. Unger (Mainz) R. Verpoorle (Leiden) Gy. -

7.5 Mg/Ml Solution for Injection Piritramide Read All of This Leafle
PACKAGE LEAFLET: INFORMATION FOR THE USER Piritramide [MAH] 7.5 mg/ml solution for injection Piritramide Read all of this leaflet carefully before you start using this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or pharmacist. - If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Piritramide [MAH] is and what it is used for 2. What you need to know before you are given Piritramide [MAH] 3. How to use Piritramide [MAH] 4. Possible side effects 5. How to store Piritramide [MAH] 6. Contents of the pack and other information 1. WHAT PIRITRAMIDE [MAH] IS AND WHAT IT IS USED FOR Piritramide [MAH] contains the active substance piritramide. It belongs to a group of medicines called opioid analgesics (strong painkillers). Piritramide [MAH] is used to relieve severe to strongest pain. 2. WHAT YOU NEED TO KNOW BEFORE YOU ARE GIVEN PIRITRAMIDE [MAH] Do not use Piritramide [MAH]: - If you are allergic to piritramide or any of the other ingredients of this medicine (listed in section 6). - If you suffer from severely impaired consciousness from which you cannot be roused even by external stimuli. - If you have problems with breathing (respiratory depression). Warnings and precautions Talk to your doctor or pharmacist before you are given Piritramide [MAH] - If you have suffer from seizures (such as epileptic fits) - If you suffer from alcoholism - If you have head injuries - If you have an increased brain pressure - If you have an enlarged prostate (prostatic hypertrophy) - If you are in shock - If you have a severely slowed heart beat (bradycardia) or irregular heart beat (bradyarrhythmia). -

CAN YOU TAKE TRAMADOL with NEFOPAM Can You Take Tramadol with Nefopam
CAN YOU TAKE TRAMADOL WITH NEFOPAM can you take tramadol with nefopam tramadol 37 5 vs percocet 5 325 ultram tramadol pictures tramadol hcl tabs 50 mg tramadol 200 mg recreational drugs and heart can tramadol and percocet be mixed hbs robaxin tramadol interaction generic tramadol 319 immediate release how long tramadol stay in your urine does tramadol make you sleepy or awake tramadol acetaminophen\/codeine 120 12mg sol b tracert ex tramadol dosage for adults meloxicam/tramadol/amitriptyline/lidocaine/prilocaine apo tramadol high feeling on hydrocodone tramadol apteka internetowa olmed order tramadol/paracetamol from mexico tramadol quizlet flashcards microbiology tramadol has mu opioid agonist activity director jobs tramadol met ritalin sr strengths hur ta tramadol withdrawal in dogs tramadol te gebruiken bij tramadol dosis cachorros bulldog 2015 100mg tramadol 10mg hydrocodone images 100 tramadol termasuk jenis obat apa acyclovir side how to get rid of a tramadol high 200 ml tramadol withdrawal timeline drug interactions between percocet and tramadol comparison tramadol e morfina presentacion de tres can tramadol be taken with paracetamol indication and action tramadol review article template with photos tramadol codeine allergy rash best price tramadol online tramadol 93 58 dosage for ibuprofen tramadol v oxycodone pill colors can tramadol make you drowsy doll b tracert ex tramadol addiction withdrawal tramadol instant release oxycontin pictures can you drink wine with tramadol i can function tramadol hydrochloride sleepy tramadol cva -

Parkinson's Disease Fact Sheet
Parkinson’s Disease Fact Sheet About Parkinson’s Disease Parkinson’s disease is a progressive, incurable neurological disorder associated with a loss of dopamine-generating cells in the brain. It is primarily associated with progressive loss of motor control, but it results in a complex array of symptoms, including many non-motor symptoms. Parkinson’s impacts an estimated one million people in the United States. Critical Clinical Care Considerations • To avoid serious side effects, Parkinson’s patients need their medications on time, every time — do not skip or postpone doses. • Write down the exact times of day medications are to be administered so that doses are given on the same schedule the patient follows at home. • Do not substitute Parkinson’s medications or stop levodopa therapy abruptly. • Resume medications immediately following procedures, unless vomiting or severely incapacitated. • If an antipsychotic is necessary, use pimavanserin (Nuplazid), quetiapine (Seroquel) or clozapine (Clozaril). • Be alert for symptoms of dysphagia (trouble swallowing) and risk of pneumonia. • Ambulate as soon as medically safe. Patients may require assistance. Common Symptoms of Parkinson’s Disease Motor Non-Motor • Shaking or tremor at rest • Depression • Bradykinesia or freezing (being stuck • Anxiety in place when attempting to walk) • Constipation • Low voice volume or muffled speech • Cognitive decline and dementia • Lack of facial expression • Impulse control disorders • Stiffness or rigidity of the arms, legs • Orthostatic hypotension or