Diabetic Neuropathy: a Position Statement by the American
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Footprints an Informational Newsletter for Patients of APMA Member Podiatrists October 2017
footprints an informational newsletter for patients of APMA member podiatrists october 2017 special EDITION include a DPM for diabetes prevention & Manage Ment According to the CDC, more than 100 million US adults are living with either diabetes or prediabetes. If you have diabetes or prediabetes, it is essential to include a podiatrist for proper diabetes prevention and management. In fact, podiatrists can reduce amputation rates up to 80 percent. In order for you not to become a part of that statistic, here are a few simple things you can do to keep your risk for diabetic ulcers and amputation low: Inspect feet daily. Check your Don’t go barefoot. Don’t go 1 feet and toes every day for 5 without shoes, even in your cuts, bruises, sores, or changes to own home. The risk of cuts and the toenails, such as thickening or infection is too great for those discoloration. with diabetes. Wear thick, soft socks. Avoid Never try to remove calluses, 2 socks with seams, which could 6 corns, or warts by yourself. rub and cause blisters or other Over-the-counter products can burn skin injuries. the skin and cause irreparable damage to the foot for people Exercise. Walking can keep with diabetes. 3 weight down and improve circulation. Be sure to wear See a podiatrist. Regular appropriate athletic shoes when 7 checkups by a podiatrist— exercising. at least annually—are the best WALKING CAN KEEP way to ensure that your feet WEIGHT DOWN AND Have new shoes properly remain healthy. 4 measured and fitted. Foot size IMPROVE CIRCULATION. -

Diabetic Foot Ulcers
REVIEW Review Diabetic foot ulcers William J Jeffcoate, Keith G Harding Ulceration of the foot in diabetes is common and disabling and frequently leads to amputation of the leg. Mortality is high and healed ulcers often recur. The pathogenesis of foot ulceration is complex, clinical presentation variable, and management requires early expert assessment. Interventions should be directed at infection, peripheral ischaemia, and abnormal pressure loading caused by peripheral neuropathy and limited joint mobility. Despite treatment, ulcers readily become chronic wounds. Diabetic foot ulcers have been neglected in health-care research and planning, and clinical practice is based more on opinion than scientific fact. Furthermore, the pathological processes are poorly understood and poorly taught and communication between the many specialties involved is disjointed and insensitive to the needs of patients. In this review, we describe the epidemiology, pathogenesis, operations above the ankle or those proximal to the and management of diabetic foot ulceration, and its effect tarsometatarsal joint, and a multinational WHO survey on on patients and society. The condition deserves more lower extremity amputation also included cases of attention, both from those who provide care and those who unoperated gangrene.13 fund research. Moreover, amputation is a marker not just of disease but also of disease management. The decision to operate Epidemiology is determined by many factors, which vary between Incidence and prevalence centres and patients. A high amputation rate might result Although accurate figures are difficult to obtain for the from high disease prevalence, late presentation, and prevalence or incidence of foot ulcers, the results of cross- inadequate resources, but could also reflect a particular sectional community surveys in the UK showed that 5·3% approach by local surgeons. -

Diabetic Neuropathy
6 Diabetic Neuropathy Solomon Tesfaye, MD, FRCP INTRODUCTION Polyneuropathy is one of the commonest complications of the diabetes and the com- monest form of neuropathy in the developed world. Diabetic polyneuropathy encompasses several neuropathic syndromes, the most common of which is distal symmetrical neuropa- thy, the main initiating factor for foot ulceration. The epidemiology of diabetic neuropathy has recently been reviewed in reasonable detail (1). Several clinic- (2,3) and population- based studies (4,5) show surprisingly similar prevalence rates for distal symmetrical neu- ropathy, affecting about 30% of all people with diabetes. The EURODIAB prospective complications study, which involved the examination of 3250 patient with type 1 from 16 European countries, found a prevalence rate of 28% for distal symmetrical neuropathy (2). After excluding those with neuropathy at baseline, the study showed that over a 7-year period, about one-quarter of patients with type 1 diabetes developed distal symmetrical neuropathy; age, duration of diabetes, and poor glycemic control being major determinants (6). The development of neuropathy was also associated with potentially modifiable car- diovascular risk factors such as serum lipids, hypertension, body mass index, and cigaret smoking (6). Furthermore, cardiovascular disease at baseline carried a twofold risk of neu- ropathy, independent of cardiovascular risk factors (6). Based on recent epidemiological studies, correlates of diabetic neuropathy include increasing age, increasing duration of dia- betes, poor glycemic control, retinopathy, albuminuria, and vascular risk factors (1,2,4,6). The differing clinical presentation of the several neuropathic syndromes in diabetes sug- gests varied etiological factors. CLASSIFICATION Clinical classification of the various syndromes of diabetic peripheral neuropathy has proved difficult. -

Data Entry II Training Course: Supervisor
Training Data Entry II Training Course: Supervisor PCC Supervisor/Manager PCC Operation Guidelines Rating for one Operator Annual Production Rating Formula Fair 20,000 visits 85 forms per day x 230 days per year Good 40,000 visits 170 forms per day x 230 days per year Outstanding 60,000 visits 260 forms per day x 230 days per year 2 PCC Data Entry Needs and Qualifications • On-Reference Material including: • English & Medical Dictionaries • Medical Abbreviations Book • Up-to-date ICD Coding Books • Drug Handbook-Nursing • Data Entry of 20,000 Forms per year by Trained Individual (about 80 forms per day using six to eight mnemonics). • Number of forms processed or data items entered dependent upon each Area or Site. 3 PCC Data Entry Needs and Qualifications (cont.) • Data Entry Staff with the following skills: • Computer keyboard skills • Ability to read provider’s handwriting • Knowledge and understanding of Medical Terminology • Knowledge and understanding of ICD Coding • Knowledge and understanding of Anatomy and Physiology 4 The International Classification of Diseases • ICD-9-CM: 9th Revision, Clinical Modification • The RPMS Coding System for Diagnoses and Procedures 5 ICD Lookup Process • Enter Provider Narrative • FQ Used File • Synonym File • Key Word File • Possible Code(s) 6 Diabetes Diagnosis Codes 250.00 - 250.93 • Type 1 Diabetes - Insulin Dependent Diabetes (Fairly Rare) • Use the Following fifth digit: • 1 - Indicates controlled • 3 - Indicates uncontrolled Note: Requires insulin to survive 7 Diabetes Diagnosis Codes 250.00 - 250.93 (cont.) • Type 2 Diabetes - Non-Insulin Dependent Diabetes (Most frequent Type) • Use the Following fifth-digit: • 0 - Indicates controlled • 2- Indicates uncontrolled Note: Not dependent on insulin to survive; can produce sufficient amounts but may receive insulin to assist the body in using the insulin present in the body. -

Acute Renal Failure in Patients with Type 1 Diabetes Mellitus G
Postgrad Med J: first published as 10.1136/pgmj.70.821.192 on 1 March 1994. Downloaded from Postgrad Med J (1994) 70, 192- 194 C) The Fellowship of Postgraduate Medicine, 1994 Acute renal failure in patients with type 1 diabetes mellitus G. Woodrow, A.M. Brownjohn and J.H. Turney Renal Unit, Leeds General Infirmary, Great George Street, Leeds LSJ 3EX, UK Summary: Acute renal failure (ARF) is a serious condition which still carries a mortality of around 50%. People with diabetes may be at increased risk of developing ARF, either as a complication of diabetic ketoacidosis or hyperosmolar coma, increased incidence of cardiovascular disease, or due to increased susceptibility ofthe kidney to adverse effects in the presence ofunderlying diabetic renal disease. During the period 1956-1992, 1,661 cases of ARF have been treated at Leeds General Infirmary. Of these, we have identified 26 patients also having type 1 diabetes. ARF due to diabetic ketoacidosis is surprisingly uncommon (14 cases out of 23 patients whose notes were reviewed). All cases of ARF complicating ketoacidosis in the last decade have been associated with particularly severe illness requiring intensive care unit support, rather than otherwise 'uncomplicated' ketoacidosis. We discuss the conditions that may result in ARF in patients with diabetes and the particular difficulties that may be encountered in management. Introduction People with diabetes may be at increased risk of Results developing acute renal failure (ARF). Acute pre- copyright. renal failure may occur as a result ofthe severe fluid Of 23 patients with type 1 diabetes complicated by depletion associated with diabetic ketoacidosis and ARF, diabetic ketoacidosis was the main underly- non-ketotic hyperosmolar coma. -

Effect of Biochemical Parameters Showing Atherogenicity in Type 2 Diabetic Nephropathy
International Journal of Basic and Applied Chemical Sciences ISSN: 2277-2073 (Online) An Online International Journal Available at http://www.cibtech.org/jcs.htm 2012 Vol. 2 (4) October-December pp.26-30/Raja and Shaker Research Article EFFECT OF BIOCHEMICAL PARAMETERS SHOWING ATHEROGENICITY IN TYPE 2 DIABETIC NEPHROPATHY *G. Raja and Ivvala Anand Shaker *Department of Biochemistry, Melmaruvathur Adhiparasakthi Institute of Medical Sciences and Research, Melmaruvathur-603319, Tamil Nadu, India *Author for Correspondence ABSTRACT Diabetic nephropathy is one of the major complications of diabetes mellitus characterized by frequent microalbuminuria, elevated arterial blood pressure, a persistent decline in glomerular filtration rate and a high risk of cardiovascular morbidity and mortality. The study comprised of 30 Diabetic mellitus (DM) with microalbuminuria patients (Group 3), 30 DM without microalbuminuria patients (group 2) compared with 30 healthy controls (Group 1). Fasting glucose, post prandial glucose, lipid profile, fructosamine and microalbuminuria were investigated in all the groups. The significant increase in serum fructosamine, fasting and post prandial glucose levels along with increased microalbuminuria observed in group 3 patients compared to group 2 and group 1 patients. Hyperglycemia, increased fructosamine and increased Cholesterol, triglycerides with decreased HDL-cholesterol levels indicates the major risk of atherogenicity. Key Words: Diabetic nephropathy, Microalbuminuria, Fructosamine and Atherogenicity INTRODUCTION Diabetes mellitus (DM) is a disease in which the hallmark feature is elevated blood glucose concentrations due to loss of insulin-producing pancreatic β-cells (type 1 diabetes) or through loss of insulin responsiveness in its target tissues (type 2 diabetes). Type 1 diabetes usually begins to manifest in childhood and early adulthood, but type 2 diabetes is typically a disease for which increased age is a risk factor (Schwarz, 2009). -

Dosing Pattern of Insulin in Diabetic Foot Ulcer Patients TPI 2019; 8(6): 1196-1199 © 2019 TPI B Sarah Fazeeha, P Nivetha, Albin Eldhose, Dr
The Pharma Innovation Journal 2019; 8(6): 1196-1199 ISSN (E): 2277- 7695 ISSN (P): 2349-8242 NAAS Rating: 5.03 Dosing pattern of insulin in diabetic foot ulcer patients TPI 2019; 8(6): 1196-1199 © 2019 TPI www.thepharmajournal.com B Sarah Fazeeha, P Nivetha, Albin Eldhose, Dr. G Veeramani and Dr. J Received: 04-04-2019 Accepted: 06-05-2019 Kabalimurthy B Sarah Fazeeha Abstract Department of Pharmacy, Background: Among the Diabetic patients, 15% develop a foot ulcer and 12-24% of patients with Annamalai University, Chidambaram, Tamil Nadu, diabetic foot ulcer require amputation. We compared the effectiveness of various dosing pattern of India insulin statistically and planned to observe wound healing by proper glycemic control. Methods: We compared the effectiveness of sliding and fixed scale dosing pattern of insulin and P Nivetha observed the wound healing by proper glycemic control. Total 50 subjects were recruited with Grade 3, 4 Department of Pharmacy, and 5 Diabetic foot ulcer (Wagner’s classification) between 40 and 70 years of age who underwent Annamalai University, surgery for management of Foot ulcer. The study was conducted in Tertiary care teaching hospital in Chidambaram, Tamil Nadu, Chidambaram. The study period was 6 month and it was a prospective observational study. The blood India glucose level (Fasting, Random and Post prandial) of subjects were monitored on daily basis and observed. Albin Eldhose Results: The study reports suggested that the major risk factors for Diabetic Foot Ulcer were Poor Department of Pharmacy, glycemic control, Male gender, left foot, Ulcer of size more than 2cm, Infection. -
Diabetic Peripheral Neuropathy
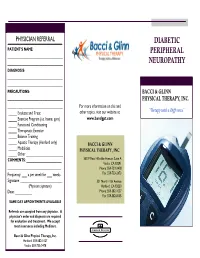
PHYSICIAN REFERRAL DIABETIC PATIENT’S NAME: PERIPHERAL _________________________________ _________________________________ NEUROPATHY DIAGNOSIS: _________________________________ _________________________________ PRECAUTIONS: BACCI & GLINN _________________________________ PHYSICAL THERAPY, INC. _________________________________ For more information on this and _____ Evaluate and Treat other topics, visit our website at: “Therapy with a Difference” _____ Exercise Program (i.e. home, gym) www.bandgpt.com _____ Functional Conditioning _____ Therapeutic Exercise _____ Balance Training _____ Aquatic Therapy (Hanford only) BACCI & GLINN _____ Modalities PHYSICAL THERAPY, INC. _____ Other ______________________ COMMENTS: _____________________ 5533 West Hillsdale Avenue, Suite A Visalia, CA 93291 ________________________________ Phone: 559-733-2478 Frequency: ___ x per week for ___ weeks Fax: 559-733-2470 Signature: _________________________ 331 North 11th Avenue (Physician signature) Hanford, CA 93230 Date: __________ Phone: 559-582-1027 Fax: 559-582-8105 SAME DAY APPOINTMENTS AVAILABLE Referrals are accepted from any physician. A physician’s order and diagnosis are required for evaluation and treatment. We accept most insurances including Medicare. Johnson Designs Bacci & Glinn Physical Therapy, Inc. Hanford: 559-582-1027 Visalia: 559-733-2478 Diabetic Peripheral Neuropathy What is Diabetic Signs and Symptoms of Treatment Options Peripheral Neuropathy? Diabetic Peripheral Neuropathy There is no cure for diabetic neuropa- Diabetic neuropathy is a nerve ♦ Tingling, tightness, or burning, shooting thy. Treatment focuses on slowing the disorder commonly caused by or stabbing pain in feet, hands, or other progression of the disease. Your diabetes. High blood sugar levels parts of the body. physician will determine the best from diabetes can damage nerves ♦ Reduced feeling or numbness, most treatment for your peripheral neuropa- throughout the body. About 50% of often in the feet. -

Diabetic Neuropathy
PRIMER Diabetic neuropathy Eva L. Feldman1*, Brian C. Callaghan1, Rodica Pop-Busui2, Douglas W. Zochodne3, Douglas E. Wright4, David L. Bennett5, Vera Bril6,7, James W. Russell8 and Vijay Viswanathan9 Abstract | The global epidemic of prediabetes and diabetes has led to a corresponding epidemic of complications of these disorders. The most prevalent complication is neuropathy , of which distal symmetric polyneuropathy (for the purpose of this Primer, referred to as diabetic neuropathy) is very common. Diabetic neuropathy is a loss of sensory function beginning distally in the lower extremities that is also characterized by pain and substantial morbidity. Over time, at least 50% of individuals with diabetes develop diabetic neuropathy. Glucose control effectively halts the progression of diabetic neuropathy in patients with type 1 diabetes mellitus, but the effects are more modest in those with type 2 diabetes mellitus. These findings have led to new efforts to understand the aetiology of diabetic neuropathy , along with new 2017 recommendations on approaches to prevent and treat this disorder that are specific for each type of diabetes. In parallel, new guidelines for the treatment of painful diabetic neuropathy using distinct classes of drugs, with an emphasis on avoiding opioid use, have been issued. Although our understanding of the complexities of diabetic neuropathy has substantially evolved over the past decade, the distinct mechanisms underlying neuropathy in type 1 and type 2 diabetes remains unknown. Future discoveries on disease pathogenesis will be crucial to successfully address all aspects of diabetic neuropathy , from prevention to treatment. The International Diabetes Federation estimates that neuropathies secondary to diabetes can occur (Fig. -

Acanthocytes in the Urine Useful Tool to Differentiate Diabetic Nephropathy from Glomerulonephritis?
Pathophysiology/Complications ORIGINAL ARTICLE Acanthocytes in the Urine Useful tool to differentiate diabetic nephropathy from glomerulonephritis? GUNNAR H. HEINE, MD MATTHIAS GIRNDT, MD of patients who are most likely to have a URBAN SESTER, MD HANS K¨OHLER, MD nondiabetic glomerulopathy and to selec- tively perform renal biopsy in this sub- group of patients. Urinary erythrocyte morphology ex- amined by phase-contrast microscopy al- OBJECTIVE — The presence of hematuria has been suggested to indicate nondiabetic ne- lows to differentiation of glomerular and phropathy in diabetic patients with proteinuria. However, hematuria is frequently found in patients with biopsy-proven diabetic glomerulosclerosis without nondiabetic nephropathy. nonglomerular bleeding (10). Glomeru- Urine microscopy allows discrimination of glomerular hematuria, which is defined as acantho- lar bleeding is indicated by urinary excre- cyturia (urinary excretion of acanthocytes, which are dysmorphic erythrocytes with vesicle-like tion of acanthocytes. Acanthocytes are protrusions), from nonglomerular hematuria. We hypothesized that acanthocyturia is an un- characteristic ring-formed erythrocytes common finding in diabetic nephropathy, which suggests the presence of a nondiabetic ne- with vesicle-shaped protrusions (Fig. 1) phropathy in diabetic patients with proteinuria. (11,12) that have been described previ- ously in the peripheral blood of patients RESEARCH DESIGN AND METHODS — Urine samples of patients with the clinical diagnosis of diabetic nephropathy (n ϭ 68), of patients with biopsy-proven glomerulonephritis suffering from certain hereditary neuro- (n ϭ 43), and of age-matched healthy control subjects (n ϭ 20) were examined by phase-contrast logical disorders (abetalipoproteinemia, microscopy for the presence of hematuria (Ն8 erythrocytes/l) and acanthocyturia. Acantho- chorea-acanthocytosis, and McLeod syn- cyturia of Ն5% (5 acanthocytes among 100 excreted erythrocytes) was classified as glomerular drome) (13). -

Diabetic Nephropathy and Microalbuminuria in Pregnant Women with Type 1 and Type 2 Diabetes Prevalence, Antihypertensive Strategy, and Pregnancy Outcome
Clinical Care/Education/Nutrition/Psychosocial Research ORIGINAL ARTICLE Diabetic Nephropathy and Microalbuminuria in Pregnant Women With Type 1 and Type 2 Diabetes Prevalence, antihypertensive strategy, and pregnancy outcome 1,2 1,2 JULIE AGNER DAMM, MD LENE RINGHOLM, MD, PHD In pregnant women with type 1 di- 1,2 1,4 BJÖRG ASBJÖRNSDÓTTIR, MD BERIT WOETMANN PEDERSEN, MD 1,2 1,2,3 abetes, nephropathy is associated with NICOLINE FOGED CALLESEN ELISABETH R. MATHIESEN, MD, DMSC 1,2 poor pregnancy outcome in terms of JONATHAN M. MATHIESEN increased rates of preeclampsia and pre- term delivery (11–13). In these women, d intrauterine growth restriction (11) oc- OBJECTIVE To evaluate the prevalence of diabetic nephropathy and microalbuminuria in curs almost twice as often as in the general pregnant women with type 2 diabetes in comparison with type 1 diabetes and to describe population (13), and in the late 1990s, pregnancy outcomes in these women following the same antihypertensive protocol. preterm delivery before 34 weeks oc- RESEARCH DESIGN AND METHODSdAmong 220 women with type 2 diabetes and curred in ;30% (13). In women with 445 women with type 1 diabetes giving birth from 2007–2012, 41 women had diabetic ne- type 1 diabetes and microalbuminuria, phropathy (albumin-creatinine ratio $300 mg/g) or microalbuminuria (albumin-creatinine ratio preterm delivery and preeclampsia are 30–299 mg/g) in early pregnancy. Antihypertensive therapy was initiated if blood pressure also frequent and serious complications $ $ 135/85 mmHg or albumin-creatinine ratio 300 mg/g. (11,13,14). RESULTSdThe prevalence of diabetic nephropathy was 2.3% (5 of 220) in women with type 2 In nonpregnant subjects with diabe- diabetes and 2.5% (11 of 445) in women with type 1 diabetes (P =1.00).Thefigures for micro- tes, inhibition of the renin angiotensin albuminuria were 4.5 (10 of 220) vs. -

Nerve Pain in Diabetes
Information O from Your Family Doctor Nerve Pain in Diabetes What is nerve pain in diabetes? feeling in your feet and it affects your balance, Nerve pain with diabetes is called neuropathy there are special shoes that can help. (new-ROP-uh-thee). It is common in people with uncontrolled diabetes. It usually starts in What can I expect? the feet and may go up the legs. It may cause Medicine will lessen the pain for many patients, burning pain or a loss of feeling. but most will still have some pain. It is also important to wear proper fitting shoes. And, What causes it? every time you see the doctor, have the doctor Nerves are like wires that bring feeling to your check your feet for injuries you cannot feel. brain from other parts of the body. High blood sugar levels can damage those nerves. The Where can I get more information? longer you have high blood sugar, the more Your doctor likely you are to get nerve damage. The nerves AAFP’s Patient Education Resource in your feet are usually the first to be damaged. http://familydoctor.org/familydoctor/en/diseases- Nerves in other parts of the body can be conditions/diabetic-neuropathy.html damaged, too. American Diabetes Association http://www.diabetes.org/living-with-diabetes/ How do I know if I have it? complications/neuropathy/peripheral-neuropathy.html If you have nerve damage in your feet, you will National Institutes of Health and National Institute of notice pain or loss of feeling. Your doctor can Diabetes and Digestive and Kidney Diseases do tests to be sure that is what is causing the http://www.niddk.nih.gov/health-information/health- problem.