Reappraisal of Metabolic Dysfunction in Neurodegeneration: Focus on Mitochondrial Function and Calcium Signaling Pooja Jadiya, Joanne F
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Walker's Point Strategic Action Plan MILWAUKEE
MILWAUKEE comprehensive Department of City Development Plan • June, 2015 Walker’s Point Strategic Action Plan A Plan for the Area ii Acknowledgments Neighborhood Associations and Continuum Architects + Planners Interest Groups Ursula Twombly, AIA, LEED AP Arts@Large Walker’s Point Association GRAEF The Mandel Group Greater Milwaukee Committee Larry Witzling, Principal The Harbor District Initiative Craig Huebner, Planner/Urban Designer 12th District Alderman Jose Perez University of Wisconsin - Milwaukee Urban Development Studio City of Milwaukee Department of City Development Carolyn Esswein, AICP, CNU-A, Faculty Member in Charge Rocky Marcoux, Commissioner Vanessa Koster, Planning Manager Sam Leichtling, Long Range Planning Manager Mike Maierle, former Long Range Planning Manager Greg Patin, Strategic Planning Manager Dan Casanova, Economic Development Specialist Janet Grau, Plan Project Manager Nolan Zaroff, Senior Planner GIS, Eco- nomic Development Jeff Poellmann, Planning Intern (Urban Design) Andrew Falkenburg, Planning Intern (GIS/Mapping, Editing) City of Milwaukee Redevelopment Authority David Misky, Assistant Executive Director - Secretary Department of Public Works Mike Loughran, Special Projects Manager Walker’s Point Kristin Bennett, Bicycle Coordinator Strategic Action Plan Historic Preservation Carlen Hatala, Historic Preservation Principal Researcher iii Plan Advisory Group Sean Kiebzak, Arts@Large Juli Kaufmann, Fix Development Dan Adams, Harbor District Initiative Joe Klein, HKS/Junior House Dean Amhaus, Milwaukee Water Council Anthony A. LaCroix Nick & JoAnne Anton, La Perla Scott Luber, Independence First Samer Asad, Envy Nightclub Barry Mandel, The Mandel Group Luis “Tony” Baez, El Centro Hispano Megan & Tyler Mason, Wayward Kitchen Tricia M. Beckwith, Wangard Partners Robert Monnat, The Mandel Group Kristin Bennett, Bike Ped Coordinator Cristina Morales Brigette Breitenbach, Company B Lorna Mueller, The Realty Company, LLC Mike Brenner, Brenner Brewing Co. -

Sculptor Nina Slobodinskaya (1898-1984)
1 de 2 SCULPTOR NINA SLOBODINSKAYA (1898-1984). LIFE AND SEARCH OF CREATIVE BOUNDARIES IN THE SOVIET EPOCH Anastasia GNEZDILOVA Dipòsit legal: Gi. 2081-2016 http://hdl.handle.net/10803/334701 http://creativecommons.org/licenses/by/4.0/deed.ca Aquesta obra està subjecta a una llicència Creative Commons Reconeixement Esta obra está bajo una licencia Creative Commons Reconocimiento This work is licensed under a Creative Commons Attribution licence TESI DOCTORAL Sculptor Nina Slobodinskaya (1898 -1984) Life and Search of Creative Boundaries in the Soviet Epoch Anastasia Gnezdilova 2015 TESI DOCTORAL Sculptor Nina Slobodinskaya (1898-1984) Life and Search of Creative Boundaries in the Soviet Epoch Anastasia Gnezdilova 2015 Programa de doctorat: Ciències humanes I de la cultura Dirigida per: Dra. Maria-Josep Balsach i Peig Memòria presentada per optar al títol de doctora per la Universitat de Girona 1 2 Acknowledgments First of all I would like to thank my scientific tutor Maria-Josep Balsach I Peig, who inspired and encouraged me to work on subject which truly interested me, but I did not dare considering to work on it, although it was most actual, despite all seeming difficulties. Her invaluable support and wise and unfailing guiadance throughthout all work periods were crucial as returned hope and belief in proper forces in moments of despair and finally to bring my study to a conclusion. My research would not be realized without constant sacrifices, enormous patience, encouragement and understanding, moral support, good advices, and faith in me of all my family: my husband Daniel, my parents Andrey and Tamara, my ount Liubov, my children Iaroslav and Maria, my parents-in-law Francesc and Maria –Antonia, and my sister-in-law Silvia. -

Gazeta Winter 2016
Chaim Goldberg, Purim Parade, 1993, oil painting on canvas Volume 23, No. 1 Gazeta Winter 2016 A quarterly publication of the American Association for Polish-Jewish Studies and Taube Foundation for Jewish Life & Culture Editorial & Design: Fay Bussgang, Julian Bussgang, Shana Penn, Vera Hannush, Alice Lawrence, Maayan Stanton, LaserCom Design. Front Cover Photo: Chaim Goldberg; Back Cover Photo: Esther Nisenthal Krinitz J.D. Kirszenbaum, Self-portrait, c. 1925, oil on canvas TABLE OF CONTENTS Message from Irene Pipes ............................................................................................... 1 Message from Tad Taube and Shana Penn ................................................................... 2 RESEARCH PROJECT The Holocaust in the Eyes of Polish Youth By Dr. Jolanta Ambrosewicz-Jacobs .................................................................................. 3 ART AS FAMILY LEGACY A Daughter Returns with Memories in Art By Bernice Steinhardt .......................................................................................................... 7 Resurrection of a Painter: “From Staszów to Paris, via Weimar, Berlin and Rio de Janeiro” By Nathan Diament ........................................................................................................... 12 Creating a New Museum in Kazimierz By Shalom Goldberg ......................................................................................................... 16 CONFERENCES, SPRING/SUMMER PROGRAMS, AND FESTIVALS Conference on Launch of Volume -

Six Canonical Projects by Rem Koolhaas
5 Six Canonical Projects by Rem Koolhaas has been part of the international avant-garde since the nineteen-seventies and has been named the Pritzker Rem Koolhaas Architecture Prize for the year 2000. This book, which builds on six canonical projects, traces the discursive practice analyse behind the design methods used by Koolhaas and his office + OMA. It uncovers recurring key themes—such as wall, void, tur montage, trajectory, infrastructure, and shape—that have tek structured this design discourse over the span of Koolhaas’s Essays on the History of Ideas oeuvre. The book moves beyond the six core pieces, as well: It explores how these identified thematic design principles archi manifest in other works by Koolhaas as both practical re- Ingrid Böck applications and further elaborations. In addition to Koolhaas’s individual genius, these textual and material layers are accounted for shaping the very context of his work’s relevance. By comparing the design principles with relevant concepts from the architectural Zeitgeist in which OMA has operated, the study moves beyond its specific subject—Rem Koolhaas—and provides novel insight into the broader history of architectural ideas. Ingrid Böck is a researcher at the Institute of Architectural Theory, Art History and Cultural Studies at the Graz Ingrid Böck University of Technology, Austria. “Despite the prominence and notoriety of Rem Koolhaas … there is not a single piece of scholarly writing coming close to the … length, to the intensity, or to the methodological rigor found in the manuscript -

May Wingtips
CENTRAL INDIANA SOARING SOCIETY EST. 1960 MAY 1, 2014 CISS WINGTIPS THE MONTHLY VOICE OF INDIANA SOARING In This Issue! ........................................! Sailplane Parts - The Battery Care and Keeping of your! electrical source, pg. 6 Our Towplanes Background and history of these important club assets, page! 5 Badge and Cross Country Camp Get the low down on what to expect, page 10 CISS Hosts Smirnof Vegas, Phoenix, Las Cruces, Odessa, Dallas, Tulsa, St. Louis, Indianapolis, ! Sailplane Derby.... Akron, Pittsburgh, Frederick, MD Octave Chanute The first Forty years ago this month the and Washington, D.C. Contestants gliders in Indiana, page 3 CISS served as one of 11 cities hosting were Ross and Ken Briegleb, Bill contestants in the third annual Holbrook, Hannes Linke, Dan ! Smirno" Sailplane Derby. The event Pierson, Dick Schreder and Karl Plan Your Summer began on May 1, 1974 in Los Angeles Striedieck. ! Vacation Here! The National and moved consecutively to Las Smirnof cont., next page... Soaring! Museum, pg. 9 ! CAESAR CREEK PILOT BREAKS 28 YEAR OLD RECORD Pilot, John Lubon, and his ground crew showed up Bandfel field south of Pittsburg, PA. According at Alexandria airport on Saturday, April 5 for an to John, he never got above 2500 agl after assault on a record held by CISS member, Ron leaving Alex until he passed Dayton, OH. At Clarke for over a quarter of a century. John, who is 6 PM John called Ron to say that he had our Region 6 Director and a highly experienced landed safely and would be filing a claim, cross country flier took advantage of our snatching the coveted record. -

Days & Hours for Social Distance Walking Visitor Guidelines Lynden
53 22 D 4 21 8 48 9 38 NORTH 41 3 C 33 34 E 32 46 47 24 45 26 28 14 52 37 12 25 11 19 7 36 20 10 35 2 PARKING 40 39 50 6 5 51 15 17 27 1 44 13 30 18 G 29 16 43 23 PARKING F GARDEN 31 EXIT ENTRANCE BROWN DEER ROAD Lynden Sculpture Garden Visitor Guidelines NO CLIMBING ON SCULPTURE 2145 W. Brown Deer Rd. Do not climb on the sculptures. They are works of art, just as you would find in an indoor art Milwaukee, WI 53217 museum, and are subject to the same issues of deterioration – and they endure the vagaries of our harsh climate. Many of the works have already spent nearly half a century outdoors 414-446-8794 and are quite fragile. Please be gentle with our art. LAKES & POND There is no wading, swimming or fishing allowed in the lakes or pond. Please do not throw For virtual tours of the anything into these bodies of water. VEGETATION & WILDLIFE sculpture collection and Please do not pick our flowers, fruits, or grasses, or climb the trees. We want every visitor to be able to enjoy the same views you have experienced. Protect our wildlife: do not feed, temporary installations, chase or touch fish, ducks, geese, frogs, turtles or other wildlife. visit: lynden.tours WEATHER All visitors must come inside immediately if there is any sign of lightning. PETS Pets are not allowed in the Lynden Sculpture Garden except on designated dog days. -
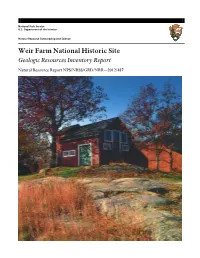
Geologic Resources Inventory Report, Weir
National Park Service U.S. Department of the Interior Natural Resource Stewardship and Science Weir Farm National Historic Site Geologic Resources Inventory Report Natural Resource Report NPS/NRSS/GRD/NRR—2012/487 ON THE COVER View of Julian Alden Weir’s studio in Weir Farm National Historic Site. Rock outcrops, such as those in the foreground, are common throughout the park. The bedrock beneath the park is ancient sea floor sediments that were accreted onto North America, hundreds of millions of years ago. They were deformed and metamorphosed during the construction of the Appalachian Mountains. Photograph by Peter Margonelli, courtesy Allison Herrmann (Weir Farm NHS). THIS PAGE The landscape of the park has inspired artists en plein air for more than 125 years. National Park Service photograph available online: http://www.nps.gov/wefa/photosmultimedia/index.htm (accessed 20 January 2012). Weir Farm National Historic Site Geologic Resources Inventory Report Natural Resource Report NPS/NRSS/GRD/NRR—2012/487 National Park Service Geologic Resources Division PO Box 25287 Denver, CO 80225 January 2012 U.S. Department of the Interior National Park Service Natural Resource Stewardship and Science Fort Collins, Colorado The National Park Service, Natural Resource Stewardship and Science office in Fort Collins, Colorado publishes a range of reports that address natural resource topics of interest and applicability to a broad audience in the National Park Service and others in natural resource management, including scientists, conservation and environmental constituencies, and the public. The Natural Resource Report Series is used to disseminate high-priority, current natural resource management information with managerial application. -

Making an Old-World Milwaukee: German Heritage, Nostalgia, and the Reshaping of the Twentieth Century City Joseph B
University of Wisconsin Milwaukee UWM Digital Commons Theses and Dissertations August 2017 Making an Old-world Milwaukee: German Heritage, Nostalgia, and the Reshaping of the Twentieth Century City Joseph B. Walzer University of Wisconsin-Milwaukee Follow this and additional works at: https://dc.uwm.edu/etd Part of the Ethnic Studies Commons, and the United States History Commons Recommended Citation Walzer, Joseph B., "Making an Old-world Milwaukee: German Heritage, Nostalgia, and the Reshaping of the Twentieth Century City" (2017). Theses and Dissertations. 1719. https://dc.uwm.edu/etd/1719 This Dissertation is brought to you for free and open access by UWM Digital Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UWM Digital Commons. For more information, please contact [email protected]. MAKING AN OLD-WORLD MILWAUKEE: GERMAN HERITAGE, NOSTALGIA AND THE RESHAPING OF THE TWENTIETH CENTURY CITY by Joseph B. Walzer A Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in History at The University of Wisconsin-Milwaukee August 2017 ABSTRACT MAKING AN OLD-WORLD MILWAUKEE: GERMAN HERITAGE, NOSTALGIA AND THE RESHAPING OF THE TWENTIETH CENTURY CITY by Joseph B. Walzer The University of Wisconsin-Milwaukee, 2017 Under the Supervision of Professor Rachel Buff This dissertation examines the importance of white ethnicity, and especially Germanness, in the “civic branding” and urban restructuring efforts of city officials, civic boosters, and business leaders in Milwaukee, Wisconsin in the mid-to-late twentieth century. Scholars have increasingly identified the significant roles the “revival” of European ethnic identities played in maintaining white racial privilege in response to the Civil Rights Movement since the 1960s. -

A Case Study of the Naz Foundation's Campaign to Decriminalize Homosexuality in India Preston G
SIT Graduate Institute/SIT Study Abroad SIT Digital Collections Capstone Collection SIT Graduate Institute Winter 12-4-2017 Lessons for Legalizing Love: A Case Study of the Naz Foundation's Campaign to Decriminalize Homosexuality in India Preston G. Johnson SIT Graduate Institute Follow this and additional works at: https://digitalcollections.sit.edu/capstones Part of the Civic and Community Engagement Commons, Civil Rights and Discrimination Commons, Criminal Law Commons, Gender and Sexuality Commons, History of Gender Commons, Human Rights Law Commons, Law and Gender Commons, Law and Society Commons, Legislation Commons, Lesbian, Gay, Bisexual, and Transgender Studies Commons, Litigation Commons, Policy Design, Analysis, and Evaluation Commons, Political Science Commons, Politics and Social Change Commons, Race, Ethnicity and Post-Colonial Studies Commons, Sexuality and the Law Commons, Social Policy Commons, Sociology of Culture Commons, and the South and Southeast Asian Languages and Societies Commons Recommended Citation Johnson, Preston G., "Lessons for Legalizing Love: A Case Study of the Naz Foundation's Campaign to Decriminalize Homosexuality in India" (2017). Capstone Collection. 3063. https://digitalcollections.sit.edu/capstones/3063 This Thesis (Open Access) is brought to you for free and open access by the SIT Graduate Institute at SIT Digital Collections. It has been accepted for inclusion in Capstone Collection by an authorized administrator of SIT Digital Collections. For more information, please contact [email protected]. -

2020-21 Course Descriptions
2020-21 Course Descriptions Students should consult their success adviser and faculty adviser each quarter prior to registering for courses to be sure they are meeting graduation requirements for their course of study and taking appropriate electives. ACCESSORY DESIGN UNDERGRADUATE ACCE 101 Accessory Design Immersion Students discover the world of fashion accessory design with an in-depth exploration of the evolution of accessory trends, brands and research methodologies. Students learn to sketch accessory concepts, make patterns and select finishing techniques to bring accessory ideas to fruition. Through operating sewing machines, cutting tables and skiving machines students learn how to craft accessories with skill and precision. Prerequisite(s): DRAW 100, DSGN 102, any major or minor except accessory design. ACCE 110 Sewing Technology for Accessory Design This course introduces students to the industry practices involved in producing accessories. Students also are introduced to decorative ornamentation techniques while applying these techniques to accessory design. Basic patternmaking skills are taught and provide the foundation for future courses in accessory design. Prerequisite(s): None. ACCE 120 Materials and Processes for Accessory Design This course introduces students to core materials used in the implementation of accessory design products. By exploring the qualities and properties of traditional materials, students learn the basics of traditional and nontraditional materials. Students explore a variety of techniques related to accessory design with leather, from tanning to production. This course also explores alternative materials used in accessory products such as rubber, synthetics, woods and metals, as well as cements. This course requires experimentation culminating in a final project which explores individualized processes and material manipulation. -

The Piazza Della Signoria: the Visualization of Political Discourse Through Sculpture
THE PIAZZA DELLA SIGNORIA: THE VISUALIZATION OF POLITICAL DISCOURSE THROUGH SCULPTURE A thesis submitted to the College of the Arts of Kent State University in partial fulfillment of the requirements for the degree of Master of Arts by Danielle M. Brady Deibel May, 2017 Thesis written by Danielle M. Brady Deibel B.A., John Carroll University, 2013 M.A., Kent State University, 2017 Approved by ___________________________________________________________ Gustav Medicus, Ph.D., Advisor ___________________________________________________________ Michael Loderstedt, M.F.A., Interim Director, School of Art ___________________________________________________________ John R. Crawford-Spinelli, Ed. D., Dean, College of the Arts TABLE OF CONTENTS Page ACKNOWLEDGMENTS………………………………………………………………………..iv LIST OF FIGURES……………………………………………………………………………….v CHAPTER I. INTRODUCTION………………………………………………………………………………1 II. THE ORIGINS OF THE PIAZZA DELLA SIGNORIA………………………………………3 III.THE JEWISH HEROINE AND HERO CRAFTED BY DONATELLO……………………17 IV. IL GIGANTE: THE AMBIGUITY OF MICHELANGELO………………………………..38 V. CONCLUSION……………………………………………………………………………….54 BIBLIOGRAPHY…………………………………………………………………………..........57 FIGURES………………………………………………………………………………………...60 iii ACKNOWLEDGMENTS First, I would like to thank my advisor Dr. Gustav Medicus, who not only encouraged me to pursue this topic, but answered every one of my detailed questions and helped me through the many different tangents I found myself stuck in. It has been a privilege to be under the tutelage of such an accomplished art historian and engaging person. I also want to thank Dr. Diane Scillia and Dr. Carol Salus for your perspectives and words of reassurance. To Darcy Egan and Kaitie Nock, I offer my unending gratitude for your support, technological savvy, and brilliant editing which kept me motivated to write. To my husband Matthew Deibel, bless you for continuing to believe in my capabilities when I was down or feeling lost. -

Implementation Guide
Implementation Schools Study Guide Earthquakes (Intellectual Output O3) Editors Ivoni Pavlou, Marios Papaevripidou, Zacharias Zacharia Authors Georgios Mavromanolakis, Marianna Potsidi, Manolis Chaniotakis, Sofoklis Sotiriou, Ilias Stouraitis, Giannis Alexopoulos Ellinogermaniki Agogi, Greece Marios Papaevripidou, Ivoni Pavlou, Zacharias Zacharia, Nikoletta Xenofontos, Maria Irakleous, Anna Fiakkou University of Cyprus, Department of Education, Cyprus Bulent Cavas, Elif Dönertaş Yavas, Zeynep Hulagu, Zeynep Ozben, Ismail Aras, Sedriye Guler Bahcesehir Eğitim Kurumları Anonim Şirketi, Turkey Philip Ivanov, Orlin Kouzov, Daniela Pavlova, Radoslav Yoshinov, Stefan Hadjitodorov National Research Network Association, Bulgaria Luigi Cerri, Flora Di Martino Fondazione Idis – Città della Scienza, Italy Date April 2016 (First Release), January 2017 (Revised Version) Dissemination Level Public Status Final 1 Consortium Members Name Organization Abbreviation Country Gerasimos Chouliaras NATIONAL Georgios Drakatos OBSERVATORY OF NOA Greece Maria Staviani ATHENS Georgios Mavromanolakis Marianna Potsidi Manolis Chaniotakis ELLINOGERMANIKI EA Greece Sofoklis Sotiriou AGOGI Ilias Stouraitis Giannis Alexopoulos Yvoni Pavlou Marios Papaevripidou Zacharias Zacharia UNIVERSITY OF CYPRUS UCY Cyprus Nikoletta Xenofontos Maria Irakleous Anna Fiakkou Bulent Cavas Elif Dönertaş Yavas BAHCESEHIR EGITIM Zeynep Ozben KURUMLARI ANONIM BEKAS Turkey Zeynep Hulagu SIRKETI Ismail Aras Sedriye Guler Luigi Cerri FONDAZIONE IDIS-CITTÀ IDIS Italy Flora Di Martino DELLA SCIENZA