A Review of Respiratory Anatomical Development, Air Flow Characterization and Particle Deposition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Infections of the Respiratory Tract
F70954-07.qxd 12/10/02 7:36 AM Page 71 Infections of the respiratory 7 tract the nasal hairs and by inertial impaction with mucus- 7.1 Pathogenesis 71 covered surfaces in the posterior nasopharynx (Fig. 11). 7.2 Diagnosis 72 The epiglottis, its closure reflex and the cough reflex all reduce the risk of microorganisms reaching the lower 7.3 Management 72 respiratory tract. Particles small enough to reach the tra- 7.4 Diseases and syndromes 73 chea and bronchi stick to the respiratory mucus lining their walls and are propelled towards the oropharynx 7.5 Organisms 79 by the action of cilia (the ‘mucociliary escalator’). Self-assessment: questions 80 Antimicrobial factors present in respiratory secretions further disable inhaled microorganisms. They include Self-assessment: answers 83 lysozyme, lactoferrin and secretory IgA. Particles in the size range 5–10 µm may penetrate further into the lungs and even reach the alveolar air Overview spaces. Here, alveolar macrophages are available to phagocytose potential pathogens, and if these are overwhelmed neutrophils can be recruited via the This chapter deals with infections of structures that constitute inflammatory response. The defences of the respira- the upper and lower respiratory tract. The general population tory tract are a reflection of its vulnerability to micro- commonly experiences upper respiratory tract infections, bial attack. Acquisition of microbial pathogens is which are often seen in general practice. Lower respiratory tract infections are less common but are more likely to cause serious illness and death. Diagnosis and specific chemotherapy of respiratory tract infections present a particular challenge to both the clinician and the laboratory staff. -

Microbial Biogeography and Ecology of the Mouth and Implications for Periodontal
bioRxiv preprint doi: https://doi.org/10.1101/541052; this version posted February 8, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. This article is a US Government work. It is not subject to copyright under 17 USC 105 and is also made available for use under a CC0 license. Microbial biogeography and ecology of the mouth and implications for periodontal diseases Authors: Diana M. Proctor1,2,10, Katie M. Shelef3,10, Antonio Gonzalez4, Clara L. Davis Long5, Les Dethlefsen1, Adam Burns1, Peter M. Loomer6, Gary C. Armitage7, Mark I. Ryder7, Meredith E. Millman7, Rob Knight4, Susan P. Holmes8, David A. Relman1,5,9 Affiliations 1Division of Infectious Disease & Geographic Medicine, Department of Medicine, Stanford University School of Medicine, Stanford, CA 94305 USA 2National Human Genome Research Institute, National Institutes of Health, Bethesda, MD 20892 USA 3Department of Biology, Stanford University School of Medicine, Stanford, CA 94305 USA 4Departments of Pediatrics and Computer Science and Engineering, University of California at San Diego, La Jolla, CA 92093 USA 5Department of Microbiology & Immunology, Stanford University School of Medicine, Stanford, CA 94305 USA 6Ashman Department of Periodontology & Implant Dentistry, New York University College of Dentistry, New York, NY 10010 USA 7Division of Periodontology, University of California, San Francisco School of Dentistry, San Francisco, CA 94143 USA 8Department of Statistics, Stanford University, Stanford, CA 94305 USA 9Veterans Affairs Palo Alto Health Care System, Palo Alto, CA 94304 USA 10These authors contributed equally Corresponding author: David A. Relman: [email protected]; Address: Encina E209, 616 Serra Street, Stanford, California 94305-6165; Phone: 650-736-6822; Fax: 650-852-3291 1 bioRxiv preprint doi: https://doi.org/10.1101/541052; this version posted February 8, 2019. -

Maximum Expiratory Flow Rates in Induced Bronchoconstriction in Man
Maximum expiratory flow rates in induced bronchoconstriction in man A. Bouhuys, … , B. M. Kim, A. Zapletal J Clin Invest. 1969;48(6):1159-1168. https://doi.org/10.1172/JCI106073. Research Article We evaluated changes of maximum expiratory flow-volume (MEFV) curves and of partial expiratory flow-volume (PEFV) curves caused by bronchoconstrictor drugs and dust, and compared these to the reverse changes induced by a bronchodilator drug in previously bronchoconstricted subjects. Measurements of maximum flow at constant lung inflation (i.e. liters thoracic gas volume) showed larger changes, both after constriction and after dilation, than measurements of peak expiratory flow rate, 1 sec forced expiratory volume and the slope of the effort-independent portion of MEFV curves. Changes of flow rates on PEFV curves (made after inspiration to mid-vital capacity) were usually larger than those of flow rates on MEFV curves (made after inspiration to total lung capacity). The decreased maximum flow rates after constrictor agents are not caused by changes in lung static recoil force and are attributed to narrowing of small airways, i.e., airways which are uncompressed during forced expirations. Changes of maximum expiratory flow rates at constant lung inflation (e.g. 60% of the control total lung capacity) provide an objective and sensitive measurement of changes in airway caliber which remains valid if total lung capacity is altered during treatment. Find the latest version: https://jci.me/106073/pdf Maximum Expiratory Flow Rates in Induced Bronchoconstriction in Man A. Bouiuys, V. R. HuNTr, B. M. Kim, and A. ZAPLETAL From the John B. Pierce Foundation Laboratory and the Yale University School of Medicine, New Haven, Connecticut 06510 A B S T R A C T We evaluated changes of maximum ex- rates are best studied as a function of lung volume. -

Dynamic Evaluation of Forces During Mastication
Project Number: ME-SYS-0787 Dynamic Evaluation of Forces During Mastication A Major Qualifying Project Submitted to the Faculty of WORCESTER POLYTECHNIC INSTITUTE In partial fulfillment of requirements for the Degree of Bachelor of Science By Justin McGarry Anthony Spangenberger Date: Approval: Professor Satya Shivkumar, Advisor Abstract A reproduction of the human masticatory system is presented here to evaluate mechanical properties of foods, relevant design elements of the simulator, and the overall practicality of the system. The model incorporates a cam-driven linkage system providing realistic motion of the mandible, with reaction forces measured by strain gages on two axes to record real time changes in food structure. The experiment demonstrates that the construction of a mastication simulator is feasible and allows texture profiling and discrimination between similar foods. i Acknowledgements Our MQP was completed with the help of several individuals who offered professional advice and technical guidance. We would like to thank Prof. Satya Shivkumar, our project advisor, for guiding us with his extensive knowledge of materials and testing procedures, Prof. John Hall for his help with the sensors used in this project and his willingness to lend some of the necessary equipment, Prof. Robert Norton for his advice on the fixture design, Fred Hutson for lending equipment from the physics department for use in calibration of the fixture, Randy Robinson for the computer used for recording data, Neil Whitehouse, Toby Bergstrom, and Adam -

Peak Flow Measure: an Index of Respiratory Function?
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Original Research Article Peak Flow Measure: An Index of Respiratory Function? D. Devadiga, Aiswarya Liz Varghese, J. Bhat, P. Baliga, J. Pahwa Department of Audiology and Speech Language Pathology, Kasturba Medical College (A Unit of Manipal University), Mangalore -575001 Corresponding Author: Aiswarya Liz Varghese Received: 06/12/2014 Revised: 26/12/2014 Accepted: 05/01/2015 ABSTRACT Aerodynamic analysis is interpreted as a reflection of the valving activity of the larynx. It involves measuring changes in air volume, flow and pressure which indicate respiratory function. These measures help in determining the important aspects of lung function. Peak expiratory flow rate is a widely used respiratory measure and is an effective measure of effort dependent airflow. Aim: The aim of the current study was to study the peak flow as an aerodynamic measure in healthy normal individuals Method: The study group was divided into two groups with n= 60(30 males and 30 females) in the age range of 18-22 years. The peak flow was measured using Aerophone II (Voice Function Analyser). The anthropometric measurements such as height, weight and Body Mass Index was calculated for all the participants. Results: The peak airflow was higher in females as compared to that of males. It was also observed that the peak air flow rate was correlating well with height and weight in males. Conclusions: Speech language pathologist should consider peak expiratory airflow, a short sharp exhalation rate as a part of routine aerodynamic evaluation which is easier as compared to the otherwise commonly used measure, the vital capacity. -
UCDH Dental Hygiene Glossary Editorial Compilation/Consultant Special Thanks
UCDH Dental Hygiene Glossary A Faculty/Student Venture Editorial Compilation/Consultant Brent Molen RDH, Med College President/Chief Operations Officer Assistant Professor, The Utah College of Dental Hygiene at Careers Unlimited Special Thanks A special thanks goes out to all the dental hygiene students of the classes of 2009, 2010, and 2011 who have helped make this venture possible and who have contributed their efforts to it. The information contained in this glossary is to be used by the dental hygiene professional only and for dental education purposes only. It is not intended for the general public. Any sale, distribution, copying, dissemination, or duplication of this glossary without written permission is strictly prohibited. If you have received this glossary electronically in error, please call (801) 426-8234 (USA) or notify by return email [email protected] immediately & delete or destroy the digital file. Copyright 2010 Careers Unlimited L.L.C. UCDH is a division of Careers Unlimited L.L.C. Abducens Nerve: the sixth cranial nerve, which controls movement of one single muscle, the lateral rectus muscle, of the eye. Abrasive: to scratch a surface or have rough texture being able to remove a layer. Abscess: the destruction of tissue due to activity of bacteria producing pus, pain and swelling as result of microscopic cellular activity. Abuse: to do harm or wrong doing to others or yourself; by physical or chemical means. Abutment: a tooth, root or implant that serves as the support or anchor to a denture or a fixed or removable bridge. See pontics. Abutment: a tooth, root, or implant that supports and maintains position of a fixed or removable prosthesis. -

Introduction to Airway Resistance Measurements
Introduction to airway resistance measurements Dr. David Kaminsky Department of Medicine The University of Vermont VT 05405 Burlington UNITED STATES OF AMERICA [email protected] AIMS Review physiology of airway resistance Survey measures of airway resistance Provide examples of clinical applications Highlight research applications SUMMARY Airway resistance (Raw) is one of the fundamental features of the mechanics of the respiratory system. While the flow-volume loop offers insight into the volume and flow of air, it is limited in terms of specific information regarding lung mechanics. Airway resistance is the ratio of driving pressure divided by flow through the airways. It specifies the pressure required to achieve a flow of air with a velocity of 1L/sec. If the airway is represented by a simple, rigid tube, with laminar flow of air through it, the airway resistance Raw = (8 x L x )/ r4, where L = length of the tube, = viscosity of the gas, and r = radius of the tube. It is important to note that the r4 relationship demonstrates how sensitive resistance is to the size of the tube, varying inversely with the 4th power of the radius. The inner diameter of the airway is itself determined by many factors, including airway smooth muscle contractile state, airway wall thickness (related to inflammation, edema and remodeling), airway wall buckling and formation of mucosal folds, the interdependence, or linkage, of airway and surrounding lung parenchyma, and the intrinsic elastic recoil of the lung parenchyma, which serves as a load on the airway and variably resists bronchoconstriction. Of course, the airways are not rigid tubes, and in fact flow is a complex process involving both laminar and turbulent conditions, so this calculation of Raw is an approximation only. -
Forensic Archaeology & Forensic Anthropology
Forensic Archaeology & Forensic Anthropology ADJ14 Advanced Criminal Investigations Anthropology & Archaeology ´ Anthropology is the study of the biological and cultural aspects of all humans in all places in all times. ´ Archaeology is the study of human history and prehistory through the excavation of sites and the analysis of artifacts and other physical remains. Introduction to Forensic Archaeology & Forensic Anthropology ´ Forensic Anthropology is the field of study that deals with the analysis of human skeletal remains resulting from unexplained deaths. Experts in the discipline, because of their understanding of skeletal biology, examine human bones with the goal of extracting information about persons represented by skeletal remains and circumstances surrounding death (Byers, 2011). ´ Forensic Archaeology is a subfield of forensic anthropology, and forensic archaeology is the forensic application of archaeological techniques. Archaeology is the study of humans, both modern and ancient. Specifically, forensic archeologists perform the controlled recovery of human remains and other evidence at forensic scenes. Proper archeological procedures generally require significant time and attention to detail, and so the process may seem rather slow to investigators. However, the end result of this effort is the ability to exactly reconstruct the entire scene as it appeared before excavation (Nawracki, 1996). Forensic Anthropology ´ Forensic anthropologists attempt to accomplish 5 main objectives in their work: ① When soft tissue has deteriorated to the point that demographic characteristics of a body cannot be determined by visual inspection, they attempt to determine ancestry, sex, age, and living height from the skeleton. ② When there is evidence of traumatic injury (bullet holes, stab wounds, fractures) to human bone, forensic anthropologists attempt to identify the nature of the traumas and their causative agent pertaining to cause and manner of death. -
Spirometry Basics
SPIROMETRY BASICS ROSEMARY STINSON MSN, CRNP THE CHILDREN’S HOSPITAL OF PHILADELPHIA DIVISION OF ALLERGY AND IMMUNOLOGY PORTABLE COMPUTERIZED SPIROMETRY WITH BUILT IN INCENTIVES WHAT IS SPIROMETRY? Use to obtain objective measures of lung function Physiological test that measures how an individual inhales or exhales volume of air Primary signal measured–volume or flow Essentially measures airflow into and out of the lungs Invaluable screening tool for respiratory health compared to BP screening CV health Gold standard for diagnosing and measuring airway obstruction. ATS, 2005 SPIROMETRY AND ASTHMA At initial assessment After treatment initiated and symptoms and PEF have stabilized During periods of progressive or prolonged asthma control At least every 1-2 years: more frequently depending on response to therapy WHY NECESSARY? o To evaluate symptoms, signs or abnormal laboratory tests o To measure the effect of disease on pulmonary function o To screen individuals at risk of having pulmonary disease o To assess pre-operative risk o To assess prognosis o To assess health status before beginning strenuous physical activity programs ATS, 2005 SPIROMETRY VERSUS PEAK FLOW Recommended over peak flow meter measurements in clinician’s office. Variability in predicted PEF reference values. Many different brands PEF meters. Peak Flow is NOT a diagnostic tool. Helpful for monitoring control. EPR 3, 2007 WHY MEASURE? o Some patients are “poor perceivers.” o Perception of obstruction variable and spirometry reveals obstruction more severe. o Family members “underestimate” severity of symptoms. o Objective assessment of degree of airflow obstruction. o Pulmonary function measures don’t always correlate with symptoms. o Comprehensive assessment of asthma. -
3-D Surface Anthropometry: Review of Technologies (L'hthropodtrie De Surface-En Trois Dimensions: Examen Des Technologies)
I 1 n A L 1 W ADVISORY QROUP FOR AEROSPACE RE(KARCH & DEVELOPMENT 7 RUE ANCEUE, 92200 NEUIUY-SUR-SEINE, FRANCE 3-D Surface Anthropometry: Review of Technologies (l'hthropodtrie de surface-en trois dimensions: examen des technologies) . \ AGARD-AR-329 I I ADVISORY GROUP FOR AEROSPACE RESEARCH & DEVELOPMENT 7 RUE ANCELLE, 92200 NEUILLY-SUR-SEINE, FRANCE AGARD ADVISORY REPORT 329 I- I. 3-D Surface Anthropometry: Review of Technologies (1'AnthropomCtrie de surface en trois dimensions: examen des technologies) Editors: K.M. Robinette (US), M.W. Vannier (US), M. Rioux (CA), P.R.M. Jones (UK) This Advisory Report was prepared by Working Group 20 of the Aerospace Medical Panel of AGARD. North Atlantic Treaty Organization Organisation du Traite de I'Atlantique Nord I The Mission of AGARD According to its Charter, the mission of AGARD is to bring together the leading personalities of the NATO nations in the fields of science and technology relating to aerospace for the following purposes: - Recommending effective ways for the member nations to use their research and development capabilities for the common benefit of the NATO community; - Providing scientific and technical advice and assistance to the Military Committee in the field of aerospace research and development (with particular regard to its military application); - Continuously stimulating advances in the aerospace sciences relevant to strengthening the common defence posture; - Improving the co-operation among member nations in aerospace research and development;, - Exchange of scientific and technical information; - Providing assistance to member nations for the purpose of increasing their scientific and technical potential; - Rendering scientific and technical assistance, as requested, to other NATO bodies and to member nations in connection with research and development problems in the aerospace field. -
The Respiratory System
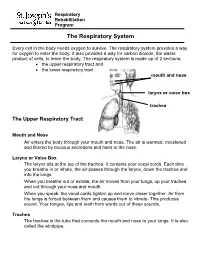
Respiratory Rehabilitation Program The Respiratory System Every cell in the body needs oxygen to survive. The respiratory system provides a way for oxygen to enter the body. It also provides a way for carbon dioxide, the waste product of cells, to leave the body. The respiratory system is made up of 2 sections: the upper respiratory tract and the lower respiratory tract mouth and nose larynx or voice box trachea The Upper Respiratory Tract Mouth and Nose Air enters the body through your mouth and nose. The air is warmed, moistened and filtered by mucous secretions and hairs in the nose. Larynx or Voice Box The larynx sits at the top of the trachea. It contains your vocal cords. Each time you breathe in or inhale, the air passes through the larynx, down the trachea and into the lungs. When you breathe out or exhale, the air moves from your lungs, up your trachea and out through your nose and mouth. When you speak, the vocal cords tighten up and move closer together. Air from the lungs is forced between them and causes them to vibrate. This produces sound. Your tongue, lips and teeth form words out of these sounds. Trachea The trachea is the tube that connects the mouth and nose to your lungs. It is also called the windpipe. The Lower Respiratory Tract Inside Lungs Outside Lungs bronchial tubes alveoli diaphragm (muscle) Bronchial Tubes The trachea splits into 2 bronchial tubes in your lungs. These are called the left bronchus and right bronchus. The bronchus tubes keep branching off into smaller and smaller tubes called bronchi. -

RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J
OFP PATIENT EDUCATION HANDOUT RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J. Keenum, DO, PharmD, Editor • Ronald Januchowski, DO, FACOFP, Health Literacy Editor HOME MANAGEMENT INCLUDES: • Drinking plenty of clear fuids and rest. Vitamin-C may help boost your immune system. Over-the-counter pain relievers such as acetaminophen and ibuprofen can be helpful for fevers and to ease any aches. Saline (salt) nose drops, lozenges, and vapor rubs can also help symptoms when used as directed by your physician. • A cool mist humidifer can make breathing easier by thinning mucus. • If you smoke, you should try to stop smoking for good! Avoid second-hand smoking also. • In most cases, antibiotics are not recommended because they are only effective if bacteria caused the infection. • Other treatments, that your Osteopathic Family Physician may prescribe, include Osteopathic Manipulative Therapy (OMT). OMT can help clear mucus, Respiratory tract infections are any relieve congestion, improve breathing and enhance comfort, relaxation, and infection that affect the nose, sinuses, immune function. and throat (i.e. the upper respiratory tract) or airways and lungs (i.e. the • Generally, the symptoms of a respiratory tract infection usually pass within lower respiratory tract). Viruses are one to two weeks. the main cause of the infections, but • To prevent spreading infections, sneeze into the arm of your shirt or in a tissue. bacteria can cause some. You can Also, practice good hygiene such as regularly washing your hands with soap and spread the infection to others through warm water. Wipe down common surfaces, such as door knobs and faucet handles, the air when you sneeze or cough.