* Thromboembolic Disease Antithrombotic Therapy for Venous
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao Et Al
USOO9498481 B2 (12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao et al. (45) Date of Patent: *Nov. 22, 2016 (54) CYCLOPROPYL MODULATORS OF P2Y12 WO WO95/26325 10, 1995 RECEPTOR WO WO99/O5142 2, 1999 WO WOOO/34283 6, 2000 WO WO O1/92262 12/2001 (71) Applicant: Apharaceuticals. Inc., La WO WO O1/922.63 12/2001 olla, CA (US) WO WO 2011/O17108 2, 2011 (72) Inventors: Tadimeti Rao, San Diego, CA (US); Chengzhi Zhang, San Diego, CA (US) OTHER PUBLICATIONS Drugs of the Future 32(10), 845-853 (2007).* (73) Assignee: Auspex Pharmaceuticals, Inc., LaJolla, Tantry et al. in Expert Opin. Invest. Drugs (2007) 16(2):225-229.* CA (US) Wallentin et al. in the New England Journal of Medicine, 361 (11), 1045-1057 (2009).* (*) Notice: Subject to any disclaimer, the term of this Husted et al. in The European Heart Journal 27, 1038-1047 (2006).* patent is extended or adjusted under 35 Auspex in www.businesswire.com/news/home/20081023005201/ U.S.C. 154(b) by Od en/Auspex-Pharmaceuticals-Announces-Positive-Results-Clinical M YW- (b) by ayS. Study (published: Oct. 23, 2008).* This patent is Subject to a terminal dis- Concert In www.concertpharma. com/news/ claimer ConcertPresentsPreclinicalResultsNAMS.htm (published: Sep. 25. 2008).* Concert2 in Expert Rev. Anti Infect. Ther. 6(6), 782 (2008).* (21) Appl. No.: 14/977,056 Springthorpe et al. in Bioorganic & Medicinal Chemistry Letters 17. 6013-6018 (2007).* (22) Filed: Dec. 21, 2015 Leis et al. in Current Organic Chemistry 2, 131-144 (1998).* Angiolillo et al., Pharmacology of emerging novel platelet inhibi (65) Prior Publication Data tors, American Heart Journal, 2008, 156(2) Supp. -

Characterising the Risk of Major Bleeding in Patients With
EU PE&PV Research Network under the Framework Service Contract (nr. EMA/2015/27/PH) Study Protocol Characterising the risk of major bleeding in patients with Non-Valvular Atrial Fibrillation: non-interventional study of patients taking Direct Oral Anticoagulants in the EU Version 3.0 1 June 2018 EU PAS Register No: 16014 EMA/2015/27/PH EUPAS16014 Version 3.0 1 June 2018 1 TABLE OF CONTENTS 1 Title ........................................................................................................................................... 5 2 Marketing authorization holder ................................................................................................. 5 3 Responsible parties ................................................................................................................... 5 4 Abstract ..................................................................................................................................... 6 5 Amendments and updates ......................................................................................................... 7 6 Milestones ................................................................................................................................. 8 7 Rationale and background ......................................................................................................... 9 8 Research question and objectives .............................................................................................. 9 9 Research methods .................................................................................................................... -
Sulodexide: Review of Recent Clinical Efficacy Data
ISSN 2277-0879; Volume 2, Issue 5, pp. 57-61; May, 2013 Online Journal of Medicine and Medical Science Research ©2013 Online Research Journals Review Article Available Online at http://www.onlineresearchjournals.org/JMMSR Sulodexide: Review of recent clinical efficacy data Massimo Milani MD Private practice, Milan Italy, Via A. Nota 18, Milan, Italy. E-Mail: [email protected]. Received 17 April, 2013 Accepted 8 May, 2013 Sulodexide (SLX) is a peculiar and interesting antithrombotic drug. It is a highly purified mixture of glycosaminoglycans (GAG) with anticoagulant and antithrombotic properties used for the prophylaxis and treatment of thromboembolic diseases. The pharmacological effects of SLX differ substantially from other GAG and are mainly characterized by a prolonged half-life and reduced effect on global coagulation and bleeding parameters. SLX is able to potentiate the antiprotease activities of both antithrombin III and heparin cofactor II. SLX shows also in vitro and in vivo profibrinolytic actions. SLX exhibits antithrombotic and profibrinolytic properties in several animal models of venous and arterial thrombosis and has relatively high affinity for endothelial cells. By oral route SLX is able to release tissue plasminogen activator and increase fibrinolytic activities. SLX is clinically effective in the treatment of peripheral arterial vascular diseases and in the treatment of deep venous thrombosis. SLX has also been found clinically active in the treatment of venous ulcers of the leg. SLX has been also used with success in tinnitus and in the thrombosis of central ocular vein. Recent data suggest that SLX could have beneficial effects in the treatment of diabetic nephropathy and in reducing microalbuminuria. -
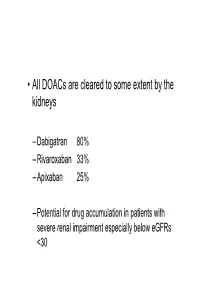
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -

Spontaneous Epidural Hematoma of the Cervical Spine Following Thrombolysis in a Patient with STEMI—Two Medical Specialties Facing a Rare Dilemma
Published online: 2019-12-05 THIEME Case Report 191 Spontaneous Epidural Hematoma of the Cervical Spine Following Thrombolysis in a Patient with STEMI—Two Medical Specialties Facing a Rare Dilemma Anastasios Tsarouchas1 Dimitrios Mouselimis1 Constantinos Bakogiannis1 Grigorios Gkasdaris2 George Dimitriadis3 Dimitrios Zioutas4 Christodoulos E. Papadopoulos1 13rd Cardiology Department, Hippokrateio University Hospital, Address for correspondence Grigorios Gkasdaris, MD, Department Aristotle University of Thessaloniki, Thessaloniki, Greece of Neurosurgery, KAT General Hospital of Attica, Athens 145 61, 2Department of Neurosurgery, KAT General Hospital of Attica, Greece (e-mail: [email protected]). Athens, Greece 3General Hospital of Katerini, Katerini, Greece 4St. Luke’s Hospital, Thessaloniki, Greece J Neurosci Rural Pract 2020;11:191–195 Abstract Spontaneous spinal epidural hematoma (SSEH) is a rare, albeit well-documented complication following thrombolysis treatment in ST elevation myocardial infarction (STEMI). A SSEH usually manifests with cervical pain and neurologic deficits and may require surgical intervention. In this case report, we present the first reported SSEH to occur following thrombolysis with reteplase. In this case, the SSEH manifested with cervical pain shortly after the patient emerged from his rescue percutaneous coronary intervention (PCI). Although magnetic resonance imaging reported spinal cord com- Keywords pression, the lack of neurologic symptoms prompted the treating clinicians to delay ► spinal epidural surgery. A dangerous dilemma emerged, as the usual antithrombotic regimen that hematoma was necessary to avoid stent thrombosis post-PCI, was also likely to exacerbate the ► spontaneous spinal bleeding. As a compromise, the patient only received aspirin as a single antiplatelet epidural hematoma therapy. Ultimately, the patient responded well to conservative treatment, with the ► cervical spine hematoma stabilizing a week later, without residual neurologic deficits. -

Treatment for Superficial Thrombophlebitis of The
Treatment for superficial thrombophlebitis of the leg (Review) Di Nisio M, Wichers IM, Middeldorp S This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2012, Issue 3 http://www.thecochranelibrary.com Treatment for superficial thrombophlebitis of the leg (Review) Copyright © 2012 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 3 METHODS ...................................... 3 RESULTS....................................... 5 Figure1. ..................................... 7 Figure2. ..................................... 8 DISCUSSION ..................................... 11 AUTHORS’CONCLUSIONS . 12 ACKNOWLEDGEMENTS . 12 REFERENCES ..................................... 12 CHARACTERISTICSOFSTUDIES . 17 DATAANDANALYSES. 42 Analysis 1.1. Comparison 1 Fondaparinux versus placebo, Outcome 1 Pulmonary embolism. 51 Analysis 1.2. Comparison 1 Fondaparinux versus placebo, Outcome 2 Deep vein thrombosis. 51 Analysis 1.3. Comparison 1 Fondaparinux versus placebo, Outcome 3 Deep vein thrombosis and pulmonary embolism. 52 Analysis 1.4. Comparison 1 Fondaparinux versus placebo, Outcome 4 Extension of ST. 52 Analysis 1.5. Comparison 1 Fondaparinux versus placebo, Outcome 5 Recurrence of ST. 53 Analysis 1.6. Comparison 1 Fondaparinux -

Anticoagulation Reversal Guideline for Adults
Anticoagulation Reversal Guideline for Adults Antithrombotic reversal strategies should be limited to clinical situations (i.e. life-threatening bleeding) where the immediate need for anticoagulant reversal outweighs the risk of thrombosis (either from the reversal agent itself or normalization of coagulation in a patient with underlying thromboembolic risk). These recommendations are meant to serve as general guidelines and should not replace clinical judgment. Always seek input from the appropriate specialists when indicated and include the patient and/or family in shared decision making when possible. This document is not meant to guide selection of patients for reversal therapies. Please refer to appropriate national guidelines to aide decision- making regarding need for reversal, if warranted. 1. ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants 2. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine All indications for anticoagulation are considered, including atrial fibrillation, venous thromboembolism, prosthetic cardiac valves, and intracardiac thrombus. Mechanical circulatory support devices, including temporary or permanent ventricular assist devices (i.e. LVADs), are excluded from this document. Whenever possible, anticoagulation should be resumed in a timely manner to avoid thromboembolic complications related to the underlying indication for anticoagulation. This guideline does not provide recommendations on resuming anticoagulation. References: • Tomaselli GF, Mahaffey KW, Cuker A, et al. 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Experts Consensus Decisions Pathways. J Am Coll Cardiol. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Pharmaceutical Services Division and the Clinical Research Centre Ministry of Health Malaysia
A publication of the PHARMACEUTICAL SERVICES DIVISION AND THE CLINICAL RESEARCH CENTRE MINISTRY OF HEALTH MALAYSIA MALAYSIAN STATISTICS ON MEDICINES 2008 Edited by: Lian L.M., Kamarudin A., Siti Fauziah A., Nik Nor Aklima N.O., Norazida A.R. With contributions from: Hafizh A.A., Lim J.Y., Hoo L.P., Faridah Aryani M.Y., Sheamini S., Rosliza L., Fatimah A.R., Nour Hanah O., Rosaida M.S., Muhammad Radzi A.H., Raman M., Tee H.P., Ooi B.P., Shamsiah S., Tan H.P.M., Jayaram M., Masni M., Sri Wahyu T., Muhammad Yazid J., Norafidah I., Nurkhodrulnada M.L., Letchumanan G.R.R., Mastura I., Yong S.L., Mohamed Noor R., Daphne G., Kamarudin A., Chang K.M., Goh A.S., Sinari S., Bee P.C., Lim Y.S., Wong S.P., Chang K.M., Goh A.S., Sinari S., Bee P.C., Lim Y.S., Wong S.P., Omar I., Zoriah A., Fong Y.Y.A., Nusaibah A.R., Feisul Idzwan M., Ghazali A.K., Hooi L.S., Khoo E.M., Sunita B., Nurul Suhaida B.,Wan Azman W.A., Liew H.B., Kong S.H., Haarathi C., Nirmala J., Sim K.H., Azura M.A., Asmah J., Chan L.C., Choon S.E., Chang S.Y., Roshidah B., Ravindran J., Nik Mohd Nasri N.I., Ghazali I., Wan Abu Bakar Y., Wan Hamilton W.H., Ravichandran J., Zaridah S., Wan Zahanim W.Y., Kannappan P., Intan Shafina S., Tan A.L., Rohan Malek J., Selvalingam S., Lei C.M.C., Ching S.L., Zanariah H., Lim P.C., Hong Y.H.J., Tan T.B.A., Sim L.H.B, Long K.N., Sameerah S.A.R., Lai M.L.J., Rahela A.K., Azura D., Ibtisam M.N., Voon F.K., Nor Saleha I.T., Tajunisah M.E., Wan Nazuha W.R., Wong H.S., Rosnawati Y., Ong S.G., Syazzana D., Puteri Juanita Z., Mohd. -

Full Prescribing Information for - Active Internal Bleeding (4) RETAVASE
HIGHLIGHTS OF PRESCRIBING INFORMATION CONTRAINDICATIONS These highlights do not include all the information needed to use • Do not use in patients with: RETAVASE safely and effectively. See full prescribing information for - Active internal bleeding (4) RETAVASE. - Recent stroke (4) - Recent intracranial or intraspinal surgery or serious head trauma (4) RETAVASE (reteplase) for injection, for intravenous use - Intracranial neoplasm, arteriovenous malformation, or aneurysm (4) Initial U.S. Approval: 1996 - Known bleeding diathesis (4) - Severe uncontrolled hypertension (4) INDICATIONS AND USAGE RETAVASE is a tissue plasminogen activator (tPA) indicated for treatment of WARNINGS AND PRECAUTIONS acute ST-elevation myocardial infarction (STEMI) to reduce the risk of death • Increases the risk of bleeding. Avoid intramuscular injections. (5.1) and heart failure. (1) • Hypersensitivity (5.2) • Cholesterol embolism (5.3) Limitation of Use: The risk of stroke may outweigh the benefit produced by thrombolytic therapy in patients whose STEMI puts them at low risk for death ADVERSE REACTIONS or heart failure. (1) The most common adverse reaction (>5%) is bleeding. (6.1) DOSAGE AND ADMINISTRATION To report SUSPECTED ADVERSE REACTIONS, contact Chiesi USA, • Two 10 unit intravenous injections, each administered over 2 minutes, Inc. at 1-888-661-9260 or FDA at 1-800-FDA-1088 or 30 minutes apart. (2.1) www.fda.gov/medwatch. • No other medication should be injected or infused simultaneously via the same intravenous line or added to the injection solution. (2.1) USE IN SPECIFIC POPULATIONS • Pediatric Use: Safety and effectiveness have not been established. (8.4) DOSAGE FORMS AND STRENGTHS For Injection: 10 units as a lyophilized powder in single-use vials for Revised: 10/2020 reconstitution co-packaged with Sterile Water for Injection, USP in 10 mL prefilled syringe. -

Predicting Potential Drugs for Breast Cancer Based on Mirna and Tissue Specificity
Int. J. Biol. Sci. 2018, Vol. 14 971 Ivyspring International Publisher International Journal of Biological Sciences 2018; 14(8): 971-982. doi: 10.7150/ijbs.23350 Research Paper Predicting Potential Drugs for Breast Cancer based on miRNA and Tissue Specificity Liang Yu, Jin Zhao and Lin Gao School of Computer Science and Technology, Xidian University, Xi'an, 710071, P.R. China. Corresponding author: [email protected] © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2017.10.16; Accepted: 2017.12.14; Published: 2018.05.22 Abstract Network-based computational method, with the emphasis on biomolecular interactions and biological data integration, has succeeded in drug development and created new directions, such as drug repositioning and drug combination. Drug repositioning, that is finding new uses for existing drugs to treat more patients, offers time, cost and efficiency benefits in drug development, especially when in silico techniques are used. MicroRNAs (miRNAs) play important roles in multiple biological processes and have attracted much scientific attention recently. Moreover, cumulative studies demonstrate that the mature miRNAs as well as their precursors can be targeted by small molecular drugs. At the same time, human diseases result from the disordered interplay of tissue- and cell lineage-specific processes. However, few computational researches predict drug-disease potential relationships based on miRNA data and tissue specificity. Therefore, based on miRNA data and the tissue specificity of diseases, we propose a new method named as miTS to predict the potential treatments for diseases.