Guideline for Reversal of Antithrombotics in Intracranial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effectiveness of Preemptive Antifibrinolysis with Tranexamic Acid
Lei et al. BMC Musculoskeletal Disorders (2020) 21:465 https://doi.org/10.1186/s12891-020-03488-8 STUDY PROTOCOL Open Access Effectiveness of preemptive antifibrinolysis with tranexamic acid in rheumatoid arthritis patients undergoing total knee arthroplasty: a study protocol for a randomized controlled trial Yiting Lei1†, Jiacheng Liu1†, Xi Liang1, Ning Hu1, Fuxing Pei2 and Wei Huang1* Abstract Background: Patients with rheumatoid arthritis (RA) who have undergone total knee arthroplasty are at increased risk of requiring a blood transfusion. This study is designed to compare the effects of preemptive antifibrinolysis of single-dose and repeat-dose tranexamic acid (TXA) in in RA patients undergoing total knee arthroplasty (TKA). Methods/design: The study will be a double-blind randomized controlled trial with two parallel groups of RA patients. Group A will be given 100 ml normal saline twice daily starting from 3 days before the operation, Group B will be given TXA 1.5 g twice daily starting from 3 days before the operation. All patients will be given TXA 1.5 g 30 min before the operation. The primary outcomes will be evaluated with total blood loss and hidden blood loss. Other outcome measurements such as, fibrinolysis parameters, inflammatory factors, visual analogue scale for post- operative pain, analgesia usage, coagulation parameters, transfusion, the length of stay (LOS), total hospitalization costs, the incidence of thromboembolic events and other complications will be recorded and compared. Recruitment is scheduled to begin on 1 August 2020, and the study will continue until 31 May 2021. Discussion: In current literature there is a lack of evidence with regard to the efficacy of TXA in RA patients. -

Role of the Renin–Angiotensin–Aldosterone and Kinin–Kallikrein Systems in the Cardiovascular Complications of COVID-19 and Long COVID
International Journal of Molecular Sciences Review Role of the Renin–Angiotensin–Aldosterone and Kinin–Kallikrein Systems in the Cardiovascular Complications of COVID-19 and Long COVID Samantha L. Cooper 1,2,*, Eleanor Boyle 3, Sophie R. Jefferson 3, Calum R. A. Heslop 3 , Pirathini Mohan 3, Gearry G. J. Mohanraj 3, Hamza A. Sidow 3, Rory C. P. Tan 3, Stephen J. Hill 1,2 and Jeanette Woolard 1,2,* 1 Division of Physiology, Pharmacology and Neuroscience, School of Life Sciences, University of Nottingham, Nottingham NG7 2UH, UK; [email protected] 2 Centre of Membrane Proteins and Receptors (COMPARE), School of Life Sciences, University of Nottingham, Nottingham NG7 2UH, UK 3 School of Medicine, Queen’s Medical Centre, University of Nottingham, Nottingham NG7 2UH, UK; [email protected] (E.B.); [email protected] (S.R.J.); [email protected] (C.R.A.H.); [email protected] (P.M.); [email protected] (G.G.J.M.); [email protected] (H.A.S.); [email protected] (R.C.P.T.) * Correspondence: [email protected] (S.L.C.); [email protected] (J.W.); Tel.: +44-115-82-30080 (S.L.C.); +44-115-82-31481 (J.W.) Abstract: Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is the virus responsible Citation: Cooper, S.L.; Boyle, E.; for the COVID-19 pandemic. Patients may present as asymptomatic or demonstrate mild to severe Jefferson, S.R.; Heslop, C.R.A.; and life-threatening symptoms. Although COVID-19 has a respiratory focus, there are major cardio- Mohan, P.; Mohanraj, G.G.J.; Sidow, vascular complications (CVCs) associated with infection. -

Low Molecular Weight Heparin Versus Acenocoumarol in the Secondary Prophylaxis of Deep Vein Thrombosis
Thromb Haemost 1999; 81: 26–31 © 1999 Schattauer Verlag, Stuttgart Low Molecular Weight Heparin versus Acenocoumarol in the Secondary Prophylaxis of Deep Vein Thrombosis S. Lopaciuk, H. Bielska-Falda1, W. Noszczyk1, M. Bielawiec 2, W. Witkiewicz 3, S. Filipecki 4, J. Michalak 5, L. Ciesielski 6, Z. Mackiewicz 7, E. Czestochowska 8, K. Zawilska 9, A. Cencora 10, among others* From the Institute of Hematology and Blood Transfusion, Warsaw, 1st 1Department of Surgery, Medical School, Warsaw, 2Department of Hematology, Medical School, Bialystok, 3Department of Vascular Surgery, District General Hospital, Wroclaw, 4Department of Internal Medicine, Institute of Tuberculosis and Lung Diseases, Warsaw, 5Department of Vascular Surgery, Medical School, Lublin, 1st 6Department of Surgery, Medical School, Lodz, 7Department of Vascular Surgery, Medical School, Bydgoszcz, 3rd 8Department of Internal Medicine, Medical School, Gdansk, 9Department of Hematology, Medical School, Poznan, and 10Department of Vascular Surgery, District General Hospital, Krakow, Poland Summary oral anticoagulant for at least 3 months (secondary prophylaxis). Al- though long-term anticoagulation with coumarin drugs, the most popu- The aim of this study was to determine the efficacy and safety of lar of which are warfarin and acenocoumarol, has been repeatedly dem- subcutaneous weight-adjusted dose low molecular weight heparin onstrated effective in the prevention of recurrent venous thromboembo- (LMWH) compared with oral anticoagulant (OA) in the prevention of lism, it suffers from a number of limitations. This treatment requires recurrent venous thromboembolism. In a prospective multicenter trial, strict laboratory control and consequent adjustments of the drug dosage 202 patients with symptomatic proximal deep vein thrombosis (DVT) and carries a substantial risk of bleeding complications (1). -
Occurrence, Elimination, and Risk of Anticoagulant Rodenticides in Wastewater and Sludge
Occurrence, elimination, and risk of anticoagulant rodenticides in wastewater and sludge Silvia Lacorte, Cristian Gómez- Canela Department of Environmental Chemistry, IDAEA-CSIC, Jordi Girona 18-26, 08034 Barcelona Rats and super-rats Neverending story 1967 Coumachlor 1 tn rodenticides /city per campaign “It will be the LAST ONE” Rodenticides Biocides: use regulated according to EU. Used mainly as bait formulations. First generation: multiple feedings, less persistent in tissues, commensal and outdoor use. Second generation: single feeding (more toxic), more persistent in tissue, commensal use only. Toxic: vitamin K antagonists that cause mortality by blocking an animal’s ability to produce several key blood clotting factors. High oral, dermal and inhalation toxicity. Origin and fate of rodenticides Study site: Catalonia (7.5 M inhabitants) 1693 km of sewage corridor 13 fluvial tanks (70.000 m3) 130,000,000 € / 8 YEARS 32,000 km2 378,742 kg/y AI 2,077,000 € Objectives 1. To develop an analytical method to determine most widely used rodenticides in wastewater and sludge. 2. To monitor the presence of rodenticides within 9 WWTP receiving urban and agricultural waters. 3. To evaluate the risk of rodenticides using Daphnia magna as aquatic toxicological model. 4. To study the accumulation of rodenticides in sludge. Compounds studied Coumachlor* Pindone C19H15ClO4 C14H14O3 Dicoumarol Warfarin C19H12O6 C19H16O4 Coumatetralyl Ferulenol FGARs C19H16O3 C24H30O3 Acenocoumarol Chlorophacinone • Solubility C19H15NO6 C23H15ClO3 0.001-128 mg/L • pKa 3.4-6.6 Flocoumafen Bromadiolone C H F O C H BrO 33 25 3 40 30 23 4 • Log P 1.92-8.5 Brodifacoum Fluindione C H BrO 31 23 3 C15H9FO2 SGARs Difenacoum Fenindione C31H24O3 C15H10O2 1. -

Role of Thrombin and Thromboxane A2 in Reocclusion Following Coronary
Proc. Natl. Acad. Sci. USA Vol. 86, pp. 7585-7589, October 1989 Medical Sciences Role of thrombin and thromboxane A2 in reocclusion following coronary thrombolysis with tissue-type plasminogen activator (thrombolytic therapy/coronary thrombosis/platelet activation/reperfusion) DESMOND J. FITZGERALD*I* AND GARRET A. FITZGERALD* Divisions of *Clinical Pharmacology and tCardiology, Vanderbilt University, Nashville, TN 37232 Communicated by Philip Needleman, June 28, 1989 (receivedfor review April 12, 1989) ABSTRACT Reocclusion of the coronary artery occurs against the prothrombinase formed on the platelet surface after thrombolytic therapy of acute myocardlal infarction (13) and the neutralization ofheparin by platelet factor 4 (14) despite routine use of the anticoagulant heparin. However, and thrombospondin (15), proteins released by activated heparin is inhibited by platelet activation, which is greatly platelets. enhanced in this setting. Consequently, it is unclear whether To address the role of thrombin during coronary throm- thrombin induces acute reocclusion. To address this possibility, bolysis, we have examined the effect of a specific thrombin we examined the effect of argatroban {MCI9038, (2R,4R)- inhibitor, argatroban {MCI9038, (2R,4R)-4-methyl-1-[N-(3- 4-methyl-l-[Na-(3-methyl-1,2,3,4-tetrahydro-8-quinolinesulfo- methyl-1,2,3,4-tetrahydro-8-quinolinesulfonyl)-L-arginyl]-2- nyl)-L-arginyl]-2-piperidinecarboxylic acid}, a specific throm- piperidinecarboxylic acid} on the response to tissue plasmin- bin inhibitor, on the response to tissue-type plasminogen ogen activator (t-PA) in a closed-chest canine model of activator in a dosed-chest canine model of coronary thrombo- coronary thrombosis. MCI9038, an argimine derivative which sis. MCI9038 prolonged the thrombin time and shortened the binds to a hydrophobic pocket close to the active site of time to reperfusion (28 + 2 min vs. -
STUDY PROTOCOL Study Information Title Apixaban Drug
Apixaban B0661076NON-INTERVENTIONAL STUDY PROTOCOL Final, 15-Feb-2016 NON-INTERVENTIONAL (NI) STUDY PROTOCOL Study information Title Apixaban drug utilization study in Stroke prevention in atrial fibrillation (SPAF) Protocol number B0661076 AEMPS Code PFI-API-2016-01 Protocol version identifier 4.0 Date of last version of protocol 15-Feb-2016 Active substance Apixaban B01AF02 Medicinal product Eliquis® Research question and objectives Evaluate the apixaban utilization according to the approved SPAF indication and recommendations by EMA. The study objectives are: Objective 1: To characterise patients using apixaban according to demographics, comorbidity, risk of thromboembolic events (CHADS2 and CHA2DS2-Vasc scores), risk of bleeding events (HAS-BLED score), comedications and compare it with the profile of patients treated with VKA, dabigatran and rivaroxaban. Objective 2: Describe the level of appropriate usage according to the posology recommended in the apixaban SmPC. Objective 3: Describe the potential interactions with other drugs prescribed concomitantly according with the SmPC recommendations. Objective 4: Estimate the level of apixaban adherence by the medication possession ratio (MPR) and discontinuation rates and compare it with VKA, dabigatran and CT24-GSOP-RF03 NI Study Protocol Template; Version 3.0, Effective Date 10-Oct-2014 Pfizer Confidential Page 1 of 28 Apixaban B0661076NON-INTERVENTIONAL STUDY PROTOCOL Final, 15-Feb-2016 rivaroxaban cohort. Objective 5: To analyze INR (International Normalized Ratio) values during the last 12 months and to obtain TTR (Time in Therapeutic Range) values in patients previously treated with VKA and, during the whole study period for those in the cohort treated with VKA Author Ángeles Quijada Manuitt, IDIAP Jordi Gol Rosa Morros Pedrós, IDIAP Jordi Gol Jordi Cortés, IDIAP Jordi Gol José Chaves Puertas, Pfizer SLU Sponsor Pfizer S.L.U Avda. -
FDA Approves ZONTIVITY™ (Vorapaxar), First-In-Class PAR-1
NEWS RELEASE FDA Approves ZONTIVITY™ (vorapaxar), First-in-Class PAR-1 Antagonist, for the Reduction of Thrombotic Cardiovascular Events in Patients with a History of Heart Attack or with Peripheral Arterial Disease 5/12/2014 ZONTIVITY Added to Standard of Care Demonstrated Long-Term Benet Through Three Years Merck (NYSE:MRK), known as MSD outside the United States and Canada, today announced that the U.S. Food and Drug Administration (FDA) has approved ZONTIVITY™ (vorapaxar) for the reduction of thrombotic cardiovascular events in patients with a history of heart attack (myocardial infarction) or in patients with narrowing of leg arteries, called peripheral arterial disease (PAD). For patients with a history of heart attack or with PAD who had no history of stroke or transient ischemic attack (TIA), ZONTIVITY added to standard of care produced a signicant 17 percent relative risk reduction over the three years of the study for the combined events of cardiovascular (CV) death, myocardial infarction (MI), stroke, and urgent coronary revascularization (UCR) [event rate 10.1 percent vs. 11.8 percent for placebo]. For the key secondary composite ecacy endpoint of CV death, MI and stroke alone, ZONTIVITY produced a signicant 20 percent relative risk reduction in these patients [7.9 percent vs. 9.5 percent for placebo]. These results were driven by an 18 percent relative risk reduction in MI [5.4 percent vs. 6.4 percent for placebo] and a 33 percent relative risk reduction in rst stroke [1.2 percent vs. 1.6 percent for placebo]. The prescribing information for ZONTIVITY includes a boxed warning regarding bleeding risk. -

New Zealand Data Sheet 1
New Zealand Data Sheet 1. PRODUCT NAME NAXEN® 250 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each NAXEN 250 mg tablet contains 250 mg of Naproxen For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM NAXEN 250 mg tablets are yellow, biconvex, round tablet of 11 mm diameter with one face engraved NX250 and having a bisecting score. The score line is only to facilitate breaking for ease of swallowing and not to divide into equal doses. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications NAXEN is indicated in adults for the relief of symptoms associated with rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, tendonitis and bursitis, acute gout and primary dysmenorrhoea. NAXEN is indicated in children for juvenile arthritis. 4.2. Dose and method of administration After assessing the risk/benefit ratio in each individual patient, the lowest effective dose for the shortest possible duration should be used (see Section 4.4). During long-term administration the dose of naproxen may be adjusted up or down depending on the clinical response of the patient. A lower daily dose may suffice for long-term administration. In patients who tolerate lower doses well, the dose may be increased to 1000 mg per day when a higher level of anti-inflammatory/analgesic 1 | P a g e activity is required. When treating patients with naproxen 1000 mg/day, the physician should observe sufficient increased clinical benefit to offset the potential increased risk. Dose Adults For rheumatoid arthritis, osteoarthritis and ankylosing spondylitis Initial therapy: The usual dose is 500-1000 mg per day taken in two doses at 12 hour intervals. -
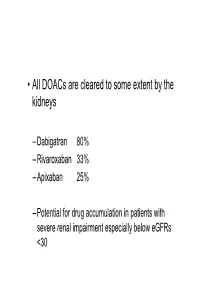
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -

Zontivity (Vorapaxar)
HIGHLIGHTS OF PRESCRIBING INFORMATION antiplatelet drugs or with ZONTIVITY as the only antiplatelet These highlights do not include all the information needed to use agent. (2.2) ZONTIVITY safely and effectively. See full prescribing information for ZONTIVITY. --------------------- DOSAGE FORMS AND STRENGTHS --------------------- Tablets: 2.08 mg vorapaxar. (3) ZONTIVITY™ (vorapaxar) Tablets 2.08 mg*, for oral use *Equivalent to 2.5 mg vorapaxar sulfate ------------------------------- CONTRAINDICATIONS ------------------------------- Initial U.S. Approval: 2014 History of stroke, TIA, or ICH. (4.1) Active pathologic bleeding. (4.2) WARNING: BLEEDING RISK See full prescribing information for complete boxed warning. ----------------------- WARNINGS AND PRECAUTIONS ----------------------- • Do not use ZONTIVITY in patients with a history of stroke, Like other antiplatelet agents, ZONTIVITY increases the risk of transient ischemic attack (TIA), or intracranial hemorrhage (ICH); bleeding. (5.1) or active pathological bleeding. (4.1, 4.2) Avoid use with strong CYP3A inhibitors or inducers. (5.2) • Antiplatelet agents, including ZONTIVITY, increase the risk of bleeding, including ICH and fatal bleeding. (5.1) ------------------------------ ADVERSE REACTIONS ------------------------------ Bleeding, including life-threatening and fatal bleeding, is the most ----------------------------INDICATIONS AND USAGE ---------------------------- commonly reported adverse reaction. (6.1) ZONTIVITY is a protease-activated receptor-1 (PAR-1) antagonist indicated for the reduction of thrombotic cardiovascular events in To report SUSPECTED ADVERSE REACTIONS, contact Merck patients with a history of myocardial infarction (MI) or with peripheral Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877 arterial disease (PAD). ZONTIVITY has been shown to reduce the rate 888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. of a combined endpoint of cardiovascular death, MI, stroke, and urgent coronary revascularization. -

Anticoagulant Effects of Statins and Their Clinical Implications
Review Article 1 Anticoagulant effects of statins and their clinical implications Anetta Undas1; Kathleen E. Brummel-Ziedins2; Kenneth G. Mann2 1Institute of Cardiology, Jagiellonian University School of Medicine, and John Paul II Hospital, Krakow, Poland; 2Department of Biochemistry, University of Vermont, Colchester, Vermont, USA Summary cleavage, factor V and factor XIII activation, as well as enhanced en- There is evidence indicating that statins (3-hydroxy-methylglutaryl dothelial thrombomodulin expression, resulting in increased protein C coenzyme A reductase inhibitors) may produce several cholesterol-inde- activation and factor Va inactivation. Observational studies and one ran- pendent antithrombotic effects. In this review, we provide an update on domized trial have shown reduced VTE risk in subjects receiving statins, the current understanding of the interactions between statins and blood although their findings still generate much controversy and suggest that coagulation and their potential relevance to the prevention of venous the most potent statin rosuvastatin exerts the largest effect. thromboembolism (VTE). Anticoagulant properties of statins reported in experimental and clinical studies involve decreased tissue factor ex- Keywords pression resulting in reduced thrombin generation and attenuation of Blood coagulation, statins, tissue factor, thrombin, venous throm- pro-coagulant reactions catalysed by thrombin, such as fibrinogen boembolism Correspondence to: Received: August 30, 2013 Anetta Undas, MD, PhD Accepted after major revision: October 15, 2013 Institute of Cardiology, Jagiellonian University School of Medicine Prepublished online: November 28, 2013 80 Pradnicka St., 31–202 Krakow, Poland doi:10.1160/TH13-08-0720 Tel.: +48 12 6143004, Fax: +48 12 4233900 Thromb Haemost 2014; 111: ■■■ E-mail: [email protected] Introduction Most of these additional statin-mediated actions reported are independent of blood cholesterol reduction.