Guidelines for ATC Classification and DDD Assignment 2013
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
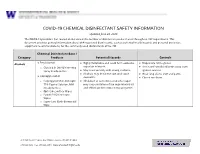
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Fosavance, INN-Alendronic Acid and Colecalciferol
EMA/175858/2015 EMEA/H/C/000619 EPAR summary for the public Fosavance alendronic acid and colecalciferol This is a summary of the European public assessment report (EPAR) for Fosavance. It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the medicine to reach its opinion in favour of granting a marketing authorisation and its recommendations on the conditions of use for Fosavance. What is Fosavance? Fosavance is a medicine that contains two active substances: alendronic acid and colecalciferol (vitamin D3). It is available as tablets (70 mg alendronic acid and 2,800 international units [IU] colecalciferol; 70 mg alendronic acid and 5,600 IU colecalciferol). What is Fosavance used for? Fosavance (containing either 2,800 or 5,600 IU colecalciferol) is used to treat osteoporosis (a disease that makes bones fragile) in women who have been through the menopause and are at risk of low vitamin D levels. Fosavance 70 mg/5,600 IU is for use in patients who are not taking vitamin D supplements. Fosavance reduces the risk of fractures (broken bones) in the spine and the hip. The medicine can only be obtained with a prescription. How is Fosavance used? The recommended dose of Fosavance is one tablet once a week. It is intended for long-term use. The patient must take the tablet with a full glass of water (but not mineral water), at least 30 minutes before any food, drink or other medicines (including antacids, calcium supplements and vitamins). To avoid irritation of the oesophagus (the tube that leads from the mouth to the stomach), the patient should not lie down until after their first food of the day, which should be at least 30 minutes after taking the tablet. -

WHO Drug Information Vol. 12, No. 3, 1998
WHO DRUG INFORMATION VOLUME 12 NUMBER 3 • 1998 RECOMMENDED INN LIST 40 INTERNATIONAL NONPROPRIETARY NAMES FOR PHARMACEUTICAL SUBSTANCES WORLD HEALTH ORGANIZATION • GENEVA Volume 12, Number 3, 1998 World Health Organization, Geneva WHO Drug Information Contents Seratrodast and hepatic dysfunction 146 Meloxicam safety similar to other NSAIDs 147 Proxibarbal withdrawn from the market 147 General Policy Issues Cholestin an unapproved drug 147 Vigabatrin and visual defects 147 Starting materials for pharmaceutical products: safety concerns 129 Glycerol contaminated with diethylene glycol 129 ATC/DDD Classification (final) 148 Pharmaceutical excipients: certificates of analysis and vendor qualification 130 ATC/DDD Classification Quality assurance and supply of starting (temporary) 150 materials 132 Implementation of vendor certification 134 Control and safe trade in starting materials Essential Drugs for pharmaceuticals: recommendations 134 WHO Model Formulary: Immunosuppressives, antineoplastics and drugs used in palliative care Reports on Individual Drugs Immunosuppresive drugs 153 Tamoxifen in the prevention and treatment Azathioprine 153 of breast cancer 136 Ciclosporin 154 Selective serotonin re-uptake inhibitors and Cytotoxic drugs 154 withdrawal reactions 136 Asparaginase 157 Triclabendazole and fascioliasis 138 Bleomycin 157 Calcium folinate 157 Chlormethine 158 Current Topics Cisplatin 158 Reverse transcriptase activity in vaccines 140 Cyclophosphamide 158 Consumer protection and herbal remedies 141 Cytarabine 159 Indiscriminate antibiotic -
AMIFOSTINE for INJECTION Incidence of Grade 2 Or Higher Xerostomia (RTOG Criteria)
TABLE 4 AMIFOSTINE FOR INJECTION Incidence of Grade 2 or Higher Xerostomia (RTOG criteria) Amifostine for RT p-value only Injection +RT LBL-7062PD Acute DESCRIPTION 51% (75/148) 78% (120/153) p<0.0001 ( 90 days from Amifostine for Injection is an organic thiophosphate cytoprotective agent known chemically ɖ start of radiation) as 2-[(3-aminopropyl)amino]ethanethiol dihydrogen phosphate (ester) and has the following structural formula: Latea 35% (36/103) 57% (63/111) p=0.0016 (9-12 months H2N(CH2)3NH(CH2)2S-PO3H2 post radiation) Amifostine is a white crystalline powder which is freely soluble in water. Its empirical aBased on the number of patients for whom actual data were available. formula is C5H15N2O3PS and it has a molecular weight of 214.22. Amifostine for Injection is the trihydrate form of amifostine and is supplied as a sterile At one year following radiation, whole saliva collection following radiation showed that lyophilized powder requiring reconstitution for intravenous infusion. Each single-use 10 mL more patients given Amifostine for Injection produced >0.1 gm of saliva (72% vs. 49%). vial contains 500 mg of amifostine on the anhydrous basis. In addition, the median saliva production at one year was higher in those patients who CLINICAL PHARMACOLOGY received amifostine (0.26 gm vs. 0.1 gm). Stimulated saliva collections did not show Amifostine is a prodrug that is dephosphorylated by alkaline phosphatase in tissues to a a difference between treatment arms. These improvements in saliva production were pharmacologically active free thiol metabolite. This metabolite is believed to be responsible supported by the patients’ subjective responses to a questionnaire regarding oral dryness. -

Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep
animals Article Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep Shashwati Mathurkar 1,*, Preet Singh 2 ID , Kavitha Kongara 2 and Paul Chambers 2 1 1B, He Awa Crescent, Waikanae 5036, New Zealand 2 School of Veterinary Sciences, College of Sciences, Massey University, Palmerston North 4474, New Zealand; [email protected] (P.S.); [email protected] (K.K.); [email protected] (P.C.) * Correspondence: [email protected]; Tel.: +64-221-678-035 Received: 13 June 2018; Accepted: 16 July 2018; Published: 18 July 2018 Simple Summary: Scarcity of non-steroidal anti-inflammatory drugs (NSAID) to minimise the pain in sheep instigated the current study. The aim of this study was to know the pharmacokinetic parameters of salicylic acid in New Zealand sheep after administration of multiple intravenous and oral doses of sodium salicylate (sodium salt of salicylic acid). Results of the study suggest that the half-life of the drug was shorter and clearance was faster after intravenous administration as compared to that of the oral administration. The minimum effective concentration required to produce analgesia in humans (16.8 µL) was achieved in sheep for about 0.17 h in the current study after intravenous administration of 100 and 200 mg/kg body weight of sodium salicylate. However, oral administration of these doses failed to achieve the minimum effective concentration as mentioned above. This study is of significance as it adds valuable information on pharmacokinetics and its variation due to breed, species, age, gender and environmental conditions. -

Valturna Label
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------WARNINGS AND PRECAUTIONS---------------- These highlights do not include all the information needed to use • Avoid fetal or neonatal exposure. (5.1) Valturna safely and effectively. See full prescribing information for • Head and neck angioedema: Discontinue Valturna and monitor until Valturna. signs and symptoms resolve. (5.2) • Hypotension in volume- or salt-depleted Patients: Correct imbalances Valturna (aliskiren and valsartan, USP) Tablets before initiating therapy with Valturna. (5.3) Initial U.S. Approval: 2009 • Patients with renal impairment: Decreases in renal function may be anticipated in susceptible individuals. (5.4) WARNING: AVOID USE IN PREGNANCY • Patients with hepatic impairment: Slower clearance may occur. (5.5) See full prescribing information for complete boxed warning. • Hyperkalemia: Consider periodic determinations of serum electrolytes to When pregnancy is detected, discontinue Valturna as soon as possible. detect possible electrolyte imbalances, particularly in patients at risk. When used in pregnancy during the second and third trimester, drugs (5.7) that act directly on the renin-angiotensin system can cause injury and death to the developing fetus. (5.1) --------------------------------ADVERSE REACTIONS----------------------- The most common adverse events (incidence ≥1.5% and more common than ---------------------------INDICATIONS AND USAGE----------------------- with placebo) are: fatigue and nasopharyngitis. (6.1) Valturna is a combination of aliskiren, a direct renin inhibitor, and valsartan, an angiotensin II receptor blocker (ARB), indicated for the treatment of To report SUSPECTED ADVERSE REACTIONS, contact Novartis hypertension: Pharmaceuticals Corporation at 1-888-669-6682 or FDA at • In patients not adequately controlled with monotherapy. (1) 1-800-FDA-1088 or www.fda.gov/medwatch • May be substituted for titrated components. -

Adrovance, INN-Alendronic Acid
EMA/194587/2011 EMEA/H/C/000759 EPAR summary for the public Adrovance alendronic acid / colecalciferol This is a summary of the European public assessment report (EPAR) for Adrovance. It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the medicine to reach its opinion in favour of granting a marketing authorisation and its recommendations on the conditions of use for Adrovance. What is Adrovance? Adrovance is a medicine that contains two active substances: alendronic acid and colecalciferol (vitamin D3). It is available as white tablets (capsule-shaped: 70 mg alendronic acid and 2,800 international units [IU] colecalciferol; rectangular: 70 mg alendronic acid and 5,600 IU colecalciferol). What is Adrovance used for? Adrovance (containing either 2,800 or 5,600 IU colecalciferol) is used to treat osteoporosis (a disease that makes bones fragile) in women who have been through the menopause and are at risk of low vitamin D levels. Adrovance 70 mg/5,600 IU is for use in patients who are not taking vitamin D supplements. Adrovance reduces the risk of broken bones in the spine and the hip. The medicine can only be obtained with a prescription. How is Adrovance used? The recommended dose of Adrovance is one tablet once a week. It is intended for long-term use. The patient must take the tablet with a full glass of water (but not mineral water), at least 30 minutes before any food, drink or other medicines (including antacids, calcium supplements and vitamins). To avoid irritation of the oesophagus (gullet), the patient should not lie down until after their first food of the day, which should be at least 30 minutes after taking the tablet. -

Advances in Immunosuppression for Renal Transplantation Antoine Durrbach, Helene Francois, Severine Beaudreuil, Antoine Jacquet and Bernard Charpentier
REVIEWS Advances in immunosuppression for renal transplantation Antoine Durrbach, Helene Francois, Severine Beaudreuil, Antoine Jacquet and Bernard Charpentier Abstract | The development of immunosuppressants with minimal adverse and nephrotoxic effects is important to improve outcomes, such as acute and chronic antibody-mediated rejection, after organ transplantation. In addition, the application of expanded criteria for donors and transplantation in immunized patients necessitates the development of new therapies. Drug development over the past 10 years has generally been disappointing, but several new promising compounds have been or are being developed to prevent acute and chronic transplant rejection. In this Review, we report on several compounds that have been developed to remove allogenic T cells and/or to inhibit T-cell activation. We also discuss compounds that interfere with antibody-mediated rejection. Durrbach, A. et al. Nat. Rev. Nephrol. 6, 160–167 (2010); published online 2 February 2010; doi:10.1038/nrneph.2009.233 Introduction Renal transplantation has specific features that make or as a result of previous transplantation, has increased it different from transplantation procedures for other over the past decade. In addition, ABOincompatible organs. For example, outcomes can be affected by grafts are becoming more frequently used. Together, these common states, such as donor and/or recipient age, high factors have led to a rise in the number of ‘immuno logically blood pressure, diabetes mellitus, metabolic disturbances atrisk’ kidney transplantations. Few immunosuppressants (such as high LDL cholesterol) and abnormalities in fluid targeted to B cells have, however, been available to control and electrolyte balance. The kidney is also very sensitive the antibodymediated response. -

Patient Information Telmisartan (TEL-Mi-SAR-Tan) Tablets, USP
Patient Information Telmisartan (TEL-mi-SAR-tan) Tablets, USP Read this Patient Information before you start taking telmisartan tablets and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment. What is the most important information I should know about telmisartan tablets? Telmisartan tablets can cause harm or death to an unborn baby. Talk to your doctor about other ways to lower your blood pressure if you plan to become pregnant. If you get pregnant while taking telmisartan tablets, tell your doctor right away. What are telmisartan tablets? Telmisartan tablets are a prescription medicine used: • to treat high blood pressure (hypertension) It is not known if telmisartan tablets are safe and effective in children. Who should not take telmisartan tablets? You should not take telmisartan tablets if you are allergic (hypersensitive) to the active ingredient (telmisartan) or any of the other ingredients listed at the end of this leaflet. For patients with diabetes, if you are taking telmisartan tablets you should not take aliskiren. What should I tell my doctor before taking telmisartan tablets? Before you take telmisartan tablets, tell your doctor if you: • are pregnant or are planning to become pregnant. See “What is the most important information I should know about telmisartan tablets?” • are breast-feeding or plan to breast-feed. It is not known if telmisartan passes into your breast milk. You and your doctor should decide if you will take telmisartan tablets or breast-feed. You should not do both. -

Biologic Armamentarium in Psoriasis
Vol 9, Issue 1, 2016 ISSN - 0974-2441 Review Article BIOLOGIC ARMAMENTARIUM IN PSORIASIS GANESH PAI1*, NITHIN SASHIDHARAN2 1Medical Director, Derma-Care ‘The Trade Centre’, Mangalore - 575 003, Karnataka, India. 2Consultant Clinical Pharmacologist, Derma-Care ‘The Trade Centre’, Mangalore - 575 003, Karnataka, India. Email: [email protected] Received: 14 July 2015, Revised and Accepted: 24 August 2015 ABSTRACT Psoriasis is an autoimmune disease and further classed as a chronic inflammatory skin condition serving as a global burden. A moderate to severe psoriasis can be treated with conventional therapies. Less efficacy, poor patient compliance, and toxicity issues were the major problems associated with conventional therapies. The introduction of biologic therapy has a great impression on psoriatic treatment duration and enhanced quality of life in psoriasis patients. The new biologic therapies are tailor-made medications with the goal of more specific and effective treatment; less toxicity. The biologic therapy is aimed to target antigen presentation and co-stimulation, T-cell activation, and leukocyte adhesion; and pro-inflammatory cascade. They act as effective and safer substitute to traditional therapy. Secukinumab, certolizumab, itolizumab, golimumab, ustekinumab, adalimumab, infliximab etanercept, alefacept, etc. are the approved biologic with the global market. This review briefs about psoriasis pathogenesis, traditional treatments, and biologic therapies potential. Keywords: Psoriasis, Biologic, Non-biologic treatment. INTRODUCTION migration, potentiation of Th1 type of response, angiogenesis, and epidermal hyperplasia [7]. Psoriasis is an autoimmune disease and further classed as a chronic inflammatory skin condition with prevalence ranging 1-3% in the TNF- is plays vital role in the pathogenesis of psoriasis. It acts by world [1]. -

The Comparison of the Effect Between Alginate-Based Raft-Forming Liquid and Alginate Liquid on Gastroesophageal Reflux Disease and Gastric Ulcer in Rats
Online - 2455-3891 Vol 10, Issue 12, 2017 Print - 0974-2441 Research Article THE COMPARISON OF THE EFFECT BETWEEN ALGINATE-BASED RAFT-FORMING LIQUID AND ALGINATE LIQUID ON GASTROESOPHAGEAL REFLUX DISEASE AND GASTRIC ULCER IN RATS HAKIM BANGUN1*, ANAYANTI ARIANTO1, RIRIN ASTYA1, GONTAR A SIREGAR2 1Department of Pharmaceutical Technology, Faculty of Pharmacy, Nanomedicine Center, University of Sumatera Utara, Jl. Tri Dharma No. 5, Kampus USU, Medan, Indonesia. 2Department of Internal Medicine, Faculty of Medicine, University of Sumatera Utara, Jl Dr. T. Mansyur No. 5, Kampus USU, Medan, Indonesia. Email: [email protected] Received: 04 July 2017, Revised and Accepted: 16 August 2017 ABSTRACT Objective: The objective of the study was to compare the effect between alginate (Alg)-based raft-forming and Alg liquid on healing gastroesophageal reflux disease (GERD) and gastric ulcer in rats. Methods: Each of the 18 fasted rats was given 1 ml acidified pepsin. Then, rats were divided into three groups. Each group consisted of six rats. Group 1 (negative control) was orally given 1 ml distilled water, Group 2 was given 1 ml Alg-based raft-forming liquid, and Group 3 was given 1 ml Alg liquid. Then, the abdomen of rats was incised under anesthesia with ketamine, and then both their pylorus and the forestomach were ligated to form gastric reflux. After 4 hrs, all rats were killed with chloroform and their esophagus and stomach were examined macroscopically and microscopically (histopathology). Results: On macroscopic observation, all of the Group 1 rats (negative control) showed esophageal lesions and gastric lesions. Four rats of Group 2 (given Alg-based raft-forming) showed no esophageal lesion and two more rats showed a slight lesion, but all of the tested rats showed gastric lesions. -

RAFT FORMING SYSTEM a REVIEW Bhavsar Dhaval Niranjanbhai*, Varde Neha Mahendrakumar, C
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Journal of Drug Delivery and Therapeutics (JDDT) Bhavsar et al Journal of Drug Delivery & Therapeutics; 2012, 2(5), 123-128 123 Available online at http://jddtonline.info REVIEW ARTICLE ADVANCES IN GRDDS: RAFT FORMING SYSTEM A REVIEW Bhavsar Dhaval Niranjanbhai*, Varde Neha Mahendrakumar, C. Sini Surendran, Shah Viral H, Upadhyay UM Dept. of pharmaceutics, Sigma Institute of Pharmacy, Bakrol, Vadodara(Gujarat), India *Corresponding Author’s Ph: +91-9725512814, Email id: [email protected] Received 06 June 2012; Review Completed 26 Aug 2012; Accepted 26 Aug 2012, Available online 15 Sep 2012 ABSTRACT: In recent years several advancements has been made in research and development of Gastro retentive drug delivery system to overcome the drawback of non-site specificity when drug administered orally. In order to understand various physiological difficulties to achieve gastric retention, we have summarized important factors controlling gastric retention time. We have reviewed various gastro retentive approaches designed and developed until now i.e. floating drug dosage systems (FDDS), swelling or expanding systems, mucoadhesive systems, high density system, Raft forming system, magnetic systems. Among these systems, the review summarizes the special focus on raft forming approach which comes under floating drug delivery system. Raft system incorporates alginate gels which have carbonate components react with gastric acid causes bubbles and this enables floating. Finally, Evaluation, advantages, disadvantages, future potential and marketed preparation of raft forming approach in gastro retentive drug delivery systems were covered. Key words-Advances in GRDDS, Raft forming system, alginic acid, gaviscon, INTRODUCTION: Conventional oral delivery is widely used in 4) Drugs with a narrow window of absorption E.g.