What Can We Learn from the 1918 Pandemic? Careful Economics and Policy Lessons from Influenza
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fitzgerald in the Late 1910S: War and Women Richard M
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Duquesne University: Digital Commons Duquesne University Duquesne Scholarship Collection Electronic Theses and Dissertations 2009 Fitzgerald in the Late 1910s: War and Women Richard M. Clark Follow this and additional works at: https://dsc.duq.edu/etd Recommended Citation Clark, R. (2009). Fitzgerald in the Late 1910s: War and Women (Doctoral dissertation, Duquesne University). Retrieved from https://dsc.duq.edu/etd/416 This Immediate Access is brought to you for free and open access by Duquesne Scholarship Collection. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Duquesne Scholarship Collection. For more information, please contact [email protected]. FITZGERALD IN THE LATE 1910s: WAR AND WOMEN A Dissertation Submitted to the McAnulty College and Graduate School Duquesne University In partial fulfillment of the requirements for the degree of Doctor of Philosophy By Richard M. Clark August 2009 Copyright by Richard M. Clark 2009 FITZGERALD IN THE LATE 1910s: WAR AND WOMEN By Richard M. Clark Approved July 21, 2009 ________________________________ ________________________________ Linda Kinnahan, Ph.D. Greg Barnhisel, Ph.D. Professor of English Assistant Professor of English (Dissertation Director) (2nd Reader) ________________________________ ________________________________ Frederick Newberry, Ph.D. Magali Cornier Michael, Ph.D. Professor of English Professor of English (1st Reader) (Chair, Department of English) ________________________________ Christopher M. Duncan, Ph.D. Dean, McAnulty College and Graduate School of Liberal Arts iii ABSTRACT FITZGERALD IN THE LATE 1910s: WAR AND WOMEN By Richard M. Clark August 2009 Dissertation supervised by Professor Linda Kinnahan This dissertation analyzes historical and cultural factors that influenced F. -

A Life Transformed: the 1910S
TWO A Life Transformed: The 1910s Not the least significant element of modem political history is contained in the constant growth of individual personality accompanied by the limitation of the State.! Georg Jellinek, 1892 FIRST TRIP TO CHINA AND THE JAPANESE COMMUNITY IN PEKING When Nakae grew bored with working for the South Manchurian Rail way Company, once again his benefactors came to his rescue and found something else for him. Around October 1914, his mother's former boarder, Ts'ao Ju-lin, managed to land him an offer. Ts'ao summoned Nakae to Peking with a one-year contract to work as secretary to Ariga Nagao (1860-1921). Ariga was a professor of international law at Waseda University and had been a friend of Ushikichi's father, although thei; political views diverged sharply. Apparently, years before, Mrs. Nakae out of concern for her wayward son's future had prevailed on the ever grateful Ts'ao to intercede on behalf of Ushikichi if necessary. Nakae received the handsome monthly salary of one hundred yuan for responsibilities neither especially demanding nor explicit. One suspects that he held this sinecure, which might otherwise not have existed, because of his mother's earlier appeal. We know, however, that Nakae spent a great deal of his time in China that year leading what he himself would later refer to as the life of a "profligate villain" (hi5ti5 burai).2 In 1914 Ariga accepted an invitation to serve as an advisor to the gov- "'-------------------- -- 28 A Life Transformed ernment of Yuan Shih-k'ai (1859-1916), which had taken power several years earlier in the young Republic of China. -

American Armies and Battlefields in Europe
Chapter v1 THE AMERICAN BATTLEFIELDS NORTH OF PARIS chapter gives brief accounts of areas and to all of the American ceme- all American fighting whi ch oc- teries and monuments. This route is Thiscurred on the battle front north of recommended for those who desire to Paris and complete information concern- make an extended automobile tour in the ing the American military cemeteries and region. Starting from Paris, it can be monuments in that general region. The completely covered in four days, allowing military operations which are treated are plenty of time to stop on the way. those of the American lst, 27th, 30th, The accounts of the different operations 33d, 37th, 80th and 91st Divisions and and the descriptions of the American the 6th and 11 th Engineer Regiments. cemeteries and monuments are given in Because of the great distances apart of the order they are reached when following So uthern Encr ance to cb e St. Quentin Can al Tunnel, Near Bellicourc, October 1, 1918 the areas where this fighting occurred no the suggested route. For tbis reason they itinerary is given. Every operation is do not appear in chronological order. described, however, by a brief account Many American units otber tban those illustrated by a sketch. The account and mentioned in this chapter, sucb as avia- sketch together give sufficient information tion, tank, medical, engineer and infantry, to enable the tourist to plan a trip through served behind this part of the front. Their any particular American combat area. services have not been recorded, however, The general map on the next page as the space limitations of tbis chapter indicates a route wbich takes the tourist required that it be limited to those Amer- either int o or cl ose to all of tbese combat ican organizations which actually engaged (371) 372 THE AMERICAN B ATTLEFIELD S NO R TH O F PARIS Suggested Tour of American Battlefields North of Paris __ Miles Ghent ( î 37th and 91st Divisions, Ypres-Lys '"offensive, October 30-November 11, 1918 \ ( N \ 1 80th Division, Somme 1918 Albert 33d Division. -

Jazz and the Cultural Transformation of America in the 1920S
Louisiana State University LSU Digital Commons LSU Doctoral Dissertations Graduate School 2003 Jazz and the cultural transformation of America in the 1920s Courtney Patterson Carney Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_dissertations Part of the History Commons Recommended Citation Carney, Courtney Patterson, "Jazz and the cultural transformation of America in the 1920s" (2003). LSU Doctoral Dissertations. 176. https://digitalcommons.lsu.edu/gradschool_dissertations/176 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Doctoral Dissertations by an authorized graduate school editor of LSU Digital Commons. For more information, please [email protected]. JAZZ AND THE CULTURAL TRANSFORMATION OF AMERICA IN THE 1920S A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Doctor of Philosophy in The Department of History by Courtney Patterson Carney B.A., Baylor University, 1996 M.A., Louisiana State University, 1998 December 2003 For Big ii ACKNOWLEDGEMENTS The real truth about it is no one gets it right The real truth about it is we’re all supposed to try1 Over the course of the last few years I have been in contact with a long list of people, many of whom have had some impact on this dissertation. At the University of Chicago, Deborah Gillaspie and Ray Gadke helped immensely by guiding me through the Chicago Jazz Archive. -

THE WRITINGS of BRITISH CONSCRIPT SOLDIERS, 1916-1918 Ilana Ruth Bet-El Submitted for the Degree of Ph
EXPERIENCE INTO IDENTITY: THE WRITINGS OF BRITISH CONSCRIPT SOLDIERS, 1916-1918 Ilana Ruth Bet-El Submitted for the degree of PhD University College London AB STRACT Between January 1916 and March 1919 2,504,183 men were conscripted into the British army -- representing as such over half the wartime enlistments. Yet to date, the conscripts and their contribution to the Great War have not been acknowledged or studied. This is mainly due to the image of the war in England, which is focused upon the heroic plight of the volunteer soldiers on the Western Front. Historiography, literary studies and popular culture all evoke this image, which is based largely upon the volumes of poems and memoirs written by young volunteer officers, of middle and upper class background, such as Wilfred Owen and Siegfried Sassoon. But the British wartime army was not a society of poets and authors who knew how to distil experience into words; nor, as mentioned, were all the soldiers volunteers. This dissertation therefore attempts to explore the cultural identity of this unknown population through a collection of diaries, letters and unpublished accounts of some conscripts; and to do so with the aid of a novel methodological approach. In Part I the concept of this research is explained, as a qualitative examination of all the chosen writings, with emphasis upon eliciting the attitudes of the writers to the factual events they recount. Each text -- e.g. letter or diary -- was read literally, and also in light of the entire collection, thus allowing for the emergence of personal and collective narratives concurrently. -
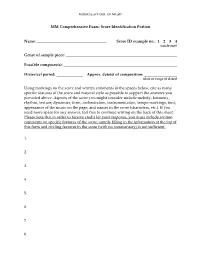
MM Comprehensive Exam: Score Identification Portion Name
MOORES SCHOOL OF MUSIC MM Comprehensive Exam: Score Identification Portion Name: Score ID example no.: 1 2 3 4 (circle one) Genre of sample piece: Possible composer(s): Historical period: Approx. date(s) of composition: (date or range of dates) Using markings on the score and written comments in the spaces below, cite as many specific features of the score and musical style as possible to support the answers you provided above. Aspects of the score you might consider include melody, harmony, rhythm, texture, dynamics, form, orchestration, instrumentation, tempo markings, font, appearance of the music on the page, and names in the score (characters, etc.). If you need more space for any answer, feel free to continue writing on the back of this sheet. Please note that in order to receive credit for your response, you must include written comments on specific features of the score; simply filling in the information at the top of this form and circling features in the score (with no commentary) is not sufficient. 1. 2. 3. 4. 5. 6. 7. 8. Andrew Davis. rev. Nov 2009. General information on preparing for a comprehensive exam in music (geared especially toward answering questions in music theory and/or discussing unidentified scores): Comprehensive exams (especially music theory portions, and to some extent score identification portions, if applicable) ask you to focus on broad theoretical and/or stylistic topics that you're expected to know as a literate musician with a graduate degree in music. For example, in the course of the exam you might -

The U.S., World War I, and Spreading Influenza in 1918
Online Office Hours We’ll get started at 2 ET Library of Congress Online Office Hours Welcome. We’re glad you’re here! Use the chat box to introduce yourselves. Let us know: Your first name Where you’re joining us from Why you’re here THE U.S., WORLD WAR I, AND SPREADING INFLUENZA IN 1918 Ryan Reft, historian of modern America in the Manuscript Division at the Library of Congress Using LoC collections to research influenza pandemic 1918-1919 Woodrow Wilson, draft Fourteen Three main takeaways Points, 1918 • Demonstrate the way World War I facilitated the spread of the virus through mobilization • How the pandemic was fought domestically and its effects • Influenza’s possible impact on world events via Woodrow Wilson and the Treaty of Versailles U.S. in January 1918 Mobilization Military Map of the [USA], 1917 • Creating a military • Selective Service Act passed in May 1917 • First truly conscripted military in U.S. history • Creates military of four million; two million go overseas • Military camps set up across nation • Home front oriented to wartime production of goods • January 1918 Woodrow Wilson outlines his 14 points Straight Outta Kansas Camp Funston Camp Funston, Fort Riley, 1918 • First reported case of influenza in Haskell County, KS, February 1918 • Camp Funston (Fort Riley), second largest cantonment • 56,000 troops • Virus erupts there in March • Cold conditions, overcrowded tents, poorly heated, inadequate clothing The first of three waves • First wave, February – May, 1918 • Even if there was war … • “high morbidity, but low mortality” – Anthony Fauci, 2018 the war was removed • Americans carry over to Europe where it changes from us you know … on • Second wave, August – December the other side … This • Most lethal, high mortality esp. -

State Gun Laws, Gun Ownership, and Mass Shootings in the US: Cross Sectional Time Series BMJ: First Published As 10.1136/Bmj.L542 on 6 March 2019
RESEARCH State gun laws, gun ownership, and mass shootings in the US: BMJ: first published as 10.1136/bmj.l542 on 6 March 2019. Downloaded from cross sectional time series Paul M Reeping,1 Magdalena Cerdá,2 Bindu Kalesan,3 Douglas J Wiebe,4 Sandro Galea,5 Charles C Branas1 1Department of Epidemiology, ABSTRACT a growing divide appears to be emerging between Columbia University, Mailman OBJECTIVE restrictive and permissive states. School of Public Health, 722 To determine whether restrictiveness-permissiveness West 168th Street, New York, of state gun laws or gun ownership are associated NY 10032, USA Introduction 2 with mass shootings in the US. Department of Population Despite an increasing frequency of mass shootings in Health, New York University, DESIGN Langone School of Medicine, the US and the seemingly disproportionate occurrence New York, NY, USA Cross sectional time series. of mass shootings in some states and not others, little 3Department of Community SETTING AND POPULATION research has been carried out to understand state level Health Sciences, Boston US gun owners from 1998-2015. factors that could influence mass shootings.1 A 2018 University School of Public Health, Boston, MA, USA EXPOSURE report pointed to only three studies that had examined 4Department of Biostatistics, An annual rating between 0 (completely restrictive) associations between gun laws and mass shooting Epidemiology & Informatics, and 100 (completely permissive) for the gun laws events.2-5 However, testing the effects of state gun University of Pennsylvania, of all 50 states taken from a reference guide for laws on the occurrence of mass shootings was not the Perelman School of Medicine, Philadelphia, PA, USA gun owners traveling between states from 1998 to primary objective of at least one of these studies and 5Boston University School of 2015. -

The War and Fashion
F a s h i o n , S o c i e t y , a n d t h e First World War i ii Fashion, Society, and the First World War International Perspectives E d i t e d b y M a u d e B a s s - K r u e g e r , H a y l e y E d w a r d s - D u j a r d i n , a n d S o p h i e K u r k d j i a n iii BLOOMSBURY VISUAL ARTS Bloomsbury Publishing Plc 50 Bedford Square, London, WC1B 3DP, UK 1385 Broadway, New York, NY 10018, USA 29 Earlsfort Terrace, Dublin 2, Ireland BLOOMSBURY, BLOOMSBURY VISUAL ARTS and the Diana logo are trademarks of Bloomsbury Publishing Plc First published in Great Britain 2021 Selection, editorial matter, Introduction © Maude Bass-Krueger, Hayley Edwards-Dujardin, and Sophie Kurkdjian, 2021 Individual chapters © their Authors, 2021 Maude Bass-Krueger, Hayley Edwards-Dujardin, and Sophie Kurkdjian have asserted their right under the Copyright, Designs and Patents Act, 1988, to be identifi ed as Editors of this work. For legal purposes the Acknowledgments on p. xiii constitute an extension of this copyright page. Cover design by Adriana Brioso Cover image: Two women wearing a Poiret military coat, c.1915. Postcard from authors’ personal collection. This work is published subject to a Creative Commons Attribution Non-commercial No Derivatives Licence. You may share this work for non-commercial purposes only, provided you give attribution to the copyright holder and the publisher Bloomsbury Publishing Plc does not have any control over, or responsibility for, any third- party websites referred to or in this book. -

COVID-19 and HIV: 1 MOMENT 2 EPIDEMICS 3 OPPORTUNITIES How to Seize the Moment to Learn, Leverage and Build a New Way Forward for Everyone’S Health and Rights
UNAIDS | 2020 COVID-19 AND HIV: 1 MOMENT 2 EPIDEMICS 3 OPPORTUNITIES How to seize the moment to learn, leverage and build a new way forward for everyone’s health and rights Contents 2 Foreword 3 Key messages 4 Introduction 6 Learning from the HIV response to effectively address COVID-19 14 Leveraging the HIV infrastructure to strengthen, accelerate and sustain responses to COVID-19 19 Reimagining systems for health 25 Key recommendations for the COVID-19 response 27 References Foreword The COVID-19 pandemic has exposed the inadequacy of investments in public health, the persistence of profound economic and social inequalities and the fragility of many key global systems and approaches. Given the epic dimensions of the emergency, the world needs unity and solidarity—led by a large-scale, coordinated and comprehensive health response, and a focus on the needs of developing countries. Our decades-long fight against HIV offers essential lessons. This new report by UNAIDS examines how the experience of tackling HIV can help inform and guide effective, efficient, people-centred and sustainable COVID-19 responses. In fighting HIV, the world was confronted with a new, serious and multifaceted health crisis. Successful international efforts were rooted in a focus on innovation, respect for human rights and gender equality, community-based solutions and a commitment to leave no one behind. Decades of investment in the HIV response have created platforms that are proving useful in battling COVID-19—just as they were in responding to the 2014–2015 Ebola outbreak in western and central Africa. By being smart and strategic, we can leverage the HIV infrastructure to accelerate COVID-19 responses. -

Recent Publications Relating to Military Meteorology
40 MONTHLY WEATHER REVIEW. JANUARY,1918 Seeod Pan Amhnseientifi eongrees-continued. U. S. States relations service. Experiment station rmd. Wiwhington. Kullmer, C. J. Monthly storm frequency in the United States. v. $7. Noiyenibcr. 1917. 338-393. Richards, E. E. Dissolved oxygen in rain water. p. 6W21. 2ud, Robert DeC[ourcy]. The thunderstorms of the United [Abstract from Jour. agr. sci.] Statea as climatic phenomena. p. 393-411. Adniie des sciences. C‘omptea rendus. Pm.8. Tome 165. 24 dkm- Huntington, Ellsworth. Solar activity, cyclonic storms, and cli- bre 1917. matic changes. 411-431. Schaffers, V. Le son du canon h grande distance. p. 1057 1058. Cox, HeyI. Iniuence of the Great Lakes upon movement of Dunoyer L. & Reboul, G. Sur les variations diurnee du vent en hqh an ow pressure areas. p. 432-459. altitude. p. 1068-1071. Fassrg, Oliver L. Tropical rains-their duration, frequency, and Acadhnie de8 skes. Compte8 rendus. Pa&. Tonit 166. 21 jan&r intensity. 9. 4-73. 191s. Gab, htonio. Fluctuacionea climatol6gicas en loa tiempos Reboul, G. Relation entre lea variations barornhtriquea et cellea hidricos. 475481. du vent au sol: application la pr6vision. p. 124-126. Cline, Isaac Bf: Temperature conditions at New Orleans, 8.- in- Bureau ~nteniatwnalde8 poide et inesure8. !haaux et 7nkmches. Pa&. fluenced by subsurface drainage. p. 461-496. Tome 16. 1917. Church, J[ames] E., Jr. Snow eurveymg: ita blems and their Leduc, A. La maaae du litre d’air dana lee conditions normalea. present phasea with reference to Mount gel Nevada, and p: 7-37. [Introductory note b Ch. Ed. -

The Impact of the 1918-1919 Influenza Epidemic on Virginia Stephanie Forrest Barker
University of Richmond UR Scholarship Repository Master's Theses Student Research 2002 The impact of the 1918-1919 influenza epidemic on Virginia Stephanie Forrest Barker Follow this and additional works at: http://scholarship.richmond.edu/masters-theses Part of the History Commons Recommended Citation Barker, Stephanie Forrest, "The impact of the 1918-1919 influenza epidemic on Virginia" (2002). Master's Theses. Paper 1169. This Thesis is brought to you for free and open access by the Student Research at UR Scholarship Repository. It has been accepted for inclusion in Master's Theses by an authorized administrator of UR Scholarship Repository. For more information, please contact [email protected]. The Impact of the 1918-1919 Influenza Epidemic on Virginia By Stephanie Forrest Barker Master of Arts in History, University of Richmond, 2002 R. Barry Westin, Thesis Director In the fall of 1918 an unparalleled influenza pandemic spread throughout the world. More than a quarter of Americans became ill, and at least 600,000 died. For many Virginians, this was a time of acute crisis that only could be compared to the days of the Civil War. This thesis describes Spanish influenza's impact on Virginia, primarily focusing on the cities of Newport News, Richmond, and Roanoke. It details influenza's emergence in Virginia and explores how state and city officials dealt with this unprecedented epidemic. This study examines how the epidemic disrupted daily routines of life and overwhelmed the state's medical community. This thesis briefly discusses the effect that the segregation of races had on the spread of influenza and the role that women played in battling the epidemic.