MDS Foundation Spring 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hen the Streams Overflow
--",41000,-**-% 44111111.11111111 k cow 1140 ocf cow 1270'. ilst cow 1025: f cow ocf cow 870 0 k cow 9150',1 1060'. )1.stcow 970' f cow 1075 d cow 890 0 k < cow 920 0 BULLS fbull 760 0 k bull 1255 0 1 f bull 1335 0r f bull 1050 0 STOCK PIGS white shts nixed shts ed pigs mixed pigs 61 white pigs 1 white pigs mixed pigs red pigs white pigs MMISSIO NY alongocno HEAP? throughtrom wif flood watersrry just ibarely gvered S closed; one carstalled 0 The highway was I thousands of acres in the area. parallels the high The railroad which n the water wasalmost covered. allay was washedout in one place. i MOVING TOHIGHER GROUND Alan and Ralph Larson help theirfather Howard 0. 1.44 flooded feel lotnear Tescott. Cattle Larson move dairystock from were moved to a pastureon higher ground. 1.10 Inc ANSI 13700 hen TheStreamsOverflow 1510 0: Co.- At*, 1709" Co. 14 ice Co. G&G area farmerscouldn't complain about not getting enough moisture ;0. @3 May. It wasa month that producedmore than its share of tornado warnings, aline Co. steady processionof grey days, some hail storms that devastated pockets of ay Co. G&G area, andfinally an accumulation of rainfall that 1065 @ ut of their banks. sent many streams 930@i Some of the places thatgot the worst of it are shown here a onpage 14, with pictures 10950:. by Kenneth Greene. o. 11700 ;0. 1320@ ;0. 1170@ ;o. 12400 th Co. 1115P 'ion Co. 1140@ 9250 Co. -

A/Dxvwltmthewx Ouwobkdoors
^^fe^^Sf^B^gM' jM'i m< *' w^*** jS!IlffHS^^^1W!5g THE MINNEAPOLIS JOURNAL. '• J^..^. A/DXVWlTmTHEWXMMMMMM»M»«*«*M*«*««*raM«MM(WM*««««cU»(M»aMMMMM«*M»M«MMM«MMM<raN I OUWOBkDOORS»»««»««»»«»«l«y—««»»»»•»»»«»««««« »««!»—IIHMHnni|HMWtM«»»"M« »•———»»»——" I T11M1 ••••»>• AMERICAN LEAGUE WINNING MACHINES IN MOUNT WASHINGTON CLIMBING CONTEST IDRUBBED SAINTS STANDING OF THE CLUBS. Played. Won. Lost. Pet. COLLEGE SEASOf v* Boston 70 . 50 20 .633 Chicago 82 40 33 ~ .598 ROM present outlook the automobile |- ON HOME FIELD New York 78 40 32 .590 Cleveland 75 42- 83 .56) « owners of the northwest are not A GREAT SUCCESS^ Philadelphia 77 42 35 .545 F St. Louis 74 33 41 .446 tumbling over each other in an attempt to •THOMAS HAD ST. PAUL ON THEDetroi t 77 31 46 .403 enter their names for the big automobile Washington. 76 16 60 .211 BIGGEST ATHLETIC YEAR ON ; ($, " GRIDDLE. l run to St. Louis. There are several rea GAMES YESTERDAY. THE RECORDS. , " *\ Chicago 6, New York 5. sons for this. Local chauffeurs are as St. Louis 5, Boston 2. good sportsmen as can be found in But Two of Kelly's Men Could Guess Cleveland 4, Philadelphia 0. America, but they are a bit more Steadily Increasing Number of Sports P Where the Ball Was Going1—Slagle Washington 0, Detroit 0. "weather-wise" than their brethren of the Has Been Taken Up by the Colle || a Christmas Box for Watkins' Men GAMES TODAY. Boston at Cincinnati. east. The making of the program for the gians Until Almost Every Abie- f^—Scene Shifts to Nicollet Park To- Brooklyn at Pittsburg. -

2010 Baseball Yearbook.Indd
1 22010010 HOOLYLY CRROSSOSS BAASEBALLSEBALL 2 22010010 HOOLYLY CRROSSOSS BAASEBALLSEBALL 3 22010010 HOOLYLY CRROSSOSS BAASEBALLSEBALL AT A GLLANCEANCE HOLY CROSS BASEBALL QUICK FACTS MISSION STATMENT Location: . .Worcester, MA 01610 COLLEGE OF THE HOLY CROSS Founded: . .1843 Enrollment: . 2,866 DEPARTMENT OF ATHLETICS Color: . Royal Purple The Mission of the Athletic Department of the College of the Nickname: . .Crusaders Holy Cross is to promote the intellectual, physical, and moral devel- Affi liations: . NCAA Division I, Patriot League opment of students. Through Division I athletic participation, our Home Field: . Fitton Field (3,000) young men and women student-athletes learn a self-discipline that Surface: . Grass has both present and long-term effects; the interplay of individual Dimensions: . L-332, LC-357, C-385, RC-372, R-313 and team effort; pride and self esteem in both victory and defeat; President: . .Rev. Michael C. McFarland, S.J. a skillful management of time; personal endurance and courage; Director of Admissions: . Ann McDermott and the complex relationships between friendship, leadership, and Offi ce Phone: . (508) 793-2443 service. Our athletics program, in the words of the College Mis- Director of Financial Aid: . Lynne M. Myers sion Statement, calls for “a community marked by freedom, mutual Offi ce Phone: . (508) 793-2265 respect, and civility.” Director of Athletics: . Richard M. Regan, Jr. Besides teaching these virtues, a few sports played at Holy Associate Director of Athletics:. .Bill Bellerose Cross have the added value of focusing alumni and student support Associate Director of Athletics:. Ann Zelesky and enhancing our reputation locally and nationally. While Holy Associate Director of Athletics:. -

Télécharger Le Fichier
rt!((((((()n))) lh. S A N T P E T E R 'S C 0 L l E G E APRIL FOOL APRIL FOOL EDITION PAlJ ow EDITION Vol. XXI Jersey City, N. J., April 1, 1953 No.11 Student Clamors Maj. Farrell On To l(orea Nix Faculty Bid With R.O.T.C. Contingent For Coed College In a dramatic statement yes terday, the Defense Department In the most startling upset since the David-Goliath bout, over announced that Major Eugene 11,000 students voted down the faculty-inspired bid for coeduca Farrell, former Professor of Mili tion at St. Peter's College. tary Science at St. Peter's Col When the first cry of "We Want Women" was heard thundering lege in Jersey City, has been from the faculty room two weeks ago, it was evident to all that named to replace Maxwell Tay the battle was on. Carrying placards lor as head of the Eighth Army in Korea. Major Farrell will ~.eading "Nix on ,,tl~e Broadies," and Council Votes F emales, Fooey, irate students pa- leave immediately and is to be accompanied by the ROTC ;;o:~d the halls in a protest demonstra- Appropriation band, the Pershing Rifles and all Hot Battle MS III cadets who will receive de fa cto commissions as second lieu As the time set for the plebiscite At yesterday's routine weekly meet- tenants in the infantry. by the Student Council neared: tlie ing, the Student Council appropriated General Taylor will return home to heat of controversy rose to fever pitch. -

The Kilmichael Ambush - a Review of Background, Controversies and Effects
The Kilmichael Ambush - A Review of Background, Controversies and Effects (Seamus Fox – September 2005) On the cold wintry evening of Sunday 28th November 1920, two Crossley tenders, each with nine cadets of the Auxiliary Division of the RIC on board, were travelling from their base in Macroom towards Dunmanway when they were ambushed about 1.5 miles south of the village of Kilmichael, Co Cork by the Flying Column of the 3rd (West) Cork Brigade of the IRA, led by Column Commander Tom Barry. While a number of details remain unclear and many others are disputed, what is clear and undisputed is that by the end of the ambush, nineteen men lay dead. Sixteen of the dead were Auxiliaries and three were IRA men. (For the casualties and details of the personnel – both Auxiliary and IRA involved, see Appendix. Also given in the Appendix is the disposition of the ambushers – the disposition assumes importance when the controversies that arose from the Kilmichael ambush are discussed below.) This essay will look at (1) The background to the ambush (2) The controversies that arose from the ambush and (3) The effects of the ambush. 1.0 Background The Auxiliaries1 arrived in the town of Macroom in early September 1920 (Twohig 1994, pg 126). According to Hart, they arrived in a "district whose police chief declared it to be 'practically in a state of war'. … Almost all the outlying police barracks had been evacuated and burned down … The [British] army had stepped in in May [1920] to try to restore order and found itself embroiled in a vicious little war in the Muskerry hill country west of the town with the Ballyvourney I.R.A. -
2012 Holy Cross Baseball Yearbook Is Published by Commitment to the Last Principle Assures That the College Secretary:
2 22012012 HOOLYLY CRROSSOSS BAASEBALLSEBALL AT A GLLANCEANCE HOLY CROSS QUICK FACTS COACHING STAFF MISSION STATMENT Location: . .Worcester, MA 01610 Head Coach:. Greg DiCenzo (St. Lawrence, 1998) COLLEGE OF THE HOLY CROSS Founded: . 1843 Career Record / Years: . 93-104-1 / Four Years Enrollment: . 2,862 Record at Holy Cross / Years: . 93-104-1 / Four Years DEPARTMENT OF ATHLETICS Color: . Royal Purple Assistant Coach / Recruiting Coordinator: The Mission of the Athletic Department of the College Nickname: . Crusaders . .Jeff Kane (Clemson, 2001) of the Holy Cross is to promote the intellectual, physical, Affi liations: . NCAA Division I, Patriot League Assistant Coach: and moral development of students. Through Division I President: . Rev. Philip L. Boroughs, S.J. Ron Rakowski (San Francisco State, 2002) athletic participation, our young men and women student- Director of Admissions: . Ann McDermott Assistant Coach:. Jeff Miller (Holy Cross, 2000) athletes learn a self-discipline that has both present and Offi ce Phone: . (508) 793-2443 Baseball Offi ce Phone:. (508) 793-2753 long-term effects; the interplay of individual and team effort; Director of Financial Aid: . Lynne M. Myers E-Mail Address: . [email protected] pride and self esteem in both victory and defeat; a skillful Offi ce Phone: . (508) 793-2265 Mailing Address: . .Greg DiCenzo management of time; personal endurance and courage; and Director of Athletics: . .Richard M. Regan, Jr. Head Baseball Coach the complex relationships between friendship, leadership, Associate Director of Athletics:. Bill Bellerose College of the Holy Cross and service. Our athletics program, in the words of the Associate Director of Athletics:. Ann Zelesky One College Street College Mission Statement, calls for “a community marked Associate Director of Athletics:. -

My Replay Baseball Encyclopedia Fifth Edition- May 2014
My Replay Baseball Encyclopedia Fifth Edition- May 2014 A complete record of my full-season Replays of the 1908, 1952, 1956, 1960, 1966, 1967, 1975, and 1978 Major League seasons as well as the 1923 Negro National League season. This encyclopedia includes the following sections: • A list of no-hitters • A season-by season recap in the format of the Neft and Cohen Sports Encyclopedia- Baseball • Top ten single season performances in batting and pitching categories • Career top ten performances in batting and pitching categories • Complete career records for all batters • Complete career records for all pitchers Table of Contents Page 3 Introduction 4 No-hitter List 5 Neft and Cohen Sports Encyclopedia Baseball style season recaps 91 Single season record batting and pitching top tens 93 Career batting and pitching top tens 95 Batter Register 277 Pitcher Register Introduction My baseball board gaming history is a fairly typical one. I lusted after the various sports games advertised in the magazines until my mom finally relented and bought Strat-O-Matic Football for me in 1972. I got SOM’s baseball game a year later and I was hooked. I would get the new card set each year and attempt to play the in-progress season by moving the traded players around and turning ‘nameless player cards” into that year’s key rookies. I switched to APBA in the late ‘70’s because they started releasing some complete old season sets and the idea of playing with those really caught my fancy. Between then and the mid-nineties, I collected a lot of card sets. -

2014 Baseball Yearbook.Indd
2 2014 HOLY CROSS BASEBALL AT A GLANCE HOLY CROSS QUICK FACTS COACHING STAFF MISSION STATMENT Location: . .Worcester, MA 01610 Head Coach:. Greg DiCenzo (St. Lawrence, 1998) COLLEGE OF THE HOLY CROSS Founded: . 1843 Career Record / Years: . 154-151-1 / Six Years Enrollment: . 2,891 Record at Holy Cross / Years: 154-151-1 / Six Years DEPARTMENT OF ATHLETICS Color: . Royal Purple E-Mail Address: . [email protected] The Mission of the Athletic Department of the College Nickname: . Crusaders Associate Head Coach Coach / Recruiting Coordinator: of the Holy Cross is to promote the intellectual, physical, Affiliations: . NCAA Division I, Patriot League . .Jeff Kane (Clemson, 2001) and moral development of students. Through Division I President: . Rev. Philip L. Boroughs, S.J. Assistant Coach: athletic participation, our young men and women student- Director of Admissions: . Ann McDermott . Ron Rakowski (San Francisco State, 2002) athletes learn a self-discipline that has both present and Office Phone: . (508) 793-2443 Assistant Coach:. Jeff Miller (Holy Cross, 2000) long-term effects; the interplay of individual and team effort; Director of Financial Aid: . .Lynne Myers Baseball Office Phone:. (508) 793-2753 pride and self esteem in both victory and defeat; a skillful Office Phone: . (508) 793-2265 Mailing Address: . Baseball Office management of time; personal endurance and courage; and Director of Athletics: . Nathan Pine College of the Holy Cross the complex relationships between friendship, leadership, Associate Director of Athletics:. Bill Bellerose One College Street and service. Our athletics program, in the words of the Associate Director of Athletics:. Ann Zelesky Worcester, MA 01610 College Mission Statement, calls for “a community marked Associate Director of Athletics:. -

Flight to Raise Money for a Good Cause and Hopefully Have Some Schedule Fun Doing It, Not Cause for May 26 - 30 Anyone Embarrassment
Guantanamo Bay, Cuba Vol. 42 -- No. 98 -- U.S. Navy's only shore-based daily newspaper -- Friday, May 23, 1986 N Radiothon is on the air until midnight Monday W; W~' JOl John McNally 1340) will be airing The minimum pledge for a song W4E News of the bay everything "live" starting request is $1.50. However, The whole purpose of a today, 11 a.m. until midnight anyone can call in while a Radiothon is to raise money Monday, May 26. The radio song is playing and have it for Navy Relief. This annual "bumped" off the air by station will sign on at 6 Taking Nominations For Spouse Of The Year -- Relief event is doubling the amount that was Navy a.m. every morning and sign The Family Service Center will again be coordinating sponsored by the Navy pledged by the original off at midnight each night. the "Spouse of the Year" Award. It has been designated Broadcasting Service During these times, base requester. to honor all spouses whose love, support and Bay, residents are invited to There will also be four Detachment Guantanamo understanding, within their family and the military is normally one of the "sustaining songs" each hour. and phone in pledges and request community, helps strengthen our military profession and bigger money makers. These songs will require a a certain song and dedicate the defense mission. In that spirit, nominations are radio station (AM minimum pledge of $100 to The AM it to someone if they desire. taken for that special person to bestow the start for each of the four now being title of "Spouse of the Year." Nominations should be times. -

History of Toledo Baseball (1883-2018)
History of Toledo Baseball (1883-2018) Year League W L PCT. GB Place Manager Attendance Stadium 1883 N.W.L. 56 28 .667 - - 1st* William Voltz/Charles Morton League Park 1884 A.A. 46 58 .442 27.5 8th Charles Morton 55,000 League Park/Tri-State Fairgrounds (Sat. & Sun.) 18851 W.L. 9 21 .300 NA 5th Daniel O’Leary League Park/Riverside Park (Sun.) 1886-87 Western League disbanded for two years 1888 T.S.L. 46 64 .418 30.5 8th Harry Smith/Frank Mountain/Robert Woods Presque Isle Park/Speranza Park 1889 I.L. 54 51 .568 15.0 4th Charles Morton Speranza Park 1890 A.A. 68 64 .515 20.0 4th Charles Morton 70,000 Speranza Park 1891 Toledo dropped out of American Association for one year 18922 W.L. 25 24 .510 13.5 4th Edward MacGregor 1893 Western League did not operate due to World’s Fair, Chicago 1894 W.L. 67 55 .549 4.5 2nd Dennis Long Whitestocking Park/Ewing Street Park 18953 W.L. 23 28 .451 27.5 8th Dennis Long Whitestocking Park/Ewing Street Park 1896 I.S.L. 86 46 .656 - - 1st* Frank Torreyson/Charles Strobel 45,000 Ewing Street Park/Bay View Park (Sat. & Sun.) 1897 I.S.L. 83 43 .659 - - 1st* Charles Strobel Armory Park/Bay View Park (Sat. & Sun.) 1898 I.S.L. 84 68 .553 0.5 2nd Charles Strobel Armory Park/Bay View Park (Sat. & Sun.) 1899 I.S.L. 82 58 .586 5.0 3rd (T) Charles Strobel Armory Park/Bay View Park (Sat. -
2017-18 Record Book
2017-18 RECORD BOOK 2017-18 BOSTON COLLEGE BASEBALL RECORD BOOK HONOR ROLL NATIONAL HONORS REGIONAL HONORS ALL-NEW ENGLAND THIRD TEAM 2017 Jake Alu BASEBALL AMERICA FIRST-TEAM ALL-AMERICA FIRST-TEAM ALL-ECAC 2016 Mike King 2009 Tony Sanchez, Jr. C 1998 Sean McGowan, Jr. 1B 2015 Blake Butera 1993 Mike Martin, Jr. 2B 2015 Mike King BASEBALL AMERICA THIRD-TEAM ALL-AMERICA 2015 Eric Stone 2016 Justin Dunn, Jr. P NCBWA DISTRICT I PLAYER OF THE YEAR 1999 Sean McGowan, Sr. 1B 2009 Mike Belfiore, Jr. 1B/P NEIBA ROOKIE OF THE YEAR 2003 Chris Lambert, So. P 2016 Jacob Stevens P ABCA/RAWLINGS SECOND-TEAM ALL-AMERICA 2009 Mike Belfiore, Jr. 1B/P NCBWA SMITH SUPER TEAM HONORABLE NEIBA ALL-STAR 2000 Steve Langone, Sr. UT MENTION 2014 Chris Shaw, So. OF 1994 Mike Martin, Sr. 2B Andrew Chin, Jr. P ABCA/RAWLINGS THIRD-TEAM ALL-AMERICA 2013 Hunter Gordon, Sr. P 2009 Tony Sanchez, Jr. C ABCA FIRST-TEAM ALL-NORTHEAST 2012 Tom Bourdon, So. OF* 1999 Sean McGowan, Sr. 1B 2015 Chris Shaw, Jr. OF Anthony Melchionda, Sr. SS* 1993 Mike Martin, Jr. 2B 2014 Chris Shaw, So. OF 2011 Matt McGovern, So. OF 2009 Mike Belfiore, Jr. 1B/P Kyle Prohovich, Jr. P NCBWA THIRD-TEAM ALL-AMERICA Tony Sanchez, Jr. C Garret Smith, Sr. P 2003 Chris Lambert, So. P 2004 Jason Delaney, Jr. OF 2010 John Spatola, Sr. OF 2000 Steve Langone, Sr. DH/UT 2002 Chris Lambert, Fr. P Mickey Wiswall, Jr. 1B 2001 Brian Macchi, Jr. 3B 2004 Jason Delaney, Jr. -
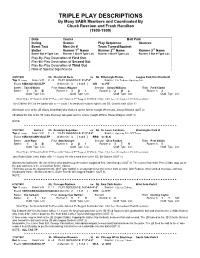
TRIPLE PLAY DESCRIPTIONS by Many SABR Members and Coordinated by Chuck Rosciam and Frank Hamilton (1900-1909)
TRIPLE PLAY DESCRIPTIONS By Many SABR Members and Coordinated By Chuck Rosciam and Frank Hamilton (1900-1909) Date Teams Ball Park Inning Scores Play Sequence Sources Event Text Men On # Team Turned/Against Batter Runner 1st Name Runner 2nd Name Runner 3rd Name Batter Out # Type Loc Runner 1 Out # Type Loc Runner 2 Out # Type Loc Runner 3 Out # Type Loc Play-By-Play Description of First Out Play-By-Play Description of Second Out Play-By-Play Description of Third Out Note of Special Significance 4/25/1900 NL Cincinnati Reds vs NL Pittsburgh Pirates League Park II in Cincinnati Top 3 Inning Score V-H 2 - 0 PLAY SEQUENCE: 6*-4*-3* Source: Chi Tribune; Sporting Life Event: 6(B)64(2)43(1)/LTP # Men On: 3 [ 1-2-3 ] CIN vs PIT Batter: Tom O'Brien First Honus Wagner Second Jimmy Williams Third Fred Clarke Batter: 1 G B Runner 1: 3 D 1 Runner 2: 2 D 2 Runner 3: 4 Out# Type Loc: Out# Type Loc: Out# Type Loc: Out# Type Loc: {Out Type: D=Doubled-Off F=Forced G=Gloved T=Tagged X=Strike-Out; Out Loc: Retrosheet Field Location} Tom O'Brien (PIT) is the batter with a ?-? count. He sends a line drive right to the SS, Charlie Irwin (OUT 1) SS throws over to the 2B (Harry Steinfeldt) who doubles up the runner caught off second, Jimmy Williams (OUT 2) 2B whips the ball to the 1B (Jake Beckley) who puts out the runner caught off first, Honus Wagner (OUT 3) NOTE: - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 5/22/1901 Game 2 NL Brooklyn Superbas vs NL St.