Understanding the Drivers of Litigation in Health Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Programme Enhancing Clinical Research Across the Globe
RCN International Nursing Research Conference and Exhibition 2019 Tuesday 3 - Thursday 5 September 2019 Sheffield Hallam University, UK Conference brochure kindly supported by media partner Accrue up to 27 hours #research2019 of CPD PATIENT STATUS Visit EDGE on stand 8 THE POWER OF DATA For everyone. Anywhere. In real-time. EDGE. Intelligent Research ManagementTM An innovative programme enhancing clinical research across the globe [email protected] www.edgeclinical.com Welcome 5 Acknowlegements and thanks 6 International Scientific Advisory Panel 7 General information 8 Venue Plan 10 Exhibitor listing 11 Programme Tuesday 3 September 13 Wednesday 4 September 18 Thursday 5 September 23 Posters Tuesday 3 September 28 Wednesday 4 September 29 Thursday 5 September 30 Royal College of Nursing 20 Cavendish Square London W1G 0RN rcn.org.uk 007 698 | August 2019 3 Library and Archive Service Exhibitions and events programme 24-hour access to thousands of e-books and e-journals at rcn.org.uk/library Help and advice on searching Libraries in Belfast, for information Cardiff, Edinburgh and London www.rcn.org.uk/library 0345 337 3368 @rcnlibraries @rcnlibraries 4 Library and Archive Service Welcome The theme of this year’s conference is the impact of nursing research. This is very fitting as 2019 is the Exhibitions and 60th year in which there has been a meeting of nurses to share their research and meet like-minded events programme colleagues. The first such meeting took place in the RCN headquarters in London in 1959 as a research discussion group attended by Doreen Norton, Winifred Raphael, Gertrude Ramsden, Muriel Skeet and Lisbeth Hockey. -
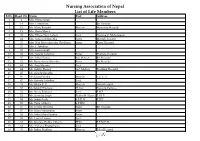
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

Design and Implementation of Health Information Systems
Design and implementation of health information systems Edited by Theo Lippeveld Director of Health Information Systems, John Snow Inc., Boston, MA, USA Rainer Sauerborn Director of the Department of Tropical Hygiene and Public Health, University of Heidelberg, Germany Claude Bodart Project Director, German Development Cooperation, Manila, Philippines World Health Organization Geneva 2000 WHO Library Cataloguing in Publication Data Design and implementation of health information systems I edited by Theo Lippeveld, Rainer Sauerborn, Claude Bodart. 1.1nformation systems-organization and administration 2.Data collection-methods I.Lippeveld, Theo II.Sauerborn, Rainer III.Bodart, Claude ISBN 92 4 1561998 (NLM classification: WA 62.5) The World Health Organization welcomes requests for permission to reproduce or translate its pub lications, in part or in full. Applications and enquiries should be addressed to the Office of Publi cations, World Health Organization, Geneva, Switzerland, which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © World Health Organization 2000 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the World Health Or ganization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Evaluation of Hospital Information System in the Northern Province in South Africa
EVALUATION OF HOSPITAL INFORMATION SYSTEM IN THE NORTHERN PROVINCE IN SOUTH AFRICA “ Using Outcome Measures” Report prepared for the HEALTH SYSTEMS TRUST By Nolwazi Mbananga Rhulani Madale Piet Becker THE MEDICAL RESEARCH COUNCIL OF SOUTH AFRICA PRETORIA May 2002 1 ACKNOWLEDGEMENTS The Department of Health and Welfare in the Northern Province is acknowledged for its mandate to conduct this study and its support of the project throughout. The project Team is recognised for its great efforts in developing the project proposal and obtaining the necessary funding to conduct the study, without which it would not have been possible. The project team members; Dr Jeremy Wyatt, Dr LittleJohns, Dr Herbst, Dr Zwarenstein, Dr Power, Dr Rawlinson, Dr De Swart, Dr P Becker, Ms Madale and others played a key role in maintaining the scientific rigour for the study and their dedication is appreciated. The MEDUNSA Community Health in the Northern Province is credited for the direction and support it provided during the early stages of project development, planning and implementation. It is important to explain that Ms Mbananga conducted the qualitative component of the study as a Principal investigator while she and Dr Becker were called upon to take over the quantitative component of the study and joined at the stage of post implementation data collection. The financial support that was provided by the Health Systems Trust and the Medical Research Council is highly valued this project could not have been started and successfully completed without it. We cannot forget our secretaries: Emily Gomes and Alta Hansen who assisted us in transcribing data. -

The Matron's Handbook
The matron’s handbook For aspiring and experienced matrons Updated July 2021 Contents Foreword........................................................................................ 2 Introduction .................................................................................... 4 The matron’s key roles................................................................... 6 1. Inclusive leadership, professional standards and accountability 8 2. Governance, patient safety and quality .................................... 12 3. Workforce planning and resource management ...................... 17 4. Patient experience and reducing health inequalities ................ 22 5. Performance and operational oversight ................................... 24 6. Digital and information technology ........................................... 27 7. Education, training and development ....................................... 33 8. Research and development ..................................................... 36 9. Collaborative working and clinical effectiveness ...................... 37 10. Service improvement and transformation .............................. 40 Appendix: The matron’s developmental framework and competencies............................................................................... 43 Acknowledgements ...................................................................... 51 1 | Contents Foreword Matrons are vital to delivering high quality care to patients and their relatives across the NHS and the wider health and care sector. They -

Divisional Structure - University Hospital Southampton NHS Foundation Trust – As at 1 July 2021
Divisional structure - University Hospital Southampton NHS Foundation Trust – as at 1 July 2021 Chief operating officer Joe Teape Division A Division B Division C Division D DCD – Andrew Webb DCD – Trevor Smith DCD – Freya Pearson DCD – David Higgs DDO – Greg Chapple DDO – Gavin Hawkins DDO – Martin De Sousa DHN/P – Rachel Davies DHN/P – Sarah Herbert DDO – Jacqui McAfee DHN/P – Louisa Green DHN/P – Natasha Watts Acuity Matron – Karen Hill DR&DL – Fraser Cummings DoM – Suzanne Cunningham DR&DL – Boyd Ghosh DR&DL – Bhaskar Somani DFM – John Light DR&DL – Luise Marino DFM – Alex Mawers (Interim) DS&BDM – Alison Gray DFM – Wayne Rogers DFM – Emma Hawkins DS&BDM – Adam Wells HRBP – Emma Watts DS&BDM – Dan Jeffery DS&BDM – Victoria Kearney HRBP – Rachel Dore HRBP – Rachel Dore (covering until replacement) Care groups HRBP – Katie Dunman (nee Molloy) Care groups Cancer care: Care groups Care groups Surgery: CGCL – Tim Iveson Women and newborn: Cardiovascular and thoracic: CGCL – John Knight CGM – Collette Byelong CGCL – Sarah Walker CGCL – Edwin Woo CGM – Justin Sanders (from 5/7/21) A/CGM – awaiting appointment CGM – Fiona Lawson CGM – Fiona Liddell A/CGM – Jon Watson Matron – Jenny Milner IP & Theatres Matron – Carol Gosling ACGM – Juliet Thomas A/CGM – Erin Flahavan Matron – Steph Churchill OP Matron – Karen Elkins Matron – Jenny Dove Neonatal Matron – Andrea Robson (interim) Matron – Kerry Rayner Matron – Julia Tonks Matron – Georgina Kirk Angie Ansell (from 12/7/21) Emergency medicine: Matron - Jean-Paul Evangelista Matron – Jo Rigby CGCL -

The Case of Modern Matrons in the English NHS
The dynamics of professions and development of new roles in public services organizations: The case of modern matrons in the English NHS Abstract This study contributes to research examining how professional autonomy and hierarchy impacts upon the implementation of policy designed to improve the quality of public services delivery through the introduction of new managerial roles. It is based on an empirical examination of a new role for nurses - modern matrons - who are expected by policy makers to drive organizational change aimed at tackling health care acquired infections [HCAI] in the National Health Service [NHS] within England. First, we show that the changing role of nurses associated with their ongoing professionalisation limit modern matron‟s influence over their own ranks in tackling HCAI. Second, modern matrons influence over doctors is limited. Third, government policy itself appears inconsistent in its support for the role of modern matrons. Modern matrons‟ attempts to tackle HCAI appear more effective where infection control activity is situated in professional practice and where modern matrons integrate aspirations for improved infection control within mainstream audit mechanisms in a health care organization. Key words: professions, NHS, modern matrons, health care acquired infections Introduction The organization and management of professional work remains a significant area of analysis (Ackroyd, 1996; Freidson, 2001; Murphy, 1990; Reed, 1996). It is argued that professional autonomy and hierarchy conflict with bureaucratic and managerial methods of organizing work, especially attempts at supervision (Broadbent and Laughlin, 2002; Freidson, 2001; Larson, 1979). Consequently, the extension of managerial prerogatives and organizational controls are seen to challenge the autonomy, legitimacy and power of professional groups (Clarke and Newman, 1997; Exworthy and Halford, 1999). -

Interventions to Reduce Unplanned Hospital Admission:A Series of Systematic Reviews Page 3
Interventions to reduce unplanned hospital admission: a series of systematic reviews Funded by National Institute for Health Research Research for Patient Benefit no. PB-PG-1208-18013 Sarah Purdy, University of Bristol Shantini Paranjothy, Cardiff University Alyson Huntley, University of Bristol Rebecca Thomas, Cardiff University Mala Mann, Cardiff University Dyfed Huws, Cardiff University Peter Brindle, NHS Bristol Glyn Elwyn, Cardiff University Final Report June 2012 Acknowledgements Advisory group Karen Bloor Senior research fellow, University of York Tricia Cresswell Deputy medical director of NHS North East Helen England Vice chair of the South of England Specialised Commissioning Group and chairs the Bristol Research and Development Leaders Group Martin Rowland Chair in Health Services Research, University of Cambridge Will Warin Professional Executive Committee Chair, NHS Bristol. Frank Dunstan Chair in Medical Statistics, Department of Epidemiology, Cardiff University Patient & public involvment group In association with Hildegard Dumper Public Involvement Manager at Bristol Community Health With additional support from Rosemary Simmonds Research associate University of Bristol Library support Lesley Greig and Stephanie Bradley at the Southmead Library & Information Service, Southmead Hospital, Westbury-on-Trym, Bristol and South Plaza library, NHS Bristol and Bristol Community Health, South Plaza, Marlborough Street, Bristol. Additional support David Salisbury assistance with paper screening. Funding This research was funded by the National Institute for Health Research, Research for Patient Benefit programme (grant PB-PG-1208-18013). This report presents independent research commissioned by the National Institute of Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. -

Telehealth/Telenursing for Registered Nurses 1
Nursing Care Quality Assurance Commission PO BOX 47864 i Olympia Washington 98504-7864 Tel: 360-236-4725i Fax: 360-236-4738 Telehealth/Telenursing For Registered Nurses 1. Telephone triage and nursing consultation by telephone or other electronic technology, incorporates unique knowledge, skill and competencies. Nurses employ the full range of the nursing process to gather data, make assessments, and generate plans for care via telephone encounters with patients. 2. Protocols are appropriate tools for implementing treatment plans. A registered nurse may use a protocol that has been written and approved by a physician to initiate a standing order for a medication or treatment. Assuming an appropriate patient-prescriber relationship exists, authorized standing orders may be implemented without consulting an authorized prescriber for a particular patient. The registered nurse should implement only standing orders which include a target population, exclusions, the population served, contraindications, special considerations, a specific order, a description of who has the authority to implement the order, physician signature, and review and approval by nursing as well as other involved disciplines. 3. Practice guidelines and protocols for care should be developed based on scientific/empirical evidence and outcomes data or expert opinion. Methods for periodic review of these tools to evaluate care effectiveness and currency of information should be in place. 4. Practice guidelines should evolve through collaboration and professional consensus among all involved health care disciplines. 5. When functions of the nurse involve complex decision making, even when driven by algorithm and protocol, telenursing should be limited to the practice of registered nursing. Licensed practical nursing activities within this context may include information gathering and the provision of patient education. -
Building Standard-Based Nursing Information Systems
Building Standard-Based Nursing Information Systems Pan American Health Organization World Health Organization Division of Health Systems and Services Development Essential Drugs and Technology Organization and Management of Health Systems and Services Human Resource Development December 2000 PAHO Library Cataloguing in Publication Data Pan American Health Organization. Building Standard-Based Nursing Information Systems. Washington, D.C. : PAHO, © 2000. 141 p. ISBN 92 75 12364 0 I. Title. 1. INFORMATION SYSTEMS. 2. NURSING. 3. NURSING PRACTICE CLASSIFICATIONS. 4. QUALITY OF HEALTHCARE. 5. MANUALS NLM W26.55.I4.p187 2001 ISBN 92 75 12364 0 The Pan American Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. Applications and inquiries should be addressed to the Publications Program, Pan American Health Organization, Washington, D.C., which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © Pan American Health Organization, 2000 Publications of the Pan American Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the Pan American Health Organization concerning the legal status of any country, territory, city, or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the Pan American Health Organization in preference to others of a similar nature that are not mentioned.