Design and Implementation of Health Information Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
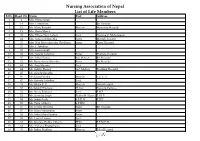
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

The Study on Improvement of Management Information Systems in Health Sector in the Islamic Republic of Pakistan
JAPAN INTERNATIONAL COOPERATION AGENCY (JICA) MINISTRY OF HEALTH, ISLAMIC REPUBLIC OF PAKISTAN THE STUDY ON IMPROVEMENT OF MANAGEMENT INFORMATION SYSTEMS IN HEALTH SECTOR IN THE ISLAMIC REPUBLIC OF PAKISTAN NATIONAL ACTION PLAN FEBRUARY 2007 NATIONAL HEALTH INFORMATION RESOURCE CENTER HM SYSTEM SCIENCE CONSULTANTS INC. JR 06-46 Japan International Cooperation Agency Ministry of Health, Islamic Republic of Pakistan THE STUDY ON IMPROVEMENT OF MANAGEMENT INFORMATION SYSTEMS IN HEALTH SECTOR IN THE ISLAMIC REPUBLIC OF PAKISTAN NATIONAL ACTION PLAN February 2007 National Health Information Resource Center System Science Consultants Inc. EXECUTIVE SUMMARY The National Action Plan for the Improvement of Health Information Systems in Pakistan Executive Summary The overall purpose of Health Information System (HIS) is to provide continuous information support to decision-making processes at each decision-making levels of the health system. Improving HIS in Pakistan is seen as an important investment towards improving the health care services. The guiding principle for the improvement of HIS in Pakistan is that the HIS should contribute to the continuous performance improvement of the health system in Pakistan with a vision of improving the overall health status of the population. After devolution in 2001, the districts are responsible for decision-making for health resource management and improving health services, particularly preventive, promotive and curative health services provided from primary and secondary level care facilities and outreach. A major objective of the management of the district health system is to improve its performance in order to contribute to the improvement of the health status of the population. Regular monitoring of the performance of health care services and their supporting sub-systems (e.g., logistics, financial, human resource management systems) is the first step in the performance improvement function of the district. -

Specific Requirements for a Secondary (Referral) Hospital
SPECIFIC REQUIREMENTS FOR A SECONDARY (REFERRAL) HOSPITAL A secondary (referral) hospital shall be defined as a facility with the following minimum requirements as listed under sections A to I below: A. Personnel B. Services C. Premises - Physical Design, Layout, Furnishing and Ancillary Facilities D. Equipment Devices and Supplies E. Wards F. Catering G. Safety and Security H. Schedules I. Records A. Personnel The minimum requirements regarding personnel for a secondary (referral) hospital must be separated according to the following 1. Board Members 2. Management Team 3. Sub-Committees 4. Heads of Departments/Units 5. Medical Practitioners 6. Additional professional staff 7. Auxiliary Staff 8. Ancillary staff (non-professional staff) 1. Board Members (Act 525) A Chairman who shall not be an employee of the hospital; The Chief Administrator of the hospital (Medical Director) The Dean of the relevant Medical School; SECONDARY HOSPITAL REQUIREMENTS Page 1 of 22 Version 1.3 dated 17-Nov-2017 The Director of Administration of the hospital; The Director of Nursing Services of the hospital; The Director of Finance of the hospital; The Director of Pharmacy of the hospital; The Dean of the Dental School, where applicable; and Three other persons who by their qualification and experience can contribute to the work of the Board at least one of whom shall be a woman 2. Management Team Chief Executive Officer for the hospital must have a masters degree Director of General Administration must have a master’s degree in hospital management -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

Health Care Services
Document of The World Bank FOR OFFICIAL USE ONLY Public Disclosure Authorized Report No: PAD885 INTERNATIONAL DEVELOPMENT ASSOCIATION PROJECT APPRAISAL DOCUMENT ON A PROPOSED GRANT Public Disclosure Authorized IN THE AMOUNT OF SDR 10.22 MILLION (US$15.79 MILLION EQUIVALENT) AND A PROPOSED GRANT IN THE AMOUNT OF US$5 MILLION FROM THE MULTI-DONOR TRUST FUND FOR HEALTH RESULTS INNOVATION Public Disclosure Authorized TO THE REPUBLIC OF CHAD FOR A MOTHER AND CHILD HEALTH SERVICES STRENGTHENING PROJECT May 6, 2014 Health, Nutrition and Population (AFTHW) Country Department West Africa (AFCW3) Public Disclosure Authorized This document has a restricted distribution and may be used by recipients only in the performance of their official duties. Its contents may not otherwise be disclosed without World Bank authorization. CURRENCY EQUIVALENTS (Exchange Rate Effective March 31, 2014) Currency Unit = Franc CFA (FCFA) XAF 475.38 = US$1 US$1.55 = SDR 1 FISCAL YEAR January 1 – December 31 ABBREVIATIONS AND ACRONYMS AF Additional Financing AIDS Acquired Immuno-Deficiency Syndrome AFTEM Africa Region Financial Management Unit ANC Ante-Natal Care ARI Acute Respiratory Infection CAS Country Assistance Strategy CBO Community-based Organizations CFAF Central African Franc CHW Community Health Worker CPA Central Pharmaceutical Purchasing Agency CPA Complementary Package of Actions CPAR Country Procurement Assessment Report CPIA Country Policy and Institutional Assessment CPS Country Partnership Strategy CSO Civil Society Organization DALY Disability-Adjusted -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

Greene Memorial Hospital Community Health Needs Assessment Greene Memorial Hospital Community Health Needs Assessment 2013
2013 Greene Memorial Hospital Community Health Needs Assessment Greene Memorial Hospital Community Health Needs Assessment 2013 Table of Contents Figures ....................................................................................................................................................... ii Introduction .................................................................................................................................................. 1 How to Read This Report .......................................................................................................................... 1 Definition of the Community Served ........................................................................................................ 2 Consulting Persons and Organizations ..................................................................................................... 2 Demographics of the Community ................................................................................................................. 3 Characteristics of the Population .............................................................................................................. 3 Health Care Facilities and Resources within the Community ....................................................................... 5 Hospital ..................................................................................................................................................... 6 Clinics ....................................................................................................................................................... -

MASS CASUALTY TRAUMA TRIAGE PARADIGMS and PITFALLS July 2019
1 Mass Casualty Trauma Triage - Paradigms and Pitfalls EXECUTIVE SUMMARY Emergency medical services (EMS) providers arrive on the scene of a mass casualty incident (MCI) and implement triage, moving green patients to a single area and grouping red and yellow patients using triage tape or tags. Patients are then transported to local hospitals according to their priority group. Tagged patients arrive at the hospital and are assessed and treated according to their priority. Though this triage process may not exactly describe your agency’s system, this traditional approach to MCIs is the model that has been used to train American EMS As a nation, we’ve got a lot providers for decades. Unfortunately—especially in of trailers with backboards mass violence incidents involving patients with time- and colored tape out there critical injuries and ongoing threats to responders and patients—this model may not be feasible and may result and that’s not what the focus in mis-triage and avoidable, outcome-altering delays of mass casualty response is in care. Further, many hospitals have not trained or about anymore. exercised triage or re-triage of exceedingly large numbers of patients, nor practiced a formalized secondary triage Dr. Edward Racht process that prioritizes patients for operative intervention American Medical Response or transfer to other facilities. The focus of this paper is to alert EMS medical directors and EMS systems planners and hospital emergency planners to key differences between “conventional” MCIs and mass violence events when: • the scene is dynamic, • the number of patients far exceeds usual resources; and • usual triage and treatment paradigms may fail. -

Evaluation of Hospital Information System in the Northern Province in South Africa
EVALUATION OF HOSPITAL INFORMATION SYSTEM IN THE NORTHERN PROVINCE IN SOUTH AFRICA “ Using Outcome Measures” Report prepared for the HEALTH SYSTEMS TRUST By Nolwazi Mbananga Rhulani Madale Piet Becker THE MEDICAL RESEARCH COUNCIL OF SOUTH AFRICA PRETORIA May 2002 1 ACKNOWLEDGEMENTS The Department of Health and Welfare in the Northern Province is acknowledged for its mandate to conduct this study and its support of the project throughout. The project Team is recognised for its great efforts in developing the project proposal and obtaining the necessary funding to conduct the study, without which it would not have been possible. The project team members; Dr Jeremy Wyatt, Dr LittleJohns, Dr Herbst, Dr Zwarenstein, Dr Power, Dr Rawlinson, Dr De Swart, Dr P Becker, Ms Madale and others played a key role in maintaining the scientific rigour for the study and their dedication is appreciated. The MEDUNSA Community Health in the Northern Province is credited for the direction and support it provided during the early stages of project development, planning and implementation. It is important to explain that Ms Mbananga conducted the qualitative component of the study as a Principal investigator while she and Dr Becker were called upon to take over the quantitative component of the study and joined at the stage of post implementation data collection. The financial support that was provided by the Health Systems Trust and the Medical Research Council is highly valued this project could not have been started and successfully completed without it. We cannot forget our secretaries: Emily Gomes and Alta Hansen who assisted us in transcribing data. -

The Matron's Handbook
The matron’s handbook For aspiring and experienced matrons Updated July 2021 Contents Foreword........................................................................................ 2 Introduction .................................................................................... 4 The matron’s key roles................................................................... 6 1. Inclusive leadership, professional standards and accountability 8 2. Governance, patient safety and quality .................................... 12 3. Workforce planning and resource management ...................... 17 4. Patient experience and reducing health inequalities ................ 22 5. Performance and operational oversight ................................... 24 6. Digital and information technology ........................................... 27 7. Education, training and development ....................................... 33 8. Research and development ..................................................... 36 9. Collaborative working and clinical effectiveness ...................... 37 10. Service improvement and transformation .............................. 40 Appendix: The matron’s developmental framework and competencies............................................................................... 43 Acknowledgements ...................................................................... 51 1 | Contents Foreword Matrons are vital to delivering high quality care to patients and their relatives across the NHS and the wider health and care sector. They -

Divisional Structure - University Hospital Southampton NHS Foundation Trust – As at 1 July 2021
Divisional structure - University Hospital Southampton NHS Foundation Trust – as at 1 July 2021 Chief operating officer Joe Teape Division A Division B Division C Division D DCD – Andrew Webb DCD – Trevor Smith DCD – Freya Pearson DCD – David Higgs DDO – Greg Chapple DDO – Gavin Hawkins DDO – Martin De Sousa DHN/P – Rachel Davies DHN/P – Sarah Herbert DDO – Jacqui McAfee DHN/P – Louisa Green DHN/P – Natasha Watts Acuity Matron – Karen Hill DR&DL – Fraser Cummings DoM – Suzanne Cunningham DR&DL – Boyd Ghosh DR&DL – Bhaskar Somani DFM – John Light DR&DL – Luise Marino DFM – Alex Mawers (Interim) DS&BDM – Alison Gray DFM – Wayne Rogers DFM – Emma Hawkins DS&BDM – Adam Wells HRBP – Emma Watts DS&BDM – Dan Jeffery DS&BDM – Victoria Kearney HRBP – Rachel Dore HRBP – Rachel Dore (covering until replacement) Care groups HRBP – Katie Dunman (nee Molloy) Care groups Cancer care: Care groups Care groups Surgery: CGCL – Tim Iveson Women and newborn: Cardiovascular and thoracic: CGCL – John Knight CGM – Collette Byelong CGCL – Sarah Walker CGCL – Edwin Woo CGM – Justin Sanders (from 5/7/21) A/CGM – awaiting appointment CGM – Fiona Lawson CGM – Fiona Liddell A/CGM – Jon Watson Matron – Jenny Milner IP & Theatres Matron – Carol Gosling ACGM – Juliet Thomas A/CGM – Erin Flahavan Matron – Steph Churchill OP Matron – Karen Elkins Matron – Jenny Dove Neonatal Matron – Andrea Robson (interim) Matron – Kerry Rayner Matron – Julia Tonks Matron – Georgina Kirk Angie Ansell (from 12/7/21) Emergency medicine: Matron - Jean-Paul Evangelista Matron – Jo Rigby CGCL -

Factors Determining Water Treatment Behavior for the Prevention of Cholera in Chad
Am. J. Trop. Med. Hyg., 93(1), 2015, pp. 57–65 doi:10.4269/ajtmh.14-0613 Copyright © 2015 by The American Society of Tropical Medicine and Hygiene Factors Determining Water Treatment Behavior for the Prevention of Cholera in Chad Jonathan Lilje,* Hamit Kessely, and Hans-Joachim Mosler Eawag: Swiss Federal Institute of Aquatic Science and Technology, Du¨bendorf, Switzerland; Centre de Support en Sante´ Internationale (CSSI), N’Djamena, Chad Abstract. Cholera is a well-known and feared disease in developing countries, and is linked to high rates of morbidity and mortality. Contaminated drinking water and the lack of sufficient treatment are two of the key causes of high transmission rates. This article presents a representative health survey performed in Chad to inform future intervention strategies in the prevention and control of cholera. To identify critical psychological factors for behavior change, structured household interviews were administered to N = 1,017 primary caregivers, assessing their thoughts and attitudes toward household water treatment according to the Risk, Attitude, Norm, Ability, and Self-regulation model. The intervention potential for each factor was estimated by analyzing differences in means between groups of current performers and nonperformers of water treatment. Personal risk evaluation for diarrheal diseases and particularly for cholera was very low among the study population. Likewise, the perception of social norms was found to be rather unfavorable for water treatment behaviors. In addition, self-reported ability estimates (self-efficacy) revealed some poten- tial for intervention. A mass radio campaign is proposed, using information and normative behavior change techniques, in combination with community meetings focused on targeting abilities and personal commitment to water treatment.