15-1040-Junu Oh-Neuronal.Key
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

St. Lawrence School Subject
St. Lawrence School Subject - Science Class - 4 Chapter - 3 Human Body : Digestive and Excetory System ( Part - 1 ) Learn about * Digestive system * Excretory system * Healthy eating habits Digestive System The process by which food is broken down into a simpler form so that it can be easily taken in or absorbed by our body is called digestion. Many organs work together and help in the process of digestion. The mouth, food pipe, stomach, small and large intestine, liver, rectum, and anus are the main organs of the digestive system. Let us learn about them. Mouth Digestion starts in the mouth. The teeth help to break down and chew food. The chewed food then mixes with a liquid, called saliva, produced in our mouth. It makes the food softer and easier to swallow. The tongue helps in the proper mixing of saliva with the food. Food pipe The food pipe ( oesophagus ) passes the food from the mouth to the stomach. Stomach Inside the stomach, the food is broken down further into smaller pieces by churning and with the help of chemicals called digestive juices. Small intestine From the small intestine, the undigested food passes into the large intestine. The large intestine is a shorter but wider, tube - like structure, which collects the indigestible food from the small intestine. The large intestine absorbs water from this undigested food and forms waste products called faeces. Rectum Rectum is the final part of the large intestine. Faeces are stored in the rectum for a short time before being passed out through anus. Anus Faeces are removed from the body through the anus. -

Gluteal Region-II
Gluteal Region-II Dr Garima Sehgal Associate Professor King George’s Medical University UP, Lucknow Structures in the Gluteal region • Bones & joints • Ligaments Thickest muscle • Muscles • Vessels • Nerves Thickest nerve • Bursae Learning Objectives By the end of this teaching session Gluteal region –II all the MBBS 1st year students must be able to: • Enumerate the nerves of gluteal region • Write a short note on nerves of gluteal region • Describe the location & relations of sciatic nerve in gluteal region • Enumerate the arteries of gluteal region • Write a short note on arteries of gluteal region • Enumerate the arteries taking part in trochanteric and cruciate anastomosis • Write a short note on trochanteric and cruciate anastomosis • Enumerate the structures passing through greater sciatic foramen • Enumerate the structures passing through lesser sciatic foramen • Enumerate the bursae in relation to gluteus maximus • Enumerate the structures deep to gluteus maximus • Discuss applied anatomy Nerves of Gluteal region (all nerves in gluteal region are branches of sacral plexus) Superior gluteal nerve (L4,L5, S1) Inferior gluteal nerve (L5, S1, S2) FROM DORSAL DIVISIONS Perforating cutaneous nerve (S2,S3) Nerve to quadratus femoris (L4,L5, S1) Nerve to obturator internus (L5, S1, S2) FROM VENTRAL DIVISIONS Pudendal nerve (S2,S3,S4) Sciatic nerve (L4,L5,S1,S2,S3) Posterior cutaneous nerve of thigh FROM BOTH DORSAL &VENTRAL (S1,S2) & (S2,S3) DIVISIONS 1. Superior Gluteal nerve (L4,L5,S1- dorsal division) 1 • Enters through the greater 3 sciatic foramen • Above piriformis 2 • Runs forwards between gluteus medius & gluteus minimus • SUPPLIES: 1. Gluteus medius 2. Gluteus minimus 3. Tensor fasciae latae 2. -

Urinary Bladder – Proteinaceous Plug
Urinary bladder – Proteinaceous Plug Figure Legend: Figure 1 An eosinophilic amorphous proteinaceous plug in the bladder lumen from a male B6C3F1 mouse in a chronic study. Figure 2 A proteinaceous plug associated with other flocculent, eosinophilic material, from a male F344/N rat in an acute study. Comment: Proteinaceous plugs are commonly noted as a postmortem change resulting from an agonal secretion of accessory sex gland fluids during euthanasia. Proteinaceous plugs vary in size but can be large, filling the urinary bladder (Figure 1 and Figure 2). Microscopically, the plug is composed of a mixture of an amorphous eosinophilic material, sometimes containing desquamated epithelial cells and spermatozoa. Proteinaceous plugs by themselves have no toxicologic importance and are not precursors of calculi. Plugs may be seen with obstructive syndromes associated with bacterial inflammation. They must be differentiated from calculi. Recommendation: Proteinaceous plugs occurring alone and not associated with any pathologic lesions should be recognized as an artifact and should not be diagnosed. Occasionally, proteinaceous plugs are recognized grossly, and the pathologist should use his or her judgment to correlate the gross lesion to an artifactual proteinaceous plug. 1 Urinary bladder – Proteinaceous Plug References: Gaillard ET. 1999. Ureter, urinary bladder and urethra. In: Pathology of the Mouse: Reference and Atlas (Maronpot RR, Boorman GA, Gaul BW, eds). Cache River Press, Vienna, IL, 235– 258. Abstract: http://www.cacheriverpress.com/books/pathmouse.htm Hard GC, Alden CL, Bruner RH, Frith CH, Lewis RM, Owen RA, Krieg K, Durchfeld-Meyer B. 1999. Non-proliferative lesions of the kidney and lower urinary tract in rats. -

Pudendal Nerve Entrapment Syndrome Caused by Ganglion Cysts Along
Case report eISSN 2384-0293 Yeungnam Univ J Med 2021;38(2):148-151 https://doi.org/10.12701/yujm.2020.00437 Pudendal nerve entrapment syndrome caused by ganglion cysts along the pudendal nerve Young Je Kim1, Du Hwan Kim2 1Department of Rehabilitation Medicine, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea 2Department of Physical Medicine and Rehabilitation, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea Received: June 5, 2020 Revised: June 22, 2020 Pudendal nerve entrapment (PNE) syndrome refers to the condition in which the pudendal nerve Accepted: June 23, 2020 is entrapped or compressed. Reported cases of PNE associated with ganglion cysts are rare. Deep gluteal syndrome (DGS) is defined as compression of the sciatic or pudendal nerve due to a Corresponding author: non-discogenic pelvic lesion. We report a case of PNE caused by compression from ganglion cysts Du Hwan Kim, MD, PhD and treated with steroid injection; we discuss this case in the context of DGS. A 77-year-old Department of Physical Medicine woman presented with a 3-month history of tingling and burning sensations in the left buttock and Rehabilitation, Chung-Ang and perineal area. Ultrasonography showed ganglion cystic lesions at the subgluteal space. Mag- University Hospital, Chung-Ang netic resonance imaging revealed cystic lesions along the pudendal nerve from below the piri- University College of Medicine, 102 formis to the Alcock’s canal and a full-thickness tear of the proximal hamstring tendon. Aspira- Heukseok-ro, Dongjak-gu, Seoul tion of the cysts did not yield any material. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -
Diagnosis, Rehabilitation and Preventive Strategies for Pudendal Neuropathy in Cyclists, a Systematic Review
Journal of Functional Morphology and Kinesiology Review Diagnosis, Rehabilitation and Preventive Strategies for Pudendal Neuropathy in Cyclists, A Systematic Review Rita Chiaramonte 1,* , Piero Pavone 2 and Michele Vecchio 1,3,* 1 Department of Biomedical and Biotechnological Sciences, Section of Pharmacology, University of Catania, 95123 Catania, Italy 2 Department of Clinical and Experimental Medicine, University Hospital “Policlinico-San Marco”, 95123 Catania, Italy; [email protected] 3 Rehabilitation Unit, “AOU Policlinico G.Rodolico”, 95123 Catania, Italy * Correspondence: [email protected] (R.C.); [email protected] (M.V.); Tel.: +39-(095)3782703 (M.V.); Fax: +39-(095)7315384 (R.C.) Abstract: This systematic review aims to provide an overview of the diagnostic methods, preventive strategies, and therapeutic approaches for cyclists suffering from pudendal neuropathy. The study defines a guide in delineating a diagnostic and therapeutic protocol using the best current strategies. Pubmed, EMBASE, the Cochrane Library, and Scopus Web of Science were searched for the terms: “Bicycling” OR “Bike” OR “Cyclists” AND “Neuropathy” OR “Pudendal Nerve” OR “Pudendal Neuralgia” OR “Perineum”. The database search identified 14,602 articles. After the titles and abstracts were screened, two independent reviewers analyzed 41 full texts. A total of 15 articles were considered eligible for inclusion. Methodology and results of the study were critically appraised in conformity with PRISMA guidelines and PICOS criteria. Fifteen articles were included in the systematic review and were used to describe the main methods used for measuring the severity of pudendal neuropathy and the preventive and therapeutic strategies for nerve impairment. Future Citation: Chiaramonte, R.; Pavone, P.; Vecchio, M. Diagnosis, research should determine the validity and the effectiveness of diagnostic and therapeutic strategies, Rehabilitation and Preventive their cost-effectiveness, and the adherences of the sportsmen to the treatment. -

1535190852 9 Medical Terminology Urinary.Pdf
Syrian Private University Medical Faculty Medical Terminology M.A.Kubtan , MD – FRCS Lecture 9 M.A.Kubtan Objectives After studying this chapter, you will be able to: •Name the parts of the urinary system and discuss the function of each part •Define combining forms used in building words that relate to the urinary system •Identify the meaning of related abbreviations •Name the common diagnoses, clinical procedures, and laboratory tests used in treating disorders of the urinary system M.A.Kubtan 2 Objectives Part 2 •List and define the major pathological conditions of the urinary system •Explain the meaning of surgical terms related to the urinary system •Recognize common pharmacological agents used in treating the urinary system M.A.Kubtan 3 Structure and Function The Urinary System Bladder Kidneys •Also called the excretory system •Maintains water Urinary System balance •Removes waste products from the Urethra Ureters blood by excreting them in the urine Meatus M.A.Kubtan 4 Kidneys Kidneys The kidneys are bean-shaped organs located in the retroperitoneal portion of the abdominal cavity on either side of the vertebral column. Two Primary Functions •To form urine for excretion •To retain essential substances the body needs in the process called reabsorption M.A.Kubtan 5 Parts of the Kidney Kidneys filter about 1700 kidney liters of blood daily in the average adult. medulla Parts of the kidneys •Cortex hilum -outer protective portion •Medulla -inner soft portion •Hilum -a depression located in the middle of the concave side of the kidney where blood vessels, nerves, and the ureters enter and cortex exit the kidneys M.A.Kubtan 6 Urine Production Urine is produced by filtration of: •water •sugar •creatine •salts •urea •uric acid Each kidney contains more than 1 million nephrons which are the functional units of the kidneys. -

Urology & Incontinence
Urology & Incontinence - Glossary of Terms Anti-reflux Refers to a tube or collapsible material within a urine collection device to help prevent urine from reentering the tubing. Applicator collar Found on some Hollister male external catheters, a plastic guide with notches for the thumb and forefinger to assist proper placement against the tip of the penis. Aseptic intermittent catheterization The process of performing intermittent catheterization using sterile equipment and inserting the catheter in a sterile way. This would include a sterile ready-to-use product that can be inserted with gloves using a no-touch technique (e.g., the Advance Plus intermittent catheter or a VaPro hydrophilic catheter). Benzalkonium chloride (BZK) An antimicrobial solution used for cleansing the urethral opening prior to inserting an intermittent catheter. Does not stain skin or clothing. Bladder A collapsible balloon-like muscular organ that lies in the pelvis and functions to store and expel urine. Bladder catheterization A procedure in which a catheter is passed through the urethra or stoma into the bladder, usually for the purpose of draining urine. Bladder control The ability to control urination. Bladder diary A printed or electronic form to keep track of when one urinates or leaks urine. Catheter (urinary) A special type of hollow tube inserted through the urethra or a stoma to the bladder to withdraw urine or instill medication. Catheterization The process of inserting a tube into the bladder to drain urine. Clean intermittent catheterization The process of emptying the bladder using a clean intermittent catheter. It involves inserting and removing a catheter, typically several times a day. -
Neuroscience
NEUROSCIENCE SCIENCE OF THE BRAIN AN INTRODUCTION FOR YOUNG STUDENTS British Neuroscience Association European Dana Alliance for the Brain Neuroscience: the Science of the Brain 1 The Nervous System P2 2 Neurons and the Action Potential P4 3 Chemical Messengers P7 4 Drugs and the Brain P9 5 Touch and Pain P11 6 Vision P14 Inside our heads, weighing about 1.5 kg, is an astonishing living organ consisting of 7 Movement P19 billions of tiny cells. It enables us to sense the world around us, to think and to talk. The human brain is the most complex organ of the body, and arguably the most 8 The Developing P22 complex thing on earth. This booklet is an introduction for young students. Nervous System In this booklet, we describe what we know about how the brain works and how much 9 Dyslexia P25 there still is to learn. Its study involves scientists and medical doctors from many disciplines, ranging from molecular biology through to experimental psychology, as well as the disciplines of anatomy, physiology and pharmacology. Their shared 10 Plasticity P27 interest has led to a new discipline called neuroscience - the science of the brain. 11 Learning and Memory P30 The brain described in our booklet can do a lot but not everything. It has nerve cells - its building blocks - and these are connected together in networks. These 12 Stress P35 networks are in a constant state of electrical and chemical activity. The brain we describe can see and feel. It can sense pain and its chemical tricks help control the uncomfortable effects of pain. -

The Peripheral Nervous System
The Peripheral Nervous System Dr. Ali Ebneshahidi Peripheral Nervous System (PNS) – Consists of 12 pairs of cranial nerves and 31 pairs of spinal nerves. – Serves as a critical link between the body and the central nervous system. – peripheral nerves contain an outermost layer of fibrous connective tissue called epineurium which surrounds a thinner layer of fibrous connective tissue called perineurium (surrounds the bundles of nerve or fascicles). Individual nerve fibers within the nerve are surrounded by loose connective tissue called endoneurium. Cranial Nerves Cranial nerves are direct extensions of the brain. Only Nerve I (olfactory) originates from the cerebrum, the remaining 11 pairs originate from the brain stem. Nerve I (Olfactory)- for the sense of smell (sensory). Nerve II (Optic)- for the sense of vision (sensory). Nerve III (Oculomotor)- for controlling muscles and accessory structures of the eyes ( primarily motor). Nerve IV (Trochlear)- for controlling muscles of the eyes (primarily motor). Nerve V (Trigeminal)- for controlling muscles of the eyes, upper and lower jaws and tear glands (mixed). Nerve VI (Abducens)- for controlling muscles that move the eye (primarily motor). Nerve VII (Facial) – for the sense of taste and controlling facial muscles, tear glands and salivary glands (mixed). Nerve VIII (Vestibulocochlear)- for the senses of hearing and equilibrium (sensory). Nerve IX (Glossopharyngeal)- for controlling muscles in the pharynx and to control salivary glands (mixed). Nerve X (Vagus)- for controlling muscles used in speech, swallowing, and the digestive tract, and controls cardiac and smooth muscles (mixed). Nerve XI (Accessory)- for controlling muscles of soft palate, pharynx and larynx (primarily motor). Nerve XII (Hypoglossal) for controlling muscles that move the tongue ( primarily motor). -
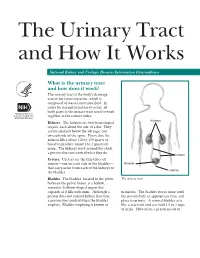
The Urinary Tract and How It Works
The Urinary Tract and How It Works National Kidney and Urologic Diseases Information Clearinghouse What is the urinary tract and how does it work? The urinary tract is the body’s drainage system for removing urine, which is composed of wastes and extra fluid. In order for normal urination to occur, all body parts in the urinary tract need to work together in the correct order. Kidneys Kidneys. The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine. The kidneys work around the clock; a person does not control what they do. Ureters Ureters. Ureters are the thin tubes of muscle—one on each side of the bladder— Bladder that carry urine from each of the kidneys to Urethra the bladder. Bladder. The bladder, located in the pelvis The urinary tract between the pelvic bones, is a hollow, muscular, balloon-shaped organ that expands as it fills with urine. Although a urination. The bladder stores urine until person does not control kidney function, the person finds an appropriate time and a person does control when the bladder place to urinate. A normal bladder acts empties. Bladder emptying is known as like a reservoir and can hold 1.5 to 2 cups of urine. How often a person needs to urinate depends on how quickly the kidneys Why is the urinary tract produce the urine that fills the bladder. -

Nerve Blocks for Surgery on the Shoulder, Arm Or Hand
The Association of Regional The Royal College of Anaesthetists of Great Anaesthesia – Anaesthetists Britain and Ireland United Kingdom Nerve blocks for surgery on the shoulder, arm or hand Information for patients and families www.rcoa.ac.uk/patientinfo First edition 2015 This leaflet is for anyone who is thinking about having a nerve block for an operation on the shoulder, arm or hand. It will be of particular interest to people who would prefer not to have a general anaesthetic. The leaflet has been written with the help of patients who have had a nerve block for their operation. You can find more information leaflets on the website www.rcoa.ac.uk/patientinfo. The leaflets may also be available from the anaesthetic department or pre-assessment clinic in your hospital. The website includes the following: ■ Anaesthesia explained (a more detailed booklet). ■ You and your anaesthetic (a shorter summary). ■ Your spinal anaesthetic. ■ Anaesthetic choices for hip or knee replacement. ■ Epidural pain relief after surgery. ■ Local anaesthesia for your eye operation. ■ Your child’s general anaesthetic. ■ Your anaesthetic for major surgery with planned high dependency care afterwards. ■ Your anaesthetic for a broken hip. Risks associated with your anaesthetic This is a collection of 14 articles about specific risks associated with having an anaesthetic or an anaesthetic procedure. It supplements the patient information leaflets listed above and is available on the website: www.rcoa.ac.uk/patients-and-relatives/risks. Throughout this leaflet and others in the series, we have used this symbol to highlight key facts. 2 NERVE BLOCKS FOR SURGERY ON THE SHOULDER, ARM OR HAND Brachial plexus block? The brachial plexus is the group of nerves that lies between your neck and your armpit.