Integrative Analysis of Pinin As a Prognostic Factor in Digestive Tract Cancers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino-Like Mouse Models: Tracking the Role of the Hairless Gene
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 5-2006 Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino-like Mouse Models: Tracking the Role of the Hairless Gene Yutao Liu University of Tennessee - Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Life Sciences Commons Recommended Citation Liu, Yutao, "Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino- like Mouse Models: Tracking the Role of the Hairless Gene. " PhD diss., University of Tennessee, 2006. https://trace.tennessee.edu/utk_graddiss/1824 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Yutao Liu entitled "Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino-like Mouse Models: Tracking the Role of the Hairless Gene." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the requirements for the degree of Doctor of Philosophy, with a major in Life Sciences. Brynn H. Voy, Major Professor We have read this dissertation and recommend its acceptance: Naima Moustaid-Moussa, Yisong Wang, Rogert Hettich Accepted for the Council: Carolyn R. -

Pinin (PNN) Rabbit Polyclonal Antibody – TA337687 | Origene
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA337687 Pinin (PNN) Rabbit Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: WB Recommended Dilution: WB Reactivity: Human Host: Rabbit Isotype: IgG Clonality: Polyclonal Immunogen: The immunogen for anti-PNN antibody: synthetic peptide directed towards the N terminal of human PNN. Synthetic peptide located within the following region: MAVAVRTLQEQLEKAKESLKNVDENIRKLTGRDPNDVRPIQARLLALSGP Formulation: Liquid. Purified antibody supplied in 1x PBS buffer with 0.09% (w/v) sodium azide and 2% sucrose. Note that this product is shipped as lyophilized powder to China customers. Purification: Affinity Purified Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Predicted Protein Size: 81 kDa Gene Name: pinin, desmosome associated protein Database Link: NP_002678 Entrez Gene 5411 Human Q9H307 Background: PNN is the transcriptional activator binding to the E-box 1 core sequence of the E-cadherin promoter gene; the core-binding sequence is 5'CAGGTG-3'. PNN is capable of reversing CTBP1-mediated transcription repression. Component of a splicing-dependent mul Synonyms: DRS; DRSP; memA; SDK3 Note: Immunogen Sequence Homology: Dog: 100%; Pig: 100%; Rat: 100%; Human: 100%; Mouse: 100%; Bovine: 100%; Rabbit: 100%; Zebrafish: 100%; Guinea pig: 100% This product -

Exon Junction Complexes Can Have Distinct Functional Flavours To
www.nature.com/scientificreports OPEN Exon Junction Complexes can have distinct functional favours to regulate specifc splicing events Received: 9 November 2017 Zhen Wang1, Lionel Ballut2, Isabelle Barbosa1 & Hervé Le Hir1 Accepted: 11 June 2018 The exon junction complex (EJC) deposited on spliced mRNAs, plays a central role in the post- Published: xx xx xxxx transcriptional gene regulation and specifc gene expression. The EJC core complex is associated with multiple peripheral factors involved in various post-splicing events. Here, using recombinant complex reconstitution and transcriptome-wide analysis, we showed that the EJC peripheral protein complexes ASAP and PSAP form distinct complexes with the EJC core and can confer to EJCs distinct alternative splicing regulatory activities. This study provides the frst evidence that diferent EJCs can have distinct functions, illuminating EJC-dependent gene regulation. Te Exon Junction Complex (EJC) plays a central role in post-transcriptional gene expression control. EJCs tag mRNA exon junctions following intron removal by spliceosomes and accompany spliced mRNAs from the nucleus to the cytoplasm where they are displaced by the translating ribosomes1,2. Te EJC is organized around a core complex made of the proteins eIF4A3, MAGOH, Y14 and MLN51, and this EJC core serves as platforms for multiple peripheral factors during diferent post-transcriptional steps3,4. Dismantled during translation, EJCs mark a very precise period in mRNA life between nuclear splicing and cytoplasmic translation. In this window, EJCs contribute to alternative splicing5–7, intra-cellular RNA localization8, translation efciency9–11 and mRNA stability control by nonsense-mediated mRNA decay (NMD)12–14. At a physiological level, developmental defects and human pathological disorders due to altered expression of EJC proteins show that the EJC dosage is critical for specifc cell fate determinations, such as specifcation of embryonic body axis in drosophila, or Neural Stem Cells division in the mouse8,15,16. -
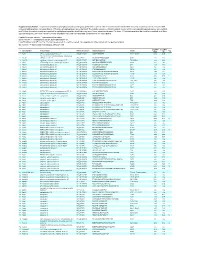
Supplementary Table 1
Supplementary Table 1. Large-scale quantitative phosphoproteomic profiling was performed on paired vehicle- and hormone-treated mTAL-enriched suspensions (n=3). A total of 654 unique phosphopeptides corresponding to 374 unique phosphoproteins were identified. The peptide sequence, phosphorylation site(s), and the corresponding protein name, gene symbol, and RefSeq Accession number are reported for each phosphopeptide identified in any one of three experimental pairs. For those 414 phosphopeptides that could be quantified in all three experimental pairs, the mean Hormone:Vehicle abundance ratio and corresponding standard error are also reported. Peptide Sequence column: * = phosphorylated residue Site(s) column: ^ = ambiguously assigned phosphorylation site Log2(H/V) Mean and SE columns: H = hormone-treated, V = vehicle-treated, n/a = peptide not observable in all 3 experimental pairs Sig. column: * = significantly changed Log 2(H/V), p<0.05 Log (H/V) Log (H/V) # Gene Symbol Protein Name Refseq Accession Peptide Sequence Site(s) 2 2 Sig. Mean SE 1 Aak1 AP2-associated protein kinase 1 NP_001166921 VGSLT*PPSS*PK T622^, S626^ 0.24 0.95 PREDICTED: ATP-binding cassette, sub-family A 2 Abca12 (ABC1), member 12 XP_237242 GLVQVLS*FFSQVQQQR S251^ 1.24 2.13 3 Abcc10 multidrug resistance-associated protein 7 NP_001101671 LMT*ELLS*GIRVLK T464, S468 -2.68 2.48 4 Abcf1 ATP-binding cassette sub-family F member 1 NP_001103353 QLSVPAS*DEEDEVPVPVPR S109 n/a n/a 5 Ablim1 actin-binding LIM protein 1 NP_001037859 PGSSIPGS*PGHTIYAK S51 -3.55 1.81 6 Ablim1 actin-binding -
Dissertation
Regulation of gene silencing: From microRNA biogenesis to post-translational modifications of TNRC6 complexes DISSERTATION zur Erlangung des DOKTORGRADES DER NATURWISSENSCHAFTEN (Dr. rer. nat.) der Fakultät Biologie und Vorklinische Medizin der Universität Regensburg vorgelegt von Johannes Danner aus Eggenfelden im Jahr 2017 Das Promotionsgesuch wurde eingereicht am: 12.09.2017 Die Arbeit wurde angeleitet von: Prof. Dr. Gunter Meister Johannes Danner Summary ‘From microRNA biogenesis to post-translational modifications of TNRC6 complexes’ summarizes the two main projects, beginning with the influence of specific RNA binding proteins on miRNA biogenesis processes. The fate of the mature miRNA is determined by the incorporation into Argonaute proteins followed by a complex formation with TNRC6 proteins as core molecules of gene silencing complexes. miRNAs are transcribed as stem-loop structured primary transcripts (pri-miRNA) by Pol II. The further nuclear processing is carried out by the microprocessor complex containing the RNase III enzyme Drosha, which cleaves the pri-miRNA to precursor-miRNA (pre-miRNA). After Exportin-5 mediated transport of the pre-miRNA to the cytoplasm, the RNase III enzyme Dicer cleaves off the terminal loop resulting in a 21-24 nt long double-stranded RNA. One of the strands is incorporated in the RNA-induced silencing complex (RISC), where it directly interacts with a member of the Argonaute protein family. The miRNA guides the mature RISC complex to partially complementary target sites on mRNAs leading to gene silencing. During this process TNRC6 proteins interact with Argonaute and recruit additional factors to mediate translational repression and target mRNA destabilization through deadenylation and decapping leading to mRNA decay. -

The Exon Junction Complex Controls Transposable Element Activity by Ensuring Faithful Splicing of the Piwi Transcript
Downloaded from genesdev.cshlp.org on September 25, 2021 - Published by Cold Spring Harbor Laboratory Press The exon junction complex controls transposable element activity by ensuring faithful splicing of the piwi transcript Colin D. Malone,1,2,5 Claire Mestdagh,3,5 Junaid Akhtar,3 Nastasja Kreim,3 Pia Deinhard,3 Ravi Sachidanandam,4 Jessica Treisman,1 and Jean-Yves Roignant3 1Kimmel Center for Biology and Medicine at the Skirball Institute of Biomolecular Medicine, Department of Cell Biology, New York Universtiy School of Medicine, New York, New York 10016, USA; 2Howard Hughes Medical Institute, 3Institute of Molecular Biology (IMB), 55128 Mainz, Germany; 4Department of Oncological Sciences, Icahn School of Medicine at Mount Sinai, New York, New York 10029, USA The exon junction complex (EJC) is a highly conserved ribonucleoprotein complex that binds RNAs during splicing and remains associated with them following export to the cytoplasm. While the role of this complex in mRNA localization, translation, and degradation has been well characterized, its mechanism of action in splicing a subset of Drosophila and human transcripts remains to be elucidated. Here, we describe a novel function for the EJC and its splicing subunit, RnpS1, in preventing transposon accumulation in both Drosophila germline and surrounding somatic follicle cells. This function is mediated specifically through the control of piwi transcript splicing, where, in the absence of RnpS1, the fourth intron of piwi is retained. This intron contains a weak polypyrimidine tract that is sufficient to confer dependence on RnpS1. Finally, we demonstrate that RnpS1-dependent removal of this intron requires splicing of the flanking introns, suggesting a model in which the EJC facilitates the splicing of weak introns following its initial deposition at adjacent exon junctions. -

Transcriptome Analysis of Different Multidrug-Resistant Gastric Carcinoma Cells
in vivo 19: 583-590 (2005) Transcriptome Analysis of Different Multidrug-resistant Gastric Carcinoma Cells STEFFEN HEIM1 and HERMANN LAGE2 1Europroteome AG, Berlin-Hennigsdorf; 2Institute of Pathology, Charité Campus Mitte, Schumannstr. 20/21, D-10117 Berlin, Germany Abstract. Multidrug resistance (MDR) of human cancers is advanced cancer. These therapeutic protocols produce an the major cause of failure of chemotherapy. To better overall response rate of about 20% at best using a single- understand the molecular events associated with the agent, and up to 50% using combination chemotherapy. development of different types of MDR, two different multidrug- Thus, a large number of malignancies are incurable. resistant gastric carcinoma cell lines, the MDR1/P-glycoprotein- Generally, gastrointestinal cancers, including gastric expressing cell line EPG85-257RDB and the MDR1/P- carcinoma, are naturally resistant to many anticancer drugs. glycoprotein-negative cell variant EPG85-257RNOV, as well as Additionally, these tumors are able to develop acquired the corresponding drug-sensitive parental cell line EPG85-257P, drug resistance phenotypes, which include the multidrug were used for analyses of the mRNA expression profiles by resistance (MDR) phenomenon. cDNA array hybridization. Of more than 12,000 genes spotted The MDR phenotype is characterized by simultaneous on the arrays, 156 genes were detected as being significantly resistance of tumor cells to various antineoplastic agents regulated in the cell line EPG85-257RDB in comparison to the which are structurally and functionally unrelated. Besides non-resistant cell variant, and 61 genes were found to be the classical MDR phenotype, mediated by the enhanced differentially expressed in the cell line EPG85-257RNOV. -

Supplementary Table S1. List of Differentially Expressed
Supplementary table S1. List of differentially expressed transcripts (FDR adjusted p‐value < 0.05 and −1.4 ≤ FC ≥1.4). 1 ID Symbol Entrez Gene Name Adj. p‐Value Log2 FC 214895_s_at ADAM10 ADAM metallopeptidase domain 10 3,11E‐05 −1,400 205997_at ADAM28 ADAM metallopeptidase domain 28 6,57E‐05 −1,400 220606_s_at ADPRM ADP‐ribose/CDP‐alcohol diphosphatase, manganese dependent 6,50E‐06 −1,430 217410_at AGRN agrin 2,34E‐10 1,420 212980_at AHSA2P activator of HSP90 ATPase homolog 2, pseudogene 6,44E‐06 −1,920 219672_at AHSP alpha hemoglobin stabilizing protein 7,27E‐05 2,330 aminoacyl tRNA synthetase complex interacting multifunctional 202541_at AIMP1 4,91E‐06 −1,830 protein 1 210269_s_at AKAP17A A‐kinase anchoring protein 17A 2,64E‐10 −1,560 211560_s_at ALAS2 5ʹ‐aminolevulinate synthase 2 4,28E‐06 3,560 212224_at ALDH1A1 aldehyde dehydrogenase 1 family member A1 8,93E‐04 −1,400 205583_s_at ALG13 ALG13 UDP‐N‐acetylglucosaminyltransferase subunit 9,50E‐07 −1,430 207206_s_at ALOX12 arachidonate 12‐lipoxygenase, 12S type 4,76E‐05 1,630 AMY1C (includes 208498_s_at amylase alpha 1C 3,83E‐05 −1,700 others) 201043_s_at ANP32A acidic nuclear phosphoprotein 32 family member A 5,61E‐09 −1,760 202888_s_at ANPEP alanyl aminopeptidase, membrane 7,40E‐04 −1,600 221013_s_at APOL2 apolipoprotein L2 6,57E‐11 1,600 219094_at ARMC8 armadillo repeat containing 8 3,47E‐08 −1,710 207798_s_at ATXN2L ataxin 2 like 2,16E‐07 −1,410 215990_s_at BCL6 BCL6 transcription repressor 1,74E‐07 −1,700 200776_s_at BZW1 basic leucine zipper and W2 domains 1 1,09E‐06 −1,570 222309_at -

WO 2013/064702 A2 10 May 2013 (10.05.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2013/064702 A2 10 May 2013 (10.05.2013) P O P C T (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, C12Q 1/68 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/EP2012/071868 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 5 November 20 12 (05 .11.20 12) NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, (25) Filing Language: English TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (26) Publication Language: English ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 1118985.9 3 November 201 1 (03. 11.201 1) GB kind of regional protection available): ARIPO (BW, GH, 13/339,63 1 29 December 201 1 (29. 12.201 1) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (71) Applicant: DIAGENIC ASA [NO/NO]; Grenseveien 92, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, N-0663 Oslo (NO). -

Datasheet A01590-2 Anti-PNN/DRSP Antibody
Product datasheet Anti-PNN/DRSP Antibody Catalog Number: A01590-2 BOSTER BIOLOGICAL TECHNOLOGY Special NO.1, International Enterprise Center, 2nd Guanshan Road, Wuhan, China Web: www.boster.com.cn Phone: +86 27 67845390 Fax: +86 27 67845390 Email: [email protected] Basic Information Product Name Anti-PNN/DRSP Antibody Gene Name PNN Source Rabbit IgG Species Reactivity human,mouse,rat Tested Application WB,FCM,Direct ELISA Contents 500ug/ml antibody with PBS ,0.02% NaN3 , 1mg BSA Immunogen E.coli-derived human PNN/DRSP recombinant protein (Position: A2-L241). Purification Immunogen affinity purified. Observed MW 82KD Dilution Ratios Western blot: 1:500-2000 Flow cytometry (FCM): 1-3μg/1x106 cells Direct ELISA: 1:100-1000 Storage 12 months from date of receipt,-20℃ as supplied.6 months 2 to 8℃ after reconstitution. Avoid repeated freezing and thawing Background Information Pinin is a protein that in humans is encoded by the PNN gene. By yeast 2-hybrid analysis of HeLa cells, followed by sequence analysis, it was found that epitope-tagged human PNN interacted with the serine/arginine (SR)-rich proteins SRP75 (SRSF4; 601940), SRM300 (SRRM2; 606032), and SRRP130 (PNISR; 616653). Truncation analysis revealed that the polyserine/RS domain of PNN and flanking sequences participated in binding to these SR proteins. The 4 proteins colocalized in the nucleus of HCE-T cells, and overexpression of any of these proteins affected the distribution of the others between nuclear speckles and nucleoplasm. Reference Anti-PNN/DRSP Antibody被引用在0文献中。 暂无引用 1 / 2 Product datasheet Anti-PNN/DRSP Antibody Catalog Number: A01590-2 BOSTER BIOLOGICAL TECHNOLOGY Special NO.1, International Enterprise Center, 2nd Guanshan Road, Wuhan, China Web: www.boster.com.cn Phone: +86 27 67845390 Fax: +86 27 67845390 Email: [email protected] Selected Validation Data Figure 1. -

ATA35521-Pinin Rabbit Polyclonal Antibody
ATAGENIX LABORATORIES Catalog Number:ATA35521 Pinin rabbit Polyclonal Antibody 产品概述 产品名(Product Name) Pinin rabbit Polyclonal Antibody 货号(Catalog No.) ATA35521 宿主(Host) Rabbit 反应种属(Species specificity) Human,Mouse 应用实验(Tested applications) WB,ELISA 克隆性(Clonality) Polyclonal 免疫原(Immunogen) The antiserum was produced against synthesized peptide derived from human PNN. AA range:211-260 产品性能 状态(Form) Liquid 存放条件(Storage) Use a manual defrost freezer and avoid repeated freeze thaw cycles. Store at 4 °C for frequent use. Store at -20 to -80 °C for twelve months from the date of receipt. 纯化方式(Purity) The antibody was affinity-purified from rabbit antiserum by affinity-chromatography using epitope-specific immunogen. 应用 Western Blot: 1/500 - 1/2000. ELISA: 1/20000. Not yet tested in other applications. 产品背景 function:Transcriptional activator binding to the E-box 1 core sequence of the E-cadherin promoter gene; the core-binding sequence is 5'CAGGTG-3'. Capable of reversing CTBP1-mediated transcription repression. Also participates in the regulation of alternative pre-mRNA splicing. Associates to spliced mRNA within 60 nt upstream of the 5'-splice sites. Involved in the establishment and maintenance of epithelia cell-cell adhesion. Potential tumor suppressor for renal cell carcinoma.,PTM: Phosphorylated upon DNA damage, probably by ATM or ATR.,similarity:Belongs to the pinin family.,subcellular location:Cell- cell contact area, predominantly desmosome of intercellular adherens junction. Not a nucleocytoplasmic shuttling protein., subunit:Found in a complex with SR proteins. Found in a mRNP complex with RNPS1. Interacts with C6orf111/SRRP130, CTBP1, CTBP2, KRT8, KRT18, KRT19, PS1D/PNO40, PPIG, RNPS1, SFRS4 and SRRM2. -

Program in Human Neutrophils Fails To
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 is online at: average * The Journal of Immunology Anaplasma phagocytophilum , 20 of which you can access for free at: 2005; 174:6364-6372; ; from submission to initial decision 4 weeks from acceptance to publication J Immunol doi: 10.4049/jimmunol.174.10.6364 http://www.jimmunol.org/content/174/10/6364 Insights into Pathogen Immune Evasion Mechanisms: Fails to Induce an Apoptosis Differentiation Program in Human Neutrophils Dori L. Borjesson, Scott D. Kobayashi, Adeline R. Whitney, Jovanka M. Voyich, Cynthia M. Argue and Frank R. DeLeo cites 28 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2005/05/03/174.10.6364.DC1 This article http://www.jimmunol.org/content/174/10/6364.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* • Why • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2005 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 25, 2021. The Journal of Immunology Insights into Pathogen Immune Evasion Mechanisms: Anaplasma phagocytophilum Fails to Induce an Apoptosis Differentiation Program in Human Neutrophils1 Dori L.