CHAPTER 11 General and Local Anesthetics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Liposomal Delivery System for Topical Anesthesia
THERAPEUTICS FOR THE CLINICIAN Evaluation of Liposomal Delivery System for Topical Anesthesia Mohamed L. Elsaie, MD, MBA; Leslie S. Baumann, MD Local anesthesia is an integral aspect of cutane- infiltrative anesthetics, now can be accomplished ous surgery. Its effects provide a reversible loss safely and comfortably with the use of topi- of sensation in a limited area of skin, allowing cal anesthetics.1 Topical anesthetics originated in dermatologists to perform diagnostic and thera- South America; native Peruvians noted perioral peutic procedures safely, with minimal discomfort numbness when chewing the leaf of the cocoa plant and risk to the patient. Moreover, the skin acts (Erythroxylon coca). The active alkaloid, cocaine, was as a major target as well as principle barrier for isolated by Niemann in 1860 and applied to con- topical/transdermal (TT) drug delivery. The stra- junctival mucosa for topical anesthesia by Koller in tum corneum (SC) plays a crucial role in barrier 1884. The development of similar benzoic acid esters function for TT drug delivery. Despite the major continued until 1943 when Loefgren synthesized lido- research and development efforts in TT systems caine hydrochloride, the first amide anesthetic.2 and their implementation for use of topical anes- We review the administration of local anes- thetics, low SC permeability limits the useful- thetics, specifically the liposomal delivery system ness of topical delivery, which has led to other for topical anesthesia, based on a review of the delivery system developments, including vesicu- literature and clinical experience. lar systems such as liposomes, niosomes, and proniosomes, with effectiveness relying on their Anatomy physiochemical properties. -

Prolonged Duration Topical Corneal Anesthesia with the Cationic Lidocaine Derivative QX-314
https://doi.org/10.1167/tvst.8.5.28 Article Prolonged Duration Topical Corneal Anesthesia With the Cationic Lidocaine Derivative QX-314 Alan G. Woodruff1,2, Claudia M. Santamaria1, Manisha Mehta1,2, Grant L. Pemberton1, Kathleen Cullion1,2,4, and Daniel S. Kohane1,2,3 1 Kohane Lab for Biomaterials and Drug Delivery, Department of Anesthesia, Perioperative and Pain Medicine, Division of Critical Care, Boston Children’s Hospital, Boston, MA, USA 2 Harvard Medical School, Boston, MA, USA 3 David H. Koch Institute, Massachusetts Institute of Technology, Cambridge, MA, USA 4 Department of Medicine, Division of Medicine Critical Care, Boston Children’s Hospital, Harvard Medical School, Boston, MA, USA Correspondence: Daniel S. Kohane, Purpose: Topical corneal local anesthetics are short acting and may impair corneal Laboratory for Biomaterials and healing. In this study we compared corneal anesthesia and toxicity of topically applied Drug Delivery, Department of Anes- N-ethyl lidocaine (QX-314) versus the conventional local anesthetic, proparacaine thesia, Division of Critical Care (PPC). Medicine, Boston Children’s Hospi- tal, Harvard Medical School, 61 Methods: Various concentrations of QX-314 and 15 mM (0.5%) PPC were topically Binney Street, Room 361, Boston, applied to rat corneas. Corneal anesthesia was assessed with a Cochet-Bonnet MA 02115, USA. e-mail: Daniel. esthesiometer at predetermined time points. PC12 cells were exposed to the same [email protected] solutions to assess cytotoxicity. Repeated topical corneal administration in rats was then used to assess for histologic evidence of toxicity. Finally, we created uniform Received: 6 May 2019 corneal epithelial defects in rats and assessed the effect of repeated administration of Accepted: 15 August 2019 these compounds on the defect healing rate. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -
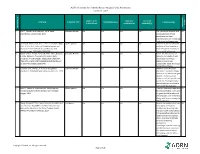
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures
Volume 2- Issue 1 : 2018 DOI: 10.26717/BJSTR.2018.02.000695 Eduardo de Oliveira Duque-Estrada. Biomed J Sci & Tech Res ISSN: 2574-1241 Mini Review Open Access The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures Eduardo de Oliveira Duque-Estrada MD* Received: January 17, 2018; Published: January 25, 2018 *Corresponding author: Eduardo de Oliveira Duque-Estrada, Ex-Professor of Pediatrics and Pediatric Surgery, Teresópolis Schoolof Medicine, Rio de Janeiro, Rua Jose da Silva Ribeiro 119 apt 11 São Paulo, SP Brazil CEP: 05726-130, Email: Abstract The local anesthetics are widely u sed in minor pediatric surgical procedures. The major problem with their use is the resulted pain experienced by the patients at the time of injection. To discuss those situations in the light of the medical literature we present this mini-review. Key words: Local Injection; Pain; Buffer; pH; Lidocaine; Pediatric Surgery Procedure Introduction Table 1: Techniques for injection pain control*. a eutectic mixture of lidocaine and prilocaine (EMLA) cream [17] S.No Techniques for injection pain control before infiltration, and local external cooling (cryoanalgesia) have 1. Warming the anesthetic solution [18,19] (Table 1). also been used to reduce the pain of infiltration of local anesthetic 2. Buffering the anesthetic Buffering the Anesthetic 3. Injection technique 4. Distraction Local anesthesia is extremely useful either as the sole method the best results on the minor surgery in general [3,6]. Blocking 5. Combination anesthetic technique the pain pathway with local anesthetic solution will also reduce 6. Cooling of skin the family stress response to the surgical procedure. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC). -

Safety Alert: Risks Associated with Ophthalmic Anesthetics
WRHA Pharmacy Program Health Sciences Centre MS-189 820 Sherbrook St. Winnipeg, Manitoba R3A 1R9 CANADA TEL: 204-787-7183 Fax: 204-787-3195 FAX: 204-787-3195 Safety Alert: Risks associated with Ophthalmic Anesthetics The self-administration of ophthalmic anesthetics by patients for the relief of eye pain should be avoided and they should not be given to patients to take home for pain relief. Vision threatening complications of topical anesthetic abuse are common. There is no indication for the use of ophthalmic anesthetics except for diagnostic and short term therapeutic purposes (the removal of a foreign body or ocular surgery) and therefore, these products should only be used under a physician’s supervision. Eye trauma resulting in a corneal abrasion (epithelial injury) is a common complaint in the Emergency department (1). A superficial corneal injury can cause intense pain causing a patient to seek medical help or immediate relief from available over the counter remedies. In Canada, only two topical ophthalmic anesthetic drugs are available commercially as single entities, proparacaine (proxymetacaine) and tetracaine (available in bottle and minim forms). Benoxinate (oxybuprocaine) is only available in combination with fluorescein (3). Lidocaine is also used in ophthalmic surgical procedures however, it is not available in the Canadian market as an ophthalmic preparation. Topical ophthalmic anesthetics function by blocking nerve conduction when applied to the cornea and conjunctiva. The ocular surface is innervated by the multiple branches of the trigeminal nerve. The cornea is supplied by the long and short ciliary nerves, the nasociliary nerve and the lacrimal nerve (4). Topical anesthetics reduce sodium permeability preventing generation and conduction of nerve impulses, increasing excitation threshold, and slowing the nerve impulse propagation. -
Local Anesthesia for Carpal Tunnel Surgery
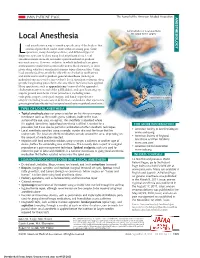
JAMA PATIENT PAGE The Journal of the American Medical Association ANESTHESIOLOGY Administration of local anesthetic Local Anesthesia for carpal tunnel surgery ocal anesthesia is a way to numb a specific area of the body so that a medical procedure can be done without causing pain. Some Loperations, many dental procedures, and different types of diagnostic tests can be done using local anesthesia alone. Local anesthesia medications do not make a person sedated or produce unconsciousness. However, sedation, in which individuals are given medications to make them comfortable and to block memory, is often given along with local anesthesia for many types of procedures. Using local anesthesia alone avoids the side effects of sedation medications and medications used to produce general anesthesia (making an individual unconscious for a procedure). Local anesthetic solutions often provide long-lasting pain relief to the area where they have been applied. Many operations, such as appendectomy (removal of the appendix), cholecystectomy (removal of the gallbladder), and open heart surgery, require general anesthesia. Other procedures, including some orthopedic surgery, urological surgery, and female reproductive Carpal tunnel surgery surgery (including most cesarean deliveries), can be done after a person is given regional anesthesia (such as spinal anesthesia or epidural anesthesia). TYPES OF LOCAL ANESTHESIA • Topical anesthesia places or sprays a solution on the skin or a mucous membrane (such as the mouth, gums, eardrum, inside of the nose, surface of the eye, anus, or vagina). The anesthetic is absorbed where it is applied. Sometimes topical local anesthesia is all that is needed for a FOR MORE INFORMATION procedure, but it can also be part of a combination of other anesthetic techniques. -

Veterinary Anesthesia and Pain Management Secrets / Edited by Stephen A
Publisher: HANLEY & BELFUS, INC. Medical Publishers 210 South 13th Street Philadelphia, PA 19107 (215) 546-7293; 800-962-1892 FAX (215) 790-9330 Web site: http://www.hanleyandbelfus.com Note to the reader Although the information in this book has been carefully reviewed for cor rectness of dosage and indications, neither the authors nor the editor nor the publisher can accept any legal responsibility for any errors or omissions that may be made. Neither the publisher nor the editor makes any warranty, expressed or implied, with respect to the material contained herein. Before prescribing any drug. the reader must review the manu facturer's correct product information (package inserts) for accepted indications, absolute dosage recommendations. and other information pertinent to the safe and effective use of the product described. This is especially important when drugs are given in combination or as an adjunct to other forms of therapy Library of Congress Cataloging-in-Publication Data Veterinary anesthesia and pain management secrets / edited by Stephen A. Greene. p. em. - (The Secrets Series®) Includes bibliographical references (p.). ISBN 1-56053-442-7 (alk paper) I. Veterinary anesthesia-Examinations, questions. etc. 2. Pain in animals Treatment-Examinations, questions, etc. I. Greene, Stephen A., 1956-11. Series. SF914.V48 2002 636 089' 796'076--dc2 I 2001039966 VETERINARY ANESTHESIA AND PAIN MANAGEMENT SECRETS ISBN 1-56053-442-7 © 2002 by Hanley & Belfus, Inc. All rights reserved. No part of this book may be repro duced, reused, republished. or transmitted in any form, or stored in a database or retrieval system, without written permission of the publisher Last digit is the print number: 9 8 7 6 5 4 3 2 CONTRIBUTORS G. -

Local Anesthetic Agents Infiltration: Role of the Nurse
Doug Ducey Joey Ridenour Governor Executive Director Arizona State Board of Nursing 1740 W Adams Street, Suite 2000 Phoenix. AZ 85007 Phone (602) 771-7800 Home Page: http://www.azbn.gov OPINION: INFILTRATION OF LOCAL An advisory opinion adopted by AZBN is an interpretation of what the law requires. While an ANESTHETIC AGENTS: THE ROLE OF THE advisory opinion is not law, it is more than a recommendation. In other words, an advisory opinion NURSE is an official opinion of AZBN regarding the practice of nursing as it relates to the functions of APPROVED DATE: 3/2015 nursing. Facility policies may restrict practice further in their setting and/or require additional REVISED DATE: 7/2018 expectations related to competency, validation, training, and supervision to assure the safety of their patient population and or decrease risk. ORIGINATING COMMITTEE: SCOPE OF PRACTICE COMMITTEE Within the Scope of Practice of X RN x LPN ADVISORY OPINION LOCAL ANESTHETIC AGENTS INFILTRATION: ROLE OF THE NURSE It is within the scope of practice of a registered nurse (RN) and a licensed practical nurse (LPN) to administer certain local anesthetic agents intradermal, subcutaneous, and submucosal for the purposes of analgesia and/or anesthesia prior to potentially painful procedures. Tumescent lidocaine infiltration for ambulatory procedures, such as but not limited to, the treatment of hyperhidrosis, ambulatory phlebectomy and laser facial resurfacings would be within the RN scope under the direction of an licensed independent practitioner (LIP) and when certain criteria is met within this advisory opinion. The licensed nurse must meet the general requirements and course of instruction listed in parts I and II. -

Script For: Local Anesthetic Agents Surgery 101 Podcast Department of Surgery University of Alberta
Script for: Local Anesthetic Agents Surgery 101 Podcast Department of Surgery University of Alberta By Urooj Siddiqui Med 4 University of Alberta Hello, and welcome to another episode of Surgery 101. My name is Urooj Siddiqui, and I am pleased to be serving as a guest host this week! I am a fourth year University of Alberta Medical student just recently finishing an anesthesia elective here at the UofA. I’d like to recognize and thank Dr. Ronald Cheng for his input and feedback on this podcast. The objectives of this podcast are to: • Describe the pharmacology of local anesthetics • Look at the different types of local anesthetics • Highlight the different techniques used in local anesthesia • Outline the toxicities associated with common local anesthetic agents • Recognize the indications for and against the use of local anesthetics How many of you have ever had to get stitches, a tooth pulled or a small lump removed? Needless to say these would all be very painful procedures were it not for some local anesthetic. When applied to nerves, local anesthetics block the generation and propagation of action potentials. This essentially induces an absence of sensation in the nerve's distribution distal to the point of application. In regional anesthesia, local anesthetics are applied to large nerves or near the spinal cord to provide diminished sensation to a large area – such as a limb or lower segment of the body. If a small discrete portion of the body (i.e. tooth or incision/laceration) needs to be "frozen", the local anesthetics are applied more distally. -

Important Clinical Factors Related to Local Anesthesia
ENDODONTICS: Colleagues for Excellence Winter 2009 Bonus Material A IMPORTANT CLINICAL FACTORS RELATED TO LOCAL ANESTHESIA Before reviewing the specifics of local anesthesia, we would like to provide an overview of some factors that are important to clinical anesthesia. How do we traditionally confirm anesthesia clinically? Traditional methods to confirm anesthesia usually involve questioning the patient (“Is your lip numb?ʺ), soft tissue testing (e.g., lack of mucosal responsiveness to a sharp explorer) or simply commencing with treatment. The problem with these approaches is they may not be effective for determining pulpal anesthesia.1‐4 Objective means of determining pulpal anesthesia in nonpainful, vital teeth. A more objective measurement of anesthesia, in nonpainful vital teeth, is obtained with an application of a cold refrigerant or by using an electric pulp tester. Clinically, application of cold or the electric pulp tester can be used to test the tooth under treatment for pulpal anesthesia prior to beginning a clinical procedure.5‐10 Determining pulpal anesthesia in painful, vital teeth. However, in painful, vital teeth (e.g., irreversible pulpitis), the lack of response to pulp testing may not guarantee pulpal anesthesia even if there is vital tissue present in the pulp chamber.5, 9, 10 Therefore, if a patient experiences pain when the endodontic procedure is started, after negative pulp testing, supplemental anesthesia is indicated. Naturally, if the chamber is necrotic and the canals are vital, no objective test can predict the level of clinical anesthesia. However, as suggested by Hsiao‐Wu, et al.10, cold testing adjacent teeth for anesthesia may provide evidence of anesthesia in the working area.