Anesthesiology Primer for SIU Medical Students
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Product Catalog POLICIES Ordering Options Payment Methods
Product Catalog POLICIES Ordering Options Payment Methods Three Easy Ways To Order Payment Portal and ACH Visit www.sunsethcs.com/paymentportal to pay online with Phone ACH or credit card. (877) 5-SUNSET (877-578-6738) Our customer service professionals are here to assist you Net 30-Day Payment Terms M-F 8:00 AM – 5:00 PM Central Time. For qualified companies. A 1.5% monthly finance charge will be assessed on all past due invoices. Fax 312-997-9985 — Accepted 24 hours a day. COD For non-qualified companies. Email [email protected] Credit Card We accept all major credit cards. A processing fee may apply. After 10 days of invoice date, a surcharge of 2.5% will be applied. Shipping Customer Service Drop shipping available — ask your sales rep Returns about sending your order to multiple locations. Call us for a return authorization number. There is no restocking charge on orders returned within 20 days of UPS invoice. Orders returned after 20 days may be assessed a Whenever possible, orders ship via UPS. If another carrier restocking fee of 15%. No returns after 90 days. is desired, please contact your sales rep. (877) 5-SUNSET (877-578-6738) All orders are packed in the smallest boxes available and Central Distribution Center Western Distribution Center combined with other products on the order to reduce Sunset Healthcare Solutions Sunset Healthcare Solutions shipping costs. 279 Madsen Dr Ste 101 2450 Statham Blvd Bloomingdale, IL 60108 Oxnard, CA 93033 All products ship prepaid and are added to the invoice. Problems All products ship from Bloomingdale, IL or Oxnard, CA. -

Oxymask™ Empower Best Practice
OxyMask™ Empower Best Practice. Safer Care. Exceptional Experience. Clinical Evidence Summary Executive Summary OxyMask is a solution for safer, more efficient oxygen delivery. It is an all-in-one replacement for other oxygen delivery modalities, such as the venturi mask and non-rebreather mask. The unique OxyMask technology helps enhance patient experience, increase efficiency, and reduce costs. Introduction: Enhance Patient Experience In an ever-competitive healthcare market, patient experience is at the forefront of advances in healthcare. Patients treated with oxygen therapy may feel they are trapped or helpless.1 Patient-centered solutions are increasingly recommended in policy and research.2 OxyMask brings patient-centered care to fruition through its design and dependability. Patient-centered design OxyMask utilizes a light-weight, open design that: • Sits lightly on the face • Allows unrestricted communication • Allows for oral medication delivery • May reduce the feeling of claustrophobia Dependability OxyMask is clinically proven to deliver more oxygen at lower flow rates compared to traditional delivery methods.3 Additionally, laboratory testing suggests that OxyMask reduces the risk of carbon dioxide rebreathing when compared to non-rebreather masks.4,5 OxyMask™ OxyMask Delivers Oxygen More Efficiently OxyMask May Reduce the Risk of Carbon Than a Venturi Mask3 Dioxide Rebreathing Compared to a Beecroft JM, Hanly PJ. Comparison of the OxyMask and Venturi mask in the Non-Rebreather Mask4 delivery of supplemental oxygen: Pilot study in oxygen-dependent patients. Can Respir J. 2006;13(5):247-252. Lamb K, Piper D. Southmedic OxyMaskTM compared with the Hudson RCI® Non-Rebreather Mask™: Safety and performance comparison. Can J Resp Ther. -

Evaluation of Liposomal Delivery System for Topical Anesthesia
THERAPEUTICS FOR THE CLINICIAN Evaluation of Liposomal Delivery System for Topical Anesthesia Mohamed L. Elsaie, MD, MBA; Leslie S. Baumann, MD Local anesthesia is an integral aspect of cutane- infiltrative anesthetics, now can be accomplished ous surgery. Its effects provide a reversible loss safely and comfortably with the use of topi- of sensation in a limited area of skin, allowing cal anesthetics.1 Topical anesthetics originated in dermatologists to perform diagnostic and thera- South America; native Peruvians noted perioral peutic procedures safely, with minimal discomfort numbness when chewing the leaf of the cocoa plant and risk to the patient. Moreover, the skin acts (Erythroxylon coca). The active alkaloid, cocaine, was as a major target as well as principle barrier for isolated by Niemann in 1860 and applied to con- topical/transdermal (TT) drug delivery. The stra- junctival mucosa for topical anesthesia by Koller in tum corneum (SC) plays a crucial role in barrier 1884. The development of similar benzoic acid esters function for TT drug delivery. Despite the major continued until 1943 when Loefgren synthesized lido- research and development efforts in TT systems caine hydrochloride, the first amide anesthetic.2 and their implementation for use of topical anes- We review the administration of local anes- thetics, low SC permeability limits the useful- thetics, specifically the liposomal delivery system ness of topical delivery, which has led to other for topical anesthesia, based on a review of the delivery system developments, including vesicu- literature and clinical experience. lar systems such as liposomes, niosomes, and proniosomes, with effectiveness relying on their Anatomy physiochemical properties. -

Femoral and Sciatic Nerve Blocks for Total Knee Replacement in an Obese Patient with a Previous History of Failed Endotracheal Intubation −A Case Report−
Anesth Pain Med 2011; 6: 270~274 ■Case Report■ Femoral and sciatic nerve blocks for total knee replacement in an obese patient with a previous history of failed endotracheal intubation −A case report− Department of Anesthesiology and Pain Medicine, School of Medicine, Catholic University of Daegu, Daegu, Korea Jong Hae Kim, Woon Seok Roh, Jin Yong Jung, Seok Young Song, Jung Eun Kim, and Baek Jin Kim Peripheral nerve block has frequently been used as an alternative are situations in which spinal or epidural anesthesia cannot be to epidural analgesia for postoperative pain control in patients conducted, such as coagulation disturbances, sepsis, local undergoing total knee replacement. However, there are few reports infection, immune deficiency, severe spinal deformity, severe demonstrating that the combination of femoral and sciatic nerve blocks (FSNBs) can provide adequate analgesia and muscle decompensated hypovolemia and shock. Moreover, factors relaxation during total knee replacement. We experienced a case associated with technically difficult neuraxial blocks influence of successful FSNBs for a total knee replacement in a 66 year-old the anesthesiologist’s decision to perform the procedure [1]. In female patient who had a previous cancelled surgery due to a failed tracheal intubation followed by a difficult mask ventilation for 50 these cases, peripheral nerve block can provide a good solution minutes, 3 days before these blocks. FSNBs were performed with for operations on a lower extremity. The combination of 50 ml of 1.5% mepivacaine because she had conditions precluding femoral and sciatic nerve blocks (FSNBs) has frequently been neuraxial blocks including a long distance from the skin to the used for postoperative pain control after total knee replacement epidural space related to a high body mass index and nonpalpable lumbar spinous processes. -

Prolonged Duration Topical Corneal Anesthesia with the Cationic Lidocaine Derivative QX-314
https://doi.org/10.1167/tvst.8.5.28 Article Prolonged Duration Topical Corneal Anesthesia With the Cationic Lidocaine Derivative QX-314 Alan G. Woodruff1,2, Claudia M. Santamaria1, Manisha Mehta1,2, Grant L. Pemberton1, Kathleen Cullion1,2,4, and Daniel S. Kohane1,2,3 1 Kohane Lab for Biomaterials and Drug Delivery, Department of Anesthesia, Perioperative and Pain Medicine, Division of Critical Care, Boston Children’s Hospital, Boston, MA, USA 2 Harvard Medical School, Boston, MA, USA 3 David H. Koch Institute, Massachusetts Institute of Technology, Cambridge, MA, USA 4 Department of Medicine, Division of Medicine Critical Care, Boston Children’s Hospital, Harvard Medical School, Boston, MA, USA Correspondence: Daniel S. Kohane, Purpose: Topical corneal local anesthetics are short acting and may impair corneal Laboratory for Biomaterials and healing. In this study we compared corneal anesthesia and toxicity of topically applied Drug Delivery, Department of Anes- N-ethyl lidocaine (QX-314) versus the conventional local anesthetic, proparacaine thesia, Division of Critical Care (PPC). Medicine, Boston Children’s Hospi- tal, Harvard Medical School, 61 Methods: Various concentrations of QX-314 and 15 mM (0.5%) PPC were topically Binney Street, Room 361, Boston, applied to rat corneas. Corneal anesthesia was assessed with a Cochet-Bonnet MA 02115, USA. e-mail: Daniel. esthesiometer at predetermined time points. PC12 cells were exposed to the same [email protected] solutions to assess cytotoxicity. Repeated topical corneal administration in rats was then used to assess for histologic evidence of toxicity. Finally, we created uniform Received: 6 May 2019 corneal epithelial defects in rats and assessed the effect of repeated administration of Accepted: 15 August 2019 these compounds on the defect healing rate. -

Dexmedetomidine During Suprazygomatic Maxillary Nerve Block for Pediatric Cleft Palate Repair, Randomized Double-Blind Controlled Study Mohamed F
Korean J Pain 2020;33(1):81-89 https://doi.org/10.3344/kjp.2020.33.1.81 pISSN 2005-9159 eISSN 2093-0569 Original Article Dexmedetomidine during suprazygomatic maxillary nerve block for pediatric cleft palate repair, randomized double-blind controlled study Mohamed F. Mostafa1, Fatma A. Abdel Aal1, Ibrahim Hassan Ali1, Ahmed K. Ibrahim2, and Ragaa Herdan1 1Department of Anesthesia and Intensive Care, Faculty of Medicine, Assiut University, Assiut, Egypt 2Department of Public Health, Faculty of Medicine, Assiut University, Assiut, Egypt Received July 26, 2019 Revised December 3, 2019 Background: For children with cleft palates, surgeries at a young age are necessary Accepted December 3, 2019 to reduce feeding or phonation difficulties and reduce complications, especially respiratory tract infections and frequent sinusitis. We hypothesized that dexmedeto- Correspondence midine might prolong the postoperative analgesic duration when added to bupiva- Mohamed F. Mostafa caine during nerve blocks. Department of Anesthesia and Intensive Methods: Eighty patients of 1-5 years old were arbitrarily assigned to two equal Care, Assiut University Hospital, Faculty groups (forty patients each) to receive bilateral suprazygomatic maxillary nerve of Medicine, Assiut University, Assiut blocks. Group A received bilateral 0.2 mL/kg bupivacaine (0.125%; maximum vol- 71515, Egypt Tel: +20-1001123062 ume 4 mL/side). Group B received bilateral 0.2 mL/kg bupivacaine (0.125%) + 0.5 Fax: +20-88-2333327 μg/kg dexmedetomidine (maximum volume 4 mL/side). E-mail: [email protected] Results: The modified children’s hospital of Eastern Ontario pain scale score was significantly lower in group B children after 8 hours of follow-up postoperatively (P < 0.001). -

Moderate Sedation
MODERATE SEDATION A SELF STUDY GUIDE Part I Self Study Guide Part II ASA Practice Guidelines for Sedation And Analgesia by Non-Anesthesiologists Part III Sedation/Analgesia Policy 1 Introduction Diagnostic and surgical procedures are being performed in a variety of settings throughout the hospital. This self-study program has been developed to increase your awareness and reinforce your understanding of the use of moderate sedation. It includes indications/contraindications for moderate sedation, accepted medications administration guidelines, and monitoring requirements. Part I is dedicated to an overall review of the principles of moderate sedation, Part II includes the American Society of Anesthesiology’s Practice Guidelines For Sedation And Analgesia by Non- Anesthesiologist. Part 3 is a post-test. Completion of this self-study packet includes learning the following material, satisfactory completion of the post-test and returning the post-test to the Medical Staff Office. Completion of this self-study is required to qualify for privileges to administer Moderate Sedation at St. David’s Medical Center. Purpose The purpose of this self-study packet is to increase and reinforce your knowledge of responsibilities and guidelines associated with the care of individuals requiring moderate sedation. On completion of this self-study program, you should be able to: 1. Recognize indications and contraindication for moderate sedation. 2. State appropriate monitoring techniques and requirements for patients undergoing moderate sedation. 3. Identify medications frequently used for moderate sedation, administration guidelines, and potential complications/side-effects. 4. Evaluate and manage expected and unexpected outcomes of moderate sedation Part I Definition Conscious Sedation more accurately termed Sedation/Analgesia or Moderate Sedation describes a state that allows patients to tolerate unpleasant procedures while maintaining adequate cardiorespiratory function and the ability to respond purposefully to verbal commands and tactile stimulation. -

Safety Alert: Risks Associated with Ophthalmic Anesthetics
WRHA Pharmacy Program Health Sciences Centre MS-189 820 Sherbrook St. Winnipeg, Manitoba R3A 1R9 CANADA TEL: 204-787-7183 Fax: 204-787-3195 FAX: 204-787-3195 Safety Alert: Risks associated with Ophthalmic Anesthetics The self-administration of ophthalmic anesthetics by patients for the relief of eye pain should be avoided and they should not be given to patients to take home for pain relief. Vision threatening complications of topical anesthetic abuse are common. There is no indication for the use of ophthalmic anesthetics except for diagnostic and short term therapeutic purposes (the removal of a foreign body or ocular surgery) and therefore, these products should only be used under a physician’s supervision. Eye trauma resulting in a corneal abrasion (epithelial injury) is a common complaint in the Emergency department (1). A superficial corneal injury can cause intense pain causing a patient to seek medical help or immediate relief from available over the counter remedies. In Canada, only two topical ophthalmic anesthetic drugs are available commercially as single entities, proparacaine (proxymetacaine) and tetracaine (available in bottle and minim forms). Benoxinate (oxybuprocaine) is only available in combination with fluorescein (3). Lidocaine is also used in ophthalmic surgical procedures however, it is not available in the Canadian market as an ophthalmic preparation. Topical ophthalmic anesthetics function by blocking nerve conduction when applied to the cornea and conjunctiva. The ocular surface is innervated by the multiple branches of the trigeminal nerve. The cornea is supplied by the long and short ciliary nerves, the nasociliary nerve and the lacrimal nerve (4). Topical anesthetics reduce sodium permeability preventing generation and conduction of nerve impulses, increasing excitation threshold, and slowing the nerve impulse propagation. -

How to Deliver Aerosolized Medications Through High Flow Nasal Cannula Safely and Effectively in the Era of COVID-19 and Beyond: a Narrative Review
NARRATIVE REVIEW How to deliver aerosolized medications through high flow nasal cannula safely and effectively in the era of COVID-19 and beyond: A narrative review Arzu Ari, PhD, RRT, PT, CPFT, FAARC, FCCP1, Gerald B. Moody, BSRC, RRT-NPS2 A Ari, GB Moody. How to deliver aerosolized medications through high flow nasal cannula safely and effectively in the era of COVID-19 and beyond: A narrative review. Can J Respir Ther 2021;57:22–25. doi: 10.29390/cjrt-2020-041. Background: The treatments of COVID-19 involve some degree of uncertainty. Current evidence also shows mixed findings with regards to bioaerosol dispersion and airborne transmission of COVID-19 during high flow nasal cannula (HFNC) therapy. While coping with this global pandemic created hot debates on the use of HFNC, it is important to bring detached opinions and current evidence to the attention of health care professionals (HCPs) who may need to use HFNC in patients with COVID-19. Aim: The purpose of this paper is to provide a framework on the selection, placement, and use of nebulizers as well as HFNC prongs, gas flow, and delivery technique via HFNC to help clinicians deliver aerosolized medications through HFNC safely and effectively in the era of COVID-19 and beyond. Methods: We searched PubMed, Medline, CINAHL, and Science Direct to identify studies on aerosol drug delivery through HFNC using the following keywords: (“aerosols,” OR “nebulizers”) AND (“high flow nasal cannula” OR “high flow oxygen therapy” OR “HFNC”) AND (“COVID-19,” OR “SARS- CoV-2”). Twenty-eight articles including in vitro studies, randomized clinical trials, scintigraphy studies, review articles, prospective and retrospective research were included in this review. -

Oxygen Therapy
Copyright EMAP Publishing 2015 This article is not for distribution Keywords: Breathing/Oxygen/ Nursing Practice Oxygen therapy/Respiratory care Practice educator ●This article has been double-blind Respiratory care peer reviewed Oxygen therapy can be lifesaving but nurses must know how it works, when to use it, and how to correctly assess and evaluate a patient’s treatment Practical procedures: oxygen therapy In this article... 5 key The rationale for using oxygen therapy in acute illness points Hypoxia is an Available oxygen delivery devices and indications for use 1indication that The need for monitoring while administering oxygen therapy oxygen therapy should be started If blood Author Sandra Olive, respiratory nurse hypoxaemia (low blood oxygen levels); 2oxygen levels specialist, Norfolk and Norwich University » Prescribing a target oxygen are not low, oxygen Hospitals Foundation Trust. saturation range to guide will not treat Abstract Olive S (2016) Practical therapeutic treatment. breathlessness procedures: oxygen therapy. Oxygen does not treat breathlessness in A target Nursing Times; 112: 1/2, 12-14. the absence of hypoxaemia (O’Driscoll et 3oxygen Knowing when to start patients on oxygen al, 2008). saturation range therapy can save lives, but ongoing In an emergency situation, immediate should be assessment and evaluation must be assessment of airway patency, breathing prescribed to carried out to ensure the treatment is safe and circulation is essential, and in critical guide therapy and effective. This article outlines when illness such as peri-arrest, high-concentra- A lower target oxygen therapy should be used and the tion oxygen should be commenced via res- 4saturation procedures to follow. -
A Guide to Aerosol Delivery Devices for Respiratory Therapists 4Th Edition
A Guide To Aerosol Delivery Devices for Respiratory Therapists 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC Platinum Sponsor Copyright ©2017 by the American Association for Respiratory Care A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC With a Foreword by Timothy R. Myers, MBA, RRT-NPS, FAARC Chief Business Officer American Association for Respiratory Care DISCLOSURE Douglas S. Gardenhire, EdD, RRT-NPS, FAARC has served as a consultant for the following companies: Westmed, Inc. and Boehringer Ingelheim. Produced by the American Association for Respiratory Care 2 A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition American Association for Respiratory Care, © 2017 Foreward Aerosol therapy is considered to be one of the corner- any) benefit from their prescribed metered-dose inhalers, stones of respiratory therapy that exemplifies the nuances dry-powder inhalers, and nebulizers simply because they are of both the art and science of 21st century medicine. As not adequately trained or evaluated on their proper use. respiratory therapists are the only health care providers The combination of the right medication and the most who receive extensive formal education and who are tested optimal delivery device with the patient’s cognitive and for competency in aerosol therapy, the ability to manage physical abilities is the critical juncture where science inter- patients with both acute and chronic respiratory disease as sects with art. -
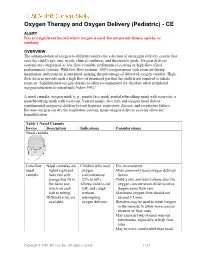
Oxygen Therapy and Oxygen Delivery (Pediatric) - CE
Oxygen Therapy and Oxygen Delivery (Pediatric) - CE ALERT Fire is a significant hazard where oxygen is used. Do not permit flames, sparks, or smoking. OVERVIEW The administration of oxygen to children requires the selection of an oxygen delivery system that suits the child’s age, size, needs, clinical condition, and therapeutic goals. Oxygen delivery systems are categorized as low-flow (variable performance) systems or high-flow (fixed performance) systems. With low-flow systems, 100% oxygen mixes with room air during inspiration, and room air is entrained, making the percentage of delivered oxygen variable. High- flow devices provide such a high flow of premixed gas that the child is not required to inhale room air. Supplemental oxygen therapy is often recommended for children when peripheral oxygen saturation is consistently below 94%.1 A nasal cannula, oxygen mask (e.g., simple face mask, partial rebreathing mask with reservoir, a nonrebreathing mask with reservoir, Venturi mask), face tent, and oxygen hood deliver supplemental oxygen to children to treat hypoxia, respiratory distress, and respiratory failure. Because oxygen can dry the respiratory system, many oxygen delivery systems allow for humidification. Table 1 Nasal Cannula Device Description Indications Considerations Nasal cannula Low-flow Nasal cannulas are Children who need FIO2 inconsistent. nasal lightweight and oxygen Most commonly used oxygen delivery cannula have two soft concentrations device. prongs that fit in 22% to 60%. Child’s size and tidal volume alter the the nares and Allows child to eat, oxygen concentration child receives attach on each talk, and cough despite same flow rate. side to tubing. without Maximum oxygen flow should not Different sizes are interrupting exceed 4 L/min.