Local Anesthesia Manual Local Anesthesia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Palatal Injection Does Not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth
Open Access Review Article DOI: 10.7759/cureus.2120 Palatal Injection does not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth Joe Iwanaga 1 , R. Shane Tubbs 2 1. Seattle Science Foundation 2. Neurosurgery, Seattle Science Foundation Corresponding author: Joe Iwanaga, [email protected] Abstract The superior alveolar nerves course lateral to the maxillary sinus and the greater palatine nerve travels through the hard palate. This difficult three-dimensional anatomy has led some dentists and oral surgeons to a critical misunderstanding in developing the anterior and middle superior alveolar (AMSA) nerve block and the palatal approach anterior superior alveolar (P-ASA) nerve block. In this review, the anatomy of the posterior, middle and anterior superior alveolar nerves, greater palatine nerve, and nasopalatine nerve are revisited in order to clarify the anatomy of these blocks so that the perpetuated anatomical misunderstanding is rectified. We conclude that the AMSA and P-ASA nerve blockades, as currently described, are not based on accurate anatomy. Categories: Anesthesiology, Medical Education, Other Keywords: anatomy, innervation, local anesthesia, maxillary nerve, nerve block, tooth Introduction And Background Anesthetic blockade of the posterior superior alveolar (PSA) branch of the maxillary nerve has played an important role in the endodontic treatment of irreversible acute pulpitis of the upper molar teeth except for the mesiobuccal root of the first molar tooth [1, 2]. This procedure requires precise anatomical knowledge of the pterygopalatine fossa and related structures in order to avoid unnecessary complications and to make the blockade most effective. The infraorbital nerve gives rise to middle superior alveolar (MSA) and anterior superior alveolar (ASA) branches. -

Accidental Displacement of Mandibular Third Molar Root Into the Submandibular Space: a Case Report
Case Report ERA’S JOURNAL OF MEDICAL RESEARCH VOL.6 NO.1 ACCIDENTAL DISPLACEMENT OF MANDIBULAR THIRD MOLAR ROOT INTO THE SUBMANDIBULAR SPACE: A CASE REPORT Mayur Vilas Limbhore, Viren S Patil, Shandilya Ramanojam, Vrushika Mahajan, Pallavi Rathi, Kisna Tadas Department of Oral and Maxillofacial surgery Bharati Vidyapeeth Dental College, Katraj, Pune, Maharashtra, India-411030 Received on : 01-04-2018 Accpected on : 10-04-2018 ABSTRACT Address for correspondence Accidental displacement of an impacted third molar, either a crown, Dr. Mayur Vilas Limbhore root piece, or the entire tooth, is a rare complication that occurs Department of Oral and Maxillofacial Surgery during surgical removal. The most common sites of dislodgment of an impacted mandibular third molar root are the submandibular, Bharati Vidyapeth Dental College, sublingual and pterygomandibular spaces. Removal of a displaced Katraj, Pune, Maharashtra, India-411030 root from these spaces may be complex due to poor visualization Email: [email protected] and limited access. A thorough evaluation of all significant risk Contact no: +91-8552887325 factors must be performed in advance to prevent complications. This case report reveals the management of accidental displaced mandibular third molar root into the submandibular space. An 39 years-old male patient underwent a third mandibular molar extraction. Accidentally, the mandibular right third molar distal root was displaced into the submandibular space, making necessary a second surgical step. After 2 days awaiting an asymptomatic health status, the second surgical step was successfully performed using multislice CBCT as preoperative imaging guide. The present case report highlights the clinical usefulness of CBCT in proper treatment of the patient. -
Proxymetacaine Hydrochloride Ropivacaine Hydrochloride
1870 Local Anaesthetics Preparations pore: Alcaine; Switz.: Alcaine; Turk.: Alcaine; Opticaine; USA: Ak-Taine; Alcaine; Ocu-Caine; Ophthetic; Parcaine; Venez.: Alcaine; Oftaine†; Poen- (details are given in Part 3) caina. Proprietary Preparations CH3 Multi-ingredient: Spain: Detraine. O Multi-ingredient: Canad.: Fluoracaine†; USA: Fluoracaine; Fluorocaine. N CH3 O Quinisocaine Hydrochloride (BANM, rINNM) H3C Propipocaine (rINN) O Chinisocainum Hydrochloride; Dimethisoquin Hydrochloride Propipocaína; Propipocaïne; Propipocainum; Propoxypipero- (USAN); Dimethisoquinium Chloride; Hidrocloruro de quinisocaí- NH2 caine. 3-Piperidino-4′-propoxypropiophenone. na; Quinisocaïne, Chlorhydrate de; Quinisocaini Hydrochlori- (proxymetacaine) dum. 2-(3-Butyl-1-isoquinolyloxy)-NN-dimethylethylamine hy- Пропипокаин drochloride. C17H25NO2 = 275.4. Хинизокаина Гидрохлорид CAS — 3670-68-6. NOTE. PROX is a code approved by the BP 2008 for use on single unit doses of eye drops containing proxymetacaine hydrochlo- C17H24N2O,HCl = 308.8. ride where the individual container may be too small to bear all CAS — 86-80-6 (quinisocaine); 2773-92-4 (quinisocaine the appropriate labelling information. PROXFLN is a similar hydrochloride). O code approved for eye drops containing proxymetacaine hydro- ATC — D04AB05. chloride and fluorescein sodium. ATC Vet — QD04AB05. N Pharmacopoeias. In Br. and US. BP 2008 (Proxymetacaine Hydrochloride). A white or almost H3C CH3 white, odourless or almost odourless, crystalline powder. Soluble O in water and in chloroform; very soluble in dehydrated alcohol; N practically insoluble in ether. A 1% solution in water has a pH of O CH Profile 5.7 to 6.4. Protect from light. 3 Propipocaine is a local anaesthetic (p.1850) that has been used USP 31 (Proparacaine Hydrochloride). A white to off-white, or for surface anaesthesia. -
Anatomical Overview
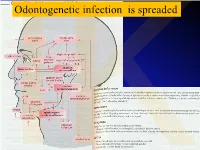
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

Retained Surgical Items Evidence Table
Guideline for Prevention of Retained Surgical Items Evidence Table CITATION CONCLUSION(S) SAMPLE SIZE REFERENCE # POPULATION COMPARISON EVIDENCE TYPE INTERVENTIONS CONSENSUS SCORE OUTCOME MEASURE 1 Wilson C. Foreign bodies left in the Case series of foreign bodies left in the abdomen. Cases VC Literature n/a n/a n/a n/a Retained abdomen after laparotomy. Trans Am found through publication, interviews, and the author's own Review, Clinician sponges Gynecol Soc. 1884;9:94-117. experience. Experience, and Case Report 2 The Joint Commission. Preventing The Joint Commission recommends that facilities develop IVB Consensus n/a n/a n/a n/a n/a unintended retained foreign objects. effective processes and procedures for preventing Sentinel Event Alert. October 17, unintended retained foreign objects. Their recommendations 2013;51. include a standardized and highly reliable counting system; http://www.jointcommission.org/sea_i development of policies and procedures; practices for ssue_51/. Accessed November 10, counting, wound opening, and closing procedures; 2015. performance of intraoperative radiographs; use of effective communication to include briefings and debriefings; documentation of counts; and assistive technologies (ie, RF tags, RFID, radiopaque, bar coding). Also, the hospital should define a process for conducting RCA for sentinel events, such as URFO. Page 1 of 60 Guideline for Prevention of Retained Surgical Items Evidence Table CITATION CONCLUSION(S) SAMPLE SIZE REFERENCE # POPULATION COMPARISON EVIDENCE TYPE INTERVENTIONS CONSENSUS SCORE OUTCOME MEASURE 3 Moffatt-Bruce SD, Cook CH, Steinberg 7 elevated risk factors for RSI in pooled data in case-control IIIA Systematic USA hospitals, n/a n/a 3 studies: Estimated SM, Stawicki SP. -

8–16–01 Vol. 66 No. 159 Thursday Aug. 16, 2001 Pages 42929
8–16–01 Thursday Vol. 66 No. 159 Aug. 16, 2001 Pages 42929–43064 VerDate 11-MAY-2000 19:13 Aug 15, 2001 Jkt 194001 PO 00000 Frm 00001 Fmt 4710 Sfmt 4710 E:\FR\FM\16AUWS.LOC pfrm11 PsN: 16AUWS 1 II Federal Register / Vol. 66, No. 159 / Thursday, August 16, 2001 The FEDERAL REGISTER is published daily, Monday through SUBSCRIPTIONS AND COPIES Friday, except official holidays, by the Office of the Federal Register, National Archives and Records Administration, PUBLIC Washington, DC 20408, under the Federal Register Act (44 U.S.C. Subscriptions: Ch. 15) and the regulations of the Administrative Committee of Paper or fiche 202–512–1800 the Federal Register (1 CFR Ch. I). The Superintendent of Assistance with public subscriptions 512–1806 Documents, U.S. Government Printing Office, Washington, DC 20402 is the exclusive distributor of the official edition. General online information 202–512–1530; 1–888–293–6498 Single copies/back copies: The Federal Register provides a uniform system for making available to the public regulations and legal notices issued by Paper or fiche 512–1800 Federal agencies. These include Presidential proclamations and Assistance with public single copies 512–1803 Executive Orders, Federal agency documents having general FEDERAL AGENCIES applicability and legal effect, documents required to be published Subscriptions: by act of Congress, and other Federal agency documents of public interest. Paper or fiche 523–5243 Assistance with Federal agency subscriptions 523–5243 Documents are on file for public inspection in the Office of the Federal Register the day before they are published, unless the issuing agency requests earlier filing. -

Anatomy of the Pterygomandibular Space — Clinical Implication and Review
FOLIA MEDICA CRACOVIENSIA 79 Vol. LIII, 1, 2013: 79–85 PL ISSN 0015-5616 MARCIN LIPSKI1, WERONIKA LIPSKA2, SYLWIA MOTYL3, Tomasz Gładysz4, TOMASZ ISKRA1 ANATOMY OF THE PTERYGOMANDIBULAR SPACE — CLINICAL IMPLICATION AND REVIEW Abstract: A i m: The aim of this study was to present review of the pterygomandibular space with some referrals to clinical practice, specially to the methods of lower teeth anesthesia. C o n c l u s i o n s: Pterygomandibular space is a clinically important region which is commonly missing in anatomical textbooks. More attention should be paid to it both from theoretical and practical point of view, especially in teaching the students of first year of dental studies. Key words: pterygomandibular space, Gow-Gates anesthesia, inferior alveolar nerve. INTRODUCTION Numerous cranial regions have been subjects of various anatomical and anthro- pological studies [1, 2]. Most of them indicate necessity of undertaking of such studies first of all because of clinical importance [3–5]. Inferior alveolar nerve blocs, one of the most common procedures in dentistry requires deep anatomical knowledge of the pterygomandibular space [6, 7]. This space is a narrow gap, which contains mostly loose areolar tissue. It communi- cates however through the mandibular foramen with the mandibular canal, which is traversed by inferior alveolar nerve, artery and comitant vein (IANAV). Many of the structures placed in this space are of certain importance for local anesthesia. Khoury at al. [8, 9] mention here the following: inferior alveolar nerve, artery and vein, lingual nerve, nerve to mylohyoid and the sphenomandibular ligament. The space contains mostly loose areolar tissue. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -

WO 2016/140629 Al 9 September 2016 (09.09.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/140629 Al 9 September 2016 (09.09.2016) P O P C T (51) International Patent Classification: (74) Agent: BULUT, Pinar; FarmaPatent Limited Sirketi, A61K 36/28 (2006.01) A61P 17/02 (2006.01) GMK Bulvari No:42/5, Maltepe, 06440 Ankara (TR). A61K 36/38 (2006.01) A61P 23/00 (2006.01) (81) Designated States (unless otherwise indicated, for every A61K 31/167 (2006.01) kind of national protection available): AE, AG, AL, AM, (21) International Application Number: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, PCT/TR20 15/000088 BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 5 March 2015 (05.03.2015) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (25) Filing Language: English MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, (71) Applicant: PHARMACTFVE ILAC SANAYI VE Tl- TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. CARET A. S. [TR/TR]; Mahmutbey Mah. Dilmenler Cad., (84) Designated States (unless otherwise indicated, for every Aslanoba Plaza No: 19 K:3, Bagcilar/istanbul (TR). -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Orbital Malignant Peripheral Nerve Sheath Tumours
Br J Ophthalmol: first published as 10.1136/bjo.73.9.731 on 1 September 1989. Downloaded from British Journal of Ophthalmology, 1989, 73, 731-738 Orbital malignant peripheral nerve sheath tumours CHRISTOPHER J LYONS,' ALAN A McNAB,l ALEC GARNER,2 AND JOHN E WRIGHT' From the I Orbital clinic, Moorfields Eye Hospital, City Road, London EC] V 2PD, and the 2Department of Pathology, Institute ofOphthalmology, London EC] V 9A T SUMMARY We describe three patients with malignant peripheral nerve tumours in the orbit and review the existing literature on these rare lesions. Malignant peripheral nerve sheath tumours are Sensation was diminished over the distribution of the unusual in any part of the body and very rare in the second division of the right trigeminal nerve. The left orbit, where only 13 cases have previously been globe was normal. Plain anteroposterior skull x-rays described. These tumours can spread rapidly along showed a normal appearance, but undertilted the involved nerve to the middle cranial fossa. They occipitomental tomographic views revealed enlarge- are radioresistant, and total surgical excision offers ment of the right infraorbital canal (Fig. 1). copyright. the only hope of cure. Our experience with three An inferior orbital margin incision revealed patients may help clinicians to recognise these lesions tumour protruding from the infraorbital foramen and and excise them at an early stage. extending beneath the soft tissues of the cheek. The tumour had a firm consistency and a pale grey cut Case reports surface. The orbital periosteum on the floor of the orbit was elevated and a mass over 18 mm in diameter PATIENT 1 was found within an expanded infraorbital canal Four years prior to presentation a man which extended posteriorly into the superior orbital 55-year-old http://bjo.bmj.com/ noted a small lump at the medial end of his right fissure. -

Local Anesthetics
Local Anesthetics Introduction and History Cocaine is a naturally occurring compound indigenous to the Andes Mountains, West Indies, and Java. It was the first anesthetic to be discovered and is the only naturally occurring local anesthetic; all others are synthetically derived. Cocaine was introduced into Europe in the 1800s following its isolation from coca beans. Sigmund Freud, the noted Austrian psychoanalyst, used cocaine on his patients and became addicted through self-experimentation. In the latter half of the 1800s, interest in the drug became widespread, and many of cocaine's pharmacologic actions and adverse effects were elucidated during this time. In the 1880s, Koller introduced cocaine to the field of ophthalmology, and Hall introduced it to dentistry Overwiev Local anesthetics (LAs) are drugs that block the sensation of pain in the region where they are administered. LAs act by reversibly blocking the sodium channels of nerve fibers, thereby inhibiting the conduction of nerve impulses. Nerve fibers which carry pain sensation have the smallest diameter and are the first to be blocked by LAs. Loss of motor function and sensation of touch and pressure follow, depending on the duration of action and dose of the LA used. LAs can be infiltrated into skin/subcutaneous tissues to achieve local anesthesia or into the epidural/subarachnoid space to achieve regional anesthesia (e.g., spinal anesthesia, epidural anesthesia, etc.). Some LAs (lidocaine, prilocaine, tetracaine) are effective on topical application and are used before minor invasive procedures (venipuncture, bladder catheterization, endoscopy/laryngoscopy). LAs are divided into two groups based on their chemical structure. The amide group (lidocaine, prilocaine, mepivacaine, etc.) is safer and, hence, more commonly used in clinical practice.