A Quick Guide to Capnography
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Gastrointestinal Tract and Ventilator-Associated Pneumonia
The Gastrointestinal Tract and Ventilator-Associated Pneumonia Richard H Kallet MSc RRT FAARC and Thomas E Quinn MD Introduction The Role of Gastric pH on the Incidence of VAP Enteral Feeding and Nosocomial Pneumonia Gastric Residual Volumes Gastric Versus Post-Pyloric Feeding Acidification of Enteral Feedings Selective Decontamination of the Digestive Tract Microbiologic Ecology of the GI Tract Rationale for SDD Technique Clinical Evidence: Efficacy of SDD SDD and the Incidence of VAP SDD and Mortality SDD in Specific Sub-Groups SDD and ICU Length of Stay, Hospital Costs, and Antibiotic Usage/Costs Unresolved Aspects of SDD Therapy Uncertainties Regarding the Gastropulmonary Hypothesis Uncertainties Regarding Colonization Resistance SDD and Selection for Drug-Resistant Microorganisms Summary and Recommendations The gastrointestinal tract is believed to play an important role in ventilator-associated pneumonia (VAP), because during critical illness the stomach often is colonized with enteric Gram-negative bacteria. These are the same bacteria that frequently are isolated from the sputum of patients with VAP. Interventions such as selective decontamination of the digestive tract (SDD), use of sucralfate for stress ulcer prophylaxis, and enteral feeding strategies that preserve gastric pH, or lessen the likelihood of pulmonary aspiration, are used to decrease the incidence of VAP. A review of both meta-analyses and large randomized controlled trials providing Level I evidence on these topics has led to the following conclusions. First, SDD substantially decreases the incidence of VAP and may have a modest positive effect on mortality. However, there is strong contravening evidence that SDD promotes infections by Gram-positive bacteria. In the context of an emerging public health crisis from the steady rise in drug-resistant Gram-positive bacteria, we cannot endorse the general use of SDD to prevent VAP. -

From Mechanical Ventilation to Intensive Care Medicine: a Challenge &For Bosnia and Herzegovina
FROM MECHANICAL VENTILATION TO INTENSIVE CARE MEDICINE: A CHALLENGE &FOR BOSNIA AND HERZEGOVINA Guillaume Thiéry1,2,3*, Pedja Kovačević2,4, Slavenka Štraus5, Jadranka Vidović2, Amer Iglica1, Emir Festić6, Ognjen Gajić7 ¹ Medical Intensive Care Unit, Clinical Centre University of Sarajevo, Bolnička , Sarajevo, Bosnia and Herzegovina ² Medical Intensive Care Unit, Clinical Center Banja Luka, Banja Luka, Bosnia and Hercegovina ³ Medical Intensive Care Unit, St Louis Hospital, University Denis Diderot, avenue Claude Vellefaux, Paris, France ⁴ Faculty of Medicine, University of Banja Luka, Banja Luka, Bosnia and Hercegovina 5 Heart Center, Clinical Centre University of Sarajevo, Bolnička , Sarajevo, Bosnia and Herzegovina 6 Department of Critical Care Medicine, Mayo Clinic, Jacksonville, FL, USA 7 Division of Pulmonary and Critical Care, Multidisciplinary Epidemiology and Translational Research in Intensive Care (METRIC) Mayo Clinic, Rochester, MN, United States * Corresponding author Abstract Intensive care medicine is a relatively new specialty, which was created in the ’s, after invent of mechanical ventilation, which allowed caring for critically ill patients who otherwise would have died. First created for treating mechanically ventilated patients, ICUs extended their scope and care to all patients with life threatening conditions. Over the years, intensive care medicine developed further and became a truly multidisciplinary speciality, encompassing patients from various fi elds of medicine and involving special- ists from a range of base specialties, with additional (subspecialty) training in intensive care medicine. In Bosnia and Herzegovina, the founding of the society of intensive care medicine in , the introduction of non invasive ventilation in , and opening of a multidisciplinary ICUs in Banja Luka and Sarajevo heralded a new age of intensive care medicine. -

Weaning and Discontinuing Ventilatory Support (2002)
Special Articles Evidence-Based Guidelines for Weaning and Discontinuing Ventilatory Support A Collective Task Force Facilitated by the American College of Chest Physicians, the American Association for Respiratory Care, and the American College of Critical Care Medicine Introduction Pathophysiology of Ventilator Dependence Criteria to Assess Ventilator Dependence Managing the Patient Who Has Failed a Spontaneous Breathing Test Role of Tracheotomy in Ventilator-Dependent Patients The Role of Long-Term Facilities [Respir Care 2002;47(1):69–90] Introduction quickly as possible. Although this process often is termed “ventilator weaning” (implying a gradual process), we pre- The discontinuation or withdrawal process from me- fer the more encompassing term “discontinuation.” chanical ventilation is an important clinical issue.1,2 Pa- tients are generally intubated and placed on mechanical SEE THE RELATED EDITORIAL ON PAGE 29 ventilators when their own ventilatory and/or gas exchange capabilities are outstripped by the demands placed on them Unnecessary delays in this discontinuation process in- from a variety of diseases. Mechanical ventilation also is crease the complication rate from mechanical ventilation required when the respiratory drive is incapable of initi- (eg, pneumonia, airway trauma) as well as the cost. Ag- ating ventilatory activity, either because of disease pro- gressiveness in removing the ventilator, however, must be cesses or drugs. As the conditions that warranted placing balanced against the possibility that premature discontin- the patient on the ventilator stabilize and begin to resolve, uation may occur. Premature discontinuation carries its attention should be placed on removing the ventilator as own set of problems, including difficulty in reestablishing artificial airways and compromised gas exchange. -

Evaluation and Management of the Polytraumatized Patient in Various Centers
World J. Surg. 7, 143-148, 1983 Wor Journal of Stirgery Evaluation and Management of the Polytraumatized Patient in Various Centers S. Olerud, M.D., and M. Allg6wer, M.D. The Akademiska Sjukhuset Uppsala, Sweden, and the Department of Surgery, Kantonsspital, Basel, Switzerland A questionnaire was sent to the following 6 trauma centers: Paris: Two or more peripheral, visceral, or com- University Hospital for Accident Surgery, Hannover, Fed- plex injuries with respiratory and circulatory fail- eral Republic of Germany (Prof. H. Tscherne); University ure. (This excludes patients who only have sus- of Munich, Department of Surgery, Klinikum Grossha- tained fractures.) dern, Munich, Federal Republic of Germany (Prof. G. Dallas: Multiply injured patient presenting le- Heberer); Akademiska Sjukhuset Uppsala, Sweden (Prof. sions to 2 cavities, associated with 2 or more long S. Olerud); University Hospital, Department of Surgery, bone failures; lesions to 1 cavity associated with 2 Basel, Switzerland (Prof. M. Allgiiwer); H6pital de la Piti~, or more long bone failures; or lesions to multiple Paris, France (Prof. R. Roy-Camille); and University of extremities (at minimum, 3 long bone failures). Texas Southwestern Medical School, Dallas, Texas, U.S.A. (Prof. B. Claudi). Their answers have been summarized in a few short paragraphs where tabulation was not possible, Do You Grade Polytrauma, and If So, How? and then mainly in tabular form for convenient comparison among the various centers. There seems to be considerable international agreement on the main points of early aggres- Hannover: Yes, with our own grading system along sive cardiopulmonary management to prevent multiple with ISS and AIS. -

Infection in Patients Under Artificial Ventilation
ISSN: 1981-8963 DOI: 10.5205/reuol.3188-26334-1-LE.0704201307 Batista JF, Santos IBC, Leite KNS et al. Infection In patients under artificial… ORIGINAL ARTICLE INFECTION IN PATIENTS UNDER ARTIFICIAL VENTILATION: UNDERSTANDING AND PREVENTIVE MEASURES ADOPTED BY NURSING STUDENTS INFECÇÃO EM PACIENTES SOB VENTILAÇÃO ARTIFICIAL: COMPREENSÃO E MEDIDAS PREVENTIVAS ADOTADAS POR ESTUDANTES DE ENFERMAGEM INFECCIÓN EN LOS PACIENTES POR VENTILACIÓN ARTIFICIAL: COMPRENSIÓN Y MEDIDAS PREVENTIVAS ADOPTADAS POR ESTUDIANTES DE ENFERMERÍA Joyce Ferreira Batista1, Iolanda Beserra da Costa Santos2, Kamila Nethielly Souza Leite3, Ana Aline Lacet Zaccara4, Smalyanna Sgren da Costa Andrade5, Sergio Ribeiro dos Santos6 ABSTRACT Objective: to investigate the understanding of nursing students about the prevention of infection in patients under artificial ventilation in the Intensive Care Unit (ICU). Method: an exploratory field study with a quantitative approach. 30 students participated. It was used a questionnaire to collect the data that were then processed and analyzed manually, from statistical software, with results shown in tables and figures. The research project was approved by the Ethics Committee in Research, with CAEE 0539.0.126.000-10. Results: 67% did not attend patients suffering from hospital infections. It was mentioned as preventive measures: 28 (24%), the education of the healthcare team, 10 (23%) cited the use of aseptic techniques, 9 (20.0%) say they do not know what actions should be taken. Conclusion: the study showed that the majority of the students cited as preventive measures the continuous education in service and the use of aseptic techniques. Descriptors: Nursing Students; Infection; Intensive Care Units. RESUMO Objetivo: investigar a compreensão de estudantes de enfermagem sobre a prevenção de infecção em pacientes sob ventilação artificial na Unidade de Terapia Intensiva (UTI). -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -

Evidence on Measures for the Prevention of Ventilator-Associated Pneumonia
Eur Respir J 2007; 30: 1193–1207 DOI: 10.1183/09031936.00048507 CopyrightßERS Journals Ltd 2007 REVIEW Evidence on measures for the prevention of ventilator-associated pneumonia L. Lorente*, S. Blot# and J. Rello",+ AFFILIATIONS ABSTRACT: Ventilator-associated pneumonia (VAP) continues to be an important cause of *Intensive Care Unit, Hospital morbidity and mortality in ventilated patients. Universitario de Canarias, La Laguna, Evidence-based guidelines have been issued since 2001 by the European Task Force on Tenerife, "Intensive Care Dept, Joan XXIII ventilator-associated pneumonia, the Centers for Disease Control and Prevention, the Canadian University Hospital, and Critical Care Society, and also by the American Thoracic Society and Infectious Diseases Society +University Rovira i Virgili Medical of America, which have produced a joint set of recommendations. School, Pere Virgili Health Institut, The present review article is based on a comparison of these guidelines, together with an Tarragona, Spain. #Critical Care Dept, Ghent University update of further publications in the literature. The 100,000 Lives campaign, endorsed by leading Hospital, Ghent, Belgium. US agencies and societies, states that all ventilated patients should receive a ventilator bundle to reduce the incidence of VAP. CORRESPONDENCE The present review article is useful for identifying evidence-based processes that can be L. Lorente Intensive Care Unit modified to improve patients’ safety. Hospital Universitario de Canarias C/ Ofra s/n KEYWORDS: Ventilator-associated pneumonia La Laguna Tenerife 38320 entilator-associated pneumonia (VAP) tracheal suctioning system’’, ‘‘open tracheal Spain Fax: 34 22662245 suctioning system’’, ‘‘change of closed tracheal continues to be an important cause of E-mail: [email protected] V morbidity and mortality in critically ill suctioning system’’, ‘‘sterilization’’, ‘‘disinfec- patients [1–3]. -
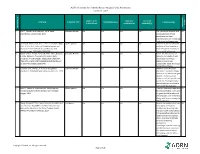
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures
Volume 2- Issue 1 : 2018 DOI: 10.26717/BJSTR.2018.02.000695 Eduardo de Oliveira Duque-Estrada. Biomed J Sci & Tech Res ISSN: 2574-1241 Mini Review Open Access The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures Eduardo de Oliveira Duque-Estrada MD* Received: January 17, 2018; Published: January 25, 2018 *Corresponding author: Eduardo de Oliveira Duque-Estrada, Ex-Professor of Pediatrics and Pediatric Surgery, Teresópolis Schoolof Medicine, Rio de Janeiro, Rua Jose da Silva Ribeiro 119 apt 11 São Paulo, SP Brazil CEP: 05726-130, Email: Abstract The local anesthetics are widely u sed in minor pediatric surgical procedures. The major problem with their use is the resulted pain experienced by the patients at the time of injection. To discuss those situations in the light of the medical literature we present this mini-review. Key words: Local Injection; Pain; Buffer; pH; Lidocaine; Pediatric Surgery Procedure Introduction Table 1: Techniques for injection pain control*. a eutectic mixture of lidocaine and prilocaine (EMLA) cream [17] S.No Techniques for injection pain control before infiltration, and local external cooling (cryoanalgesia) have 1. Warming the anesthetic solution [18,19] (Table 1). also been used to reduce the pain of infiltration of local anesthetic 2. Buffering the anesthetic Buffering the Anesthetic 3. Injection technique 4. Distraction Local anesthesia is extremely useful either as the sole method the best results on the minor surgery in general [3,6]. Blocking 5. Combination anesthetic technique the pain pathway with local anesthetic solution will also reduce 6. Cooling of skin the family stress response to the surgical procedure. -

Posttraumatic Stress Disorder (PTSD)
Child and Adolescent Psychiatry and Mental Health BioMed Central Research Open Access Posttraumatic stress disorder (PTSD) in children after paediatric intensive care treatment compared to children who survived a major fire disaster Madelon B Bronner*1, Hendrika Knoester2, Albert P Bos2, Bob F Last1,3 and Martha A Grootenhuis1 Address: 1Psychosocial Department, Emma Children's Hospital Academic Medical Center, University of Amsterdam, The Netherlands, 2Department of Paediatric Intensive Care, Emma Children's Hospital Academic Medical Center, University of Amsterdam, The Netherlands and 3Department of Developmental Psychology, Vrije Universiteit, Amsterdam, The Netherlands Email: Madelon B Bronner* - [email protected]; Hendrika Knoester - [email protected]; Albert P Bos - [email protected]; Bob F Last - [email protected]; Martha A Grootenhuis - [email protected] * Corresponding author Published: 20 May 2008 Received: 23 January 2008 Accepted: 20 May 2008 Child and Adolescent Psychiatry and Mental Health 2008, 2:9 doi:10.1186/1753-2000-2-9 This article is available from: http://www.capmh.com/content/2/1/9 © 2008 Bronner et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: The goals were to determine the presence of posttraumatic stress disorder (PTSD) in children after paediatric intensive care treatment, to identify risk factors for PTSD, and to compare this data with data from a major fire disaster in the Netherlands. -

Guidelines for Preventing Health-Care-Associated Pneumonia, 2003
GUIDELINES FOR PREVENTING HEALTH-CARE-ASSOCIATED PNEUMONIA, 2003 Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee Accessible version: https://www.cdc.gov/infectioncontrol/guidelines/pneumonia/index.html Prepared By: Ofelia C. Tablan, M.D.1 Larry J. Anderson, M.D.2 Richard Besser, M.D.3 Carolyn Bridges, M.D.2 Rana Hajjeh, M.D.3 1Division of Healthcare Quality Promotion, National Center for Infectious Diseases , CDC 2Division of Viral and Rickettsial Diseases, NCID, CDC 3Division of Bacterial and Mycotic Diseases, NCID, CDC The material in this report originated in the National Center for Infectious Diseases, James M. Hughes, M.D., Director, Division of Healthcare Quality Promotion, Denise M. Cardo, M.D., Director, and the Division of Bacterial and Mycotic Diseases, Mitchell L. Cohen, M.D., Director. HEALTHCARE INFECTION CONTROL PRACTICES ADVISORY COMMITTEE Chair: Robert A. Weinstein, M.D., Cook County Hospital, Chicago, Illinois Co-Chair: Jane D. Siegel, M.D., University of Texas Southwestern Medical Center, Dallas, Texas Executive Secretary: Michele L. Pearson, M.D., CDC, Atlanta, Georgia Members: Raymond Y.W. Chinn, M.D., Sharp Memorial Hospital, San Diego, California; Alfred DeMaria, Jr., M.D., Massachusetts Department of Public Health, Jamaica Plains, Massachusetts; Elaine L. Larson, R.N., Ph.D., Columbia University School of Nursing, New York, New York; James T. Lee, M.D.,Ph.D., Veterans Affairs Medical Center, University of Minnesota, St. Paul, Minnesota; Ramon E. Moncada, M.D.,Coronado Physician’s Medical Center Coronado, California; William A. Rutala, Ph.D.; University of North Carolina School of Medicine, Chapel Hill, North Carolina; William E. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC).