A Delphi Study on the Healthcare Needs of Patients with Type
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Taiwan's Nationwide Cancer Registry System of 40 Years: Past, Present
Journal of the Formosan Medical Association (2019) 118, 856e858 Available online at www.sciencedirect.com ScienceDirect journal homepage: www.jfma-online.com Perspective Taiwan’s Nationwide Cancer Registry System of 40 years: Past, present, and future Chun-Ju Chiang a,b, Ying-Wei Wang c, Wen-Chung Lee a,b,* a Institute of Epidemiology and Preventive Medicine, College of Public Health, National Taiwan University, Taipei, Taiwan b Taiwan Cancer Registry, Taipei, Taiwan c Health Promotion Administration, Ministry of Health and Welfare, Taipei, Taiwan Received 29 October 2018; accepted 15 January 2019 The Taiwan Cancer Registry (TCR) is a nationwide demonstrate that the TCR is one of the highest-quality population-based cancer registry system that was estab- cancer registries in the world.3 lished by the Ministry of Health and Welfare in 1979. The The TCR publishes annual cancer statistics for all cancer data of patients with newly diagnosed malignant cancer in sites, and the TCR’s accurate data is used for policy making hospitals with 50 or more beds in Taiwan are collected and and academic research. For example, the Health Promotion reported to the TCR. To evaluate cancer care patterns and Administration (HPA) in Taiwan has implemented national treatment outcomes in Taiwan, the TCR established a long- screening programs for cancers of the cervix uteri, oral form database in which cancer staging and detailed treat- cavity, colon, rectum, and female breast,4 and the TCR ment and recurrence information has been recorded since database has been employed to verify the effectiveness of 2002. Furthermore, in 2011, the long-form database these nationwide cancer screening programs for reducing began to include detailed information regarding cancer cancer burdens in Taiwan.5,6 Additionally, liver cancer was site-specific factors, such as laboratory values, tumor once a major health problem in Taiwan; however, since the markers, and other clinical data related to patient care. -

Democratic Values and Democratic Support in East Asia
Democratic Values and Democratic Support in East Asia Kuan-chen Lee [email protected] Postdoctoral fellow, Institute of Political Science, Academia Sinica Judy Chia-yin Wei [email protected] Postdoctoral fellow, Center for East Asia Democratic Studies, National Taiwan University Stan Hok-Wui Wong [email protected] Assistant Professor, Department of Applied Social Sciences, Hong Kong Polytechnic University Karl Ho [email protected] Associate Professor, School of Economic, Political, and Policy Sciences, University of Texas at Dallas Harold D. Clarke [email protected] Ashbel Smith Professor, School of Economic, Political, and Policy Sciences, University of Texas at Dallas Introduction In East Asia, 2014 was an epochal year for transformation of social, economic and political orders. Students in Taiwan and Hong Kong each led a large scale social movement in 2014 that not only caught international attention, but also profoundly influenced domestic politics afterwards. According to literature of political socialization, it is widely assumed that the occurrences of such a huge event will produce period effects which bring socio-political attitudinal changes for all citizens, or at least, cohort effects, which affect political views for a group of people who has experienced the event in its formative years. While existing studies have accumulated fruitful knowledge in the socio-political structure of the student-led movement, the profiles of the supporters in each movement, as well as the causes and consequences of the student demonstrations in the elections (Ho, 2015; Hawang, 2016; Hsiao and Wan, 2017; Stan, forthcoming; Ho et al., forthcoming), relatively few studies pay attention to the link between democratic legitimacy and student activism. -

Study in Taiwan - 7% Rich and Colorful Culture - 15% in Taiwan, Ancient Chinese Culture Is Uniquely Interwoven No.7 in the Fabric of Modern Society
Le ar ni ng pl us a d v e n t u r e Study in Foundation for International Cooperation in Higher Education of Taiwan (FICHET) Address: Room 202, No.5, Lane 199, Kinghua Street, Taipei City, Taiwan 10650, R.O.C. Taiwan Website: www.fichet.org.tw Tel: +886-2-23222280 Fax: +886-2-23222528 Ministry of Education, R.O.C. Address: No.5, ZhongShan South Road, Taipei, Taiwan 10051, R.O.C. Website: www.edu.tw www.studyintaiwan.org S t u d y n i T a i w a n FICHET: Your all – inclusive information source for studying in Taiwan FICHET (The Foundation for International Cooperation in Higher Education of Taiwan) is a Non-Profit Organization founded in 2005. It currently has 114 member universities. Tel: +886-2-23222280 Fax: +886-2-23222528 E-mail: [email protected] www.fichet.org.tw 加工:封面全面上霧P 局部上亮光 Why Taiwan? International Students’ Perspectives / Reasons Why Taiwan?1 Why Taiwan? Taiwan has an outstanding higher education system that provides opportunities for international students to study a wide variety of subjects, ranging from Chinese language and history to tropical agriculture and forestry, genetic engineering, business, semi-conductors and more. Chinese culture holds education and scholarship in high regard, and nowhere is this truer than in Taiwan. In Taiwan you will experience a vibrant, modern society rooted in one of world’s most venerable cultures, and populated by some of the most friendly and hospitable people on the planet. A great education can lead to a great future. What are you waiting for? Come to Taiwan and fulfill your dreams. -

Multilevel Spatial Impact Analysis of High-Speed Rail and Station Placement: a Short-Term Empirical Study of the Taiwan HSR
T J T L U http://jtlu.org V. 13 N. 1 [2020] pp. 317–341 Multilevel spatial impact analysis of high-speed rail and station placement: A short-term empirical study of the Taiwan HSR Yu-Hsin Tsai Jhong-yun Guan National Chengchi University Dept. of Urban Development, Taipei City [email protected] Government [email protected] Yi-hsin Chung Dept. of Urban Development, Taipei City Government [email protected] Abstract: Understanding the impact of high-speed rail (HSR) services Article history: on spatial distributions of population and employment is important for Received: September 15, 2019 planning and policy concerning HSR station location as well as a wide Received in revised form: May range of complementary spatial, transportation, and urban planning 14, 2020 initiatives. Previous research, however, has yielded mixed results into the Accepted: May 26, 2020 extent of this impact and a number of influential factors rarely have been Available online: November 4, controlled for during assessment. This study aims to address this gap 2020 by controlling for socioeconomic and transportation characteristics in evaluating the spatial impacts of HSR (including station placement) at multiple spatial levels to assess overall impact across metropolitan areas. The Taiwan HSR is used for this empirical study. Research methods include descriptive statistics, multilevel analysis, and multiple regression analysis. Findings conclude that HSR-based towns, on average, may experience growing population and employment, but HSR-based counties are likely to experience relatively less growth of employment in the tertiary sector. HSR stations located in urban or suburban settings may have a more significant spatial impact. -

Special Issue on Mobility and Human Interaction Guest Editorial Preface
InternatIonal Journal of technology and human InteractIon October-December 2013, Vol. 9, No. 4 Table of Contents Special Issue on Mobility and Human Interaction Guest Editorial Preface iv Shu-Lu Hsu, National Chiayi University, Chiayi City, Taiwan Hong-Yi Chang, National Chiayi University, Chiayi City, Taiwan Research Articles 1 Intention to Adopt a Text Message-based Mobile Coaching Service to Help Stop Smoking: Which Explanatory Variables? Silvia Cacho-Elizondo, IPADE Business School, Mexico City, DF, Mexico Niousha Shahidi, EDC Paris Business School, Observatoire et Centre de Recherche en Entrepreneuriat, Ecole des Dirigeants et Créateurs d’Entreprise, Paris, France Vesselina Tossan, CNAM, Lirsa, France & EDC Paris Business School, Paris, France 20 Like, Share, Recommend: Smartphones as a Self-Broadcast and Self-Promotion Medium of College Students Franklin N. A. Yartey, Communication Department, University of Dubuque, Dubuque, IA, USA Louisa Ha, Department of Telecommunications, Bowling Green State University, Bowling Green, OH, USA 41 High Performance Reversible Data Hiding for Mobile Applications and Human Interaction Fong-Hao Liu, Department of Information Management, Management College, National Defense University, Taipei City, Taiwan Hsiang-Fu Lo, Department of Electrical Engineering, TamKang University, New Taipei City, Taiwan Chun-Te Su, Department of Information Management, Management College, National Defense University, Taipei City, Taiwan Der-Chyuan Lou, Department of Computer Science and Information Engineering, Chang -

The Competitiveness of Taiwan Higher Education
The Competitiveness of Taiwan Higher Education Presented By Wan-Lee Cheng, Ph.D. Chair Professor Chung Yuan Christian University At The Executive Conference on International and Cross- strait Affairs, 2013 June 26, 2013 Presentation Outlines • Taiwan Students Study Abroad (60s, 70s and 80s) • Time for Taiwan Higher Education Institutions to Make Contributions • Quality Assurance of Taiwan Higher Education • Government Investments in Research and Teaching • Uniqueness and Worthiness of Studying in Taiwan • Internationalization of Campuses • Additional Values on University Campuses in Taiwan • Conclusion 2 • The number of study abroad over the years in the 60s 70s and 80s • Overseas scholars returning homeland TAIWAN STUDENTS STUDY ABROAD 3 Taiwan Students Study Abroad Number of people approved to study abroad (A) 215,830 64,216 31,365 21,248 4,515 1950-1959 1960-1969 1970-1979 1980-1989 1990-1998 4 Taiwan Students Study Abroad Number of people return to Taiwan (B) 37,883 14,880 5,166 400 1,172 1950-59 1960-69 1970-79 **1980-1989 **1990-1998 5 Taiwan Students Study Abroad Percentage of return to Taiwan (B) / (A) * 100 23.17 17.55 16.5 8.9 5.5 1950-59 1960-69 1970-79 **1980-1989 **1990-1998 6 Taiwan Students Study Abroad Data from MOE 7 Number of Returning Study Abroad Scholars Employed in Various Sectors 1971-1998 Year Total Employment Assisted by the Youth Commission Self Employed(%) Research University Government Public Private Organizations (%) Teaching (%) Units (%) Businesses (%) Businesses (%) 1971 291 6.5 52.2 10 10.7 5.5 15.1 1972 -

Crustal Structures from the Wuyi-Yunkai Orogen to the Taiwan Orogen: the Onshore-Offshore Wide-Angle Seismic Experiments of the TAIGER and ATSEE Projects
Tectonophysics 692 (2016) 164–180 Contents lists available at ScienceDirect Tectonophysics journal homepage: www.elsevier.com/locate/tecto Crustal structures from the Wuyi-Yunkai orogen to the Taiwan orogen: The onshore-offshore wide-angle seismic experiments of the TAIGER and ATSEE projects Yao-Wen Kuo a,Chien-YingWanga,HaoKuo-Chena,⁎, Xin Jin b,c,Hui-TengCaib,c,Jing-YiLina, Francis T. Wu d, Horng-Yuan Yen a, Bor-Shouh Huang e, Wen-Tzong Liang e, David Okaya f, Larry Brown g a Dept. of Earth Sciences, National Central University, Zhongli, Taiwan b College of Civil Engineering, Fuzhou University, Fuzhou, China c Earthquake Administration of Fujian Province, Fuzhou, China d Dept. of Geological and Environmental Science, State University of New York at Binghamton, Binghamton, USA e Institute of Earth Sciences, Academia Sinica, Taipei, Taiwan f Dept. of Earth Science, University of Southern California, Los Angeles, CA, USA g Dept. of Earth and Atmosphere Science, Cornell University, Ithaca, NY, USA article info abstract Article history: Knowledge of the crustal structure is important for understanding the tectonic framework and geological evolu- Received 8 March 2015 tion of southeastern China and adjacent areas. In this study, we integrated the datasets from the TAIGER (TAiwan Received in revised form 9 August 2015 Integrated GEodynamic Research) and ATSEE (Across Taiwan Strait Explosion Experiment) projects to resolve Accepted 20 September 2015 onshore-offshore deep crustal seismic profiles from the Wuyi-Yunkai orogen to the Taiwan orogen in southeast- Available online 30 September 2015 ern China. Three seismic profiles were resolved, and the longest profile was 850 km. -

Journal of the Taiwan Institute of Chemical Engineers
JOURNAL OF THE TAIWAN INSTITUTE OF CHEMICAL ENGINEERS AUTHOR INFORMATION PACK TABLE OF CONTENTS XXX . • Description p.1 • Impact Factor p.1 • Abstracting and Indexing p.1 • Editorial Board p.1 • Guide for Authors p.3 ISSN: 1876-1070 DESCRIPTION . Journal of the Taiwan Institute of Chemical Engineers (formerly known as Journal of the Chinese Institute of Chemical Engineers) publishes original works, from fundamental principles to practical applications, in the broad field of chemical engineering with special focus on three aspects: Chemical and Biomolecular Science and Technology, Energy and Environmental Science and Technology, and Materials Science and Technology. Authors should choose for their manuscript an appropriate aspect section and a few related classifications when submitting to the journal online. IMPACT FACTOR . 2020: 5.876 © Clarivate Analytics Journal Citation Reports 2021 ABSTRACTING AND INDEXING . Chemical Abstracts INSPEC EDITORIAL BOARD . Editor-in-Chief Heng-Kwong Tsao, National Central University Deputy Editors Dong-Hwang Chen, National Cheng Kung University Yu-Chen Hu, National Tsing Hua University Yung-Chih Kuo, National Chung Cheng University Shing-Yi Suen, National Chung Hsing University Kuo-Lun Tung, National Taiwan University Department of Chemical Engineering Associate Editors Bing-Hung Chen, National Cheng Kung University Chih-Ming Chen, National Chung Hsing University Ruey-Shin Juang, Chang Gung University Dun-Yen Kang, National Taiwan University Department of Chemical Engineering Chien-Liang Lee, National -

A Spatial Analysis
International Journal of Environmental Research and Public Health Article Social Determinants of Diabetes-Related Preventable Hospitalization in Taiwan: A Spatial Analysis Chung-Yi Li 1 , Yung-Chung Chuang 2 , Pei-Chun Chen 3 , Michael S. Chen 4,5, Miaw-Chwen Lee 5 , Li-Jung Elizabeth Ku 1 and Chiachi Bonnie Lee 6,* 1 Department of Public Health, College of Medicine, National Cheng Kung University, Tainan 701401, Taiwan; [email protected] (C.-Y.L.); [email protected] (L.-J.E.K.) 2 Department of Urban Planning and Spatial Information, Feng Chia University, Taichung 407802, Taiwan; [email protected] 3 Department of Public Health, China Medical University, Taichung 40402, Taiwan; [email protected] 4 Department of Healthcare Administration, Asia University, Taichung 41354, Taiwan; [email protected] 5 Department of Social Welfare and Center for Innovative Research on Aging Society, National Chung Cheng University, Chiayi 62102, Taiwan; [email protected] 6 Department of Health Services Administration, China Medical University, Taichung 40402, Taiwan * Correspondence: [email protected] Abstract: Diabetes-Related Preventable Hospitalization (DRPH) has been identified as an important indicator of efficiency and quality of the health system and can be modified by social determinants. However, the spatial disparities, clustering, and relationships between DRPH and social determinants have rarely been investigated. Accordingly, this study examined the association of DRPH with area deprivation, densities of certificated diabetes health-promoting clinics (DHPC) and hospitals (DHPH), Citation: Li, C.-Y.; Chuang, Y.-C.; and the presence of elderly social services (ESS) using both statistical and spatial analyses. -

Epidemiology of Gout in the United Kingdom and Taiwan
Epidemiology of gout in the United Kingdom and Taiwan Kuo, Chang‐Fu Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy December 2014 Abstract Background: Gout is the most common inflammatory arthritis worldwide. The hallmarks of initial gout presentation are acute pain, swelling, erythema and tenderness in peripheral joints but eventually unremitting arthritis, joint deformity and tophus deposition may develop with long‐standing hyperuricaemia. Patients with gout suffer not only arthritis but also cardiovascular, renal, metabolic and other comorbidities. Since gout is the consequence of chronic hyperuricaemia, urate‐lowering treatments (ULT) helps prevent the formation of urate crystals and promote dissolution of existing crystals. Methods: This thesis contained results from a series of observational studies relating to gout. The data sources included the Clinical Practice Research Data‐link in the UK and the National Health Insurance Database in Taiwan, both of which are representative of the general population in these two countries. Six different analyses were carried out: (1) epidemiology of gout in the UK (chapter 3); (2) epidemiology of gout in Taiwan (chapter 4); (3) Nature history of gout following diagnosis in the UK (chapter 5); (4) familial aggregation and heritability of gout in Taiwan (chapter 6); (5) risk of comorbidities occurring before gout diagnosis (chapter 7) and (6) Effects of allopurinol on all‐cause mortality (chapter 8). i Results: This study estimated that the prevalence of gout was 2.49% in the UK in 2012 and 6.24% in Taiwan. Incidence of gout was also higher in Taiwan (3.47 per 1,000 person years in 2010) than in the UK (1.77 per 1,000 person years in 2012). -
2020 TEEP@Asiaplus Programs List
2020 TEEP@AsiaPlus Programs List University / Department / Theme Brief Introduction Contact Person Contact E-Mail More Info College Institute ## Title: Ultrasonic Guidance System and Measurement Stand for Image Analysis of Artificial Intelligence Soft Tissue ## Project objectives and expected benefits: The features of this project focus on the category of biotechnology, smart machinery, and deep learning. Although the Magnetic Resonance Imaging (MRI) images are deliberate to know the location of the soft tissue injury, however, it is not convenient to operate immediately in the clinic. One of the standard clinic measure methods, ultrasound image, is quick and convenient to take in the clinic. However, the scanning angle and posture of the Department of Creative Ultrasound Image, Deep ultrasound probe often affect the image quality and cause difficulty in interpretation. Asia University Dr. Chi-Wen Lung [email protected] Product Design Learning, Soft Tissue. Therefore, the first step of this study will develop an ultrasound probe support system to accuracy the scanning angle and posture. The ultrasound probe support system will be automatically adjusted during different patient scanning processes to improve the scanning quality of the ultrasonic image. The second step of this study will take these benefit quality ultrasonic images to further data analyses in Deep learning. The results of this study would be better to classify the location of soft tissue injury in the clinic. ## Fee and dormitory This project offers $ 500 per person per month. The University can provide paid dormitories (4 beds / room) at a cost of about $ 100 per person per month. This program is a customized study program designed in particular for our sister university students. -
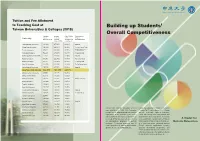
Building up Students' Overall Competitiveness
Tuition and Fee Allotment to Teaching Cost at Building up Students’ Taiwan Universities & Colleges (2018) Overall Competitiveness Standard Average Ratio (Tuition Businesses or University Tuition Teaching and Fees/ Religious andFees (NT$) Cost per Average Cost Group Sponsors Student (NT$) per Student) Taipei Medical University 110,914 477,951 23.21% Hospital Chang Gung University 100,884 408,819 24.68% Formosa Plastics Group Tzu Chi University 90,817 330,959 27.00% Fo Guang University 74,246 215,989 34.37% Fo Guang Shan Kaohsiung Medical University 113,625 273,208 42.00% Hospital Huafan University 97,250 222,862 44.00% Religious Group Nanhua University 91,116 191,562 47.56% Fo Guang Shan Yuan Ze University 112,080 231,538 48.41% The Far Eastern Group China Medical University 107,145 217,531 49.26% Hospital Chung Yuan Christian University 102,534 163,875 62.57% Chinese Culture University 99,093 151,274 65.51% Chung Hua University 96,578 139,963 69.00% Tatung University 104,815 151,611 69.13% Tatung Company Dayeh University 100,042 143,934 69.51% Tunghai University 109,000 153,000 71.20% Feng Chia University 104,720 138,175 76.00% Fu Jen Catholic University 98,229 123,812 79.00% Hospital I-SHOU University 109,687 138,852 79.00% E United Group Tamkang University 98,456 124,259 79.23% Soochow University 102,834 129,458 79.43% Asia University 104,894 129,817 80.80% Hospital Ming Chuan University 97,863 120,723 81.06% Providence University 95,262 111,994 85.06% Chung Yuan Christian University (CYCU) Under the leadership of Chair of the Board Shih Chien University 94,716 110,069 86.05% was established in 1955.