Essential Medicines, Medical Countermeasures, and Critical Inputs for the List Described in Section 3(C) of the Executive Order 13944
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Candida Auris
microorganisms Review Candida auris: Epidemiology, Diagnosis, Pathogenesis, Antifungal Susceptibility, and Infection Control Measures to Combat the Spread of Infections in Healthcare Facilities Suhail Ahmad * and Wadha Alfouzan Department of Microbiology, Faculty of Medicine, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait; [email protected] * Correspondence: [email protected]; Tel.: +965-2463-6503 Abstract: Candida auris, a recently recognized, often multidrug-resistant yeast, has become a sig- nificant fungal pathogen due to its ability to cause invasive infections and outbreaks in healthcare facilities which have been difficult to control and treat. The extraordinary abilities of C. auris to easily contaminate the environment around colonized patients and persist for long periods have recently re- sulted in major outbreaks in many countries. C. auris resists elimination by robust cleaning and other decontamination procedures, likely due to the formation of ‘dry’ biofilms. Susceptible hospitalized patients, particularly those with multiple comorbidities in intensive care settings, acquire C. auris rather easily from close contact with C. auris-infected patients, their environment, or the equipment used on colonized patients, often with fatal consequences. This review highlights the lessons learned from recent studies on the epidemiology, diagnosis, pathogenesis, susceptibility, and molecular basis of resistance to antifungal drugs and infection control measures to combat the spread of C. auris Citation: Ahmad, S.; Alfouzan, W. Candida auris: Epidemiology, infections in healthcare facilities. Particular emphasis is given to interventions aiming to prevent new Diagnosis, Pathogenesis, Antifungal infections in healthcare facilities, including the screening of susceptible patients for colonization; the Susceptibility, and Infection Control cleaning and decontamination of the environment, equipment, and colonized patients; and successful Measures to Combat the Spread of approaches to identify and treat infected patients, particularly during outbreaks. -

NORPRAMIN® (Desipramine Hydrochloride Tablets USP)
NORPRAMIN® (desipramine hydrochloride tablets USP) Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of NORPRAMIN or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. NORPRAMIN is not approved for use in pediatric patients. (See WARNINGS: Clinical Worsening and Suicide Risk, PRECAUTIONS: Information for Patients, and PRECAUTIONS: Pediatric Use.) DESCRIPTION NORPRAMIN® (desipramine hydrochloride USP) is an antidepressant drug of the tricyclic type, and is chemically: 5H-Dibenz[bƒ]azepine-5-propanamine,10,11-dihydro-N-methyl-, monohydrochloride. 1 Reference ID: 3536021 Inactive Ingredients The following inactive ingredients are contained in all dosage strengths: acacia, calcium carbonate, corn starch, D&C Red No. 30 and D&C Yellow No. 10 (except 10 mg and 150 mg), FD&C Blue No. 1 (except 25 mg, 75 mg, and 100 mg), hydrogenated soy oil, iron oxide, light mineral oil, magnesium stearate, mannitol, polyethylene glycol 8000, pregelatinized corn starch, sodium benzoate (except 150 mg), sucrose, talc, titanium dioxide, and other ingredients. -

Mycamine (Micafungin) Safety and Drug Utilization Review
Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Surveillance and Epidemiology Pediatric Postmarketing Pharmacovigilance and Drug Utilization Review Date: February 26, 2016 Safety Evaluator: Timothy Jancel, PharmD, BCPS (AQ-ID) Division of Pharmacovigilance II (DPV II) Drug Use Analyst: LCDR Justin Mathew, PharmD Division of Epidemiology II (DEPI II) Team Leaders: Kelly Cao, PharmD Division of Pharmacovigilance II (DPV II) Rajdeep Gill, PharmD Division of Epidemiology II (DEPI II) Deputy Directors: S. Christopher Jones, PharmD, MS, MPH Division of Pharmacovigilance II (DPV II) LCDR Grace Chai, Pharm.D Division of Epidemiology II (DEPI II) Product Name(s): Mycamine® (micafungin) Pediatric Labeling Approval Date: June 21, 2013 Application Type/Number: NDA 021506 Applicant/Sponsor: Astellas OSE RCM #: 2015-1945 **This document contains proprietary drug use data obtained by FDA under contract. The drug use data/information cannot be released to the public/non-FDA personnel without contractor approval obtained through the FDA/CDER Office of Surveillance and Epidemiology.** Reference ID: 3893564 TABLE OF CONTENTS Executive Summary.........................................................................................................................3 1 Introduction..............................................................................................................................4 1.1 Pediatric Regulatory History.............................................................................................4 -

Oral Anticoagulants
4/26/2018 Disclosure • Kelsey Gander, PharmD, BCACP Direct Oral Anticoagulants: – Declares no financial relationships pertinent to this session When to Use and How to Choose – Declares off-label use of medication will not be discussed during this presentation. Kelsey Gander, PharmD, BCACP Minnesota Academy of Physician Assistants Conference May 11th, 2018 Abbreviations Objectives • DOAC= direct oral anticoagulant 1) Compare and contrast the efficacy and safety • VTE= venous thromboembolism • DVT= deep vein thrombosis of direct oral anticoagulants (DOACs) to • PE= pulmonary embolism warfarin • A-fib, AF= atrial fibrillation 2) Identify which anticoagulant would be most • ESRD= end stage renal disease appropriate for a given patient • ACC= American College of Cardiology • AHA= American Heart Association 3) Recognize when it would not be appropriate • HRS= Heart Rhythm Society to use a DOAC • BID= twice daily Appropriate Abbreviations Patient Case JJ is a 66 y/o male who was hospitalized for pulmonary • NOAC embolism and initiated on anticoagulant therapy one week – Novel Oral Anticoagulant ago. – Chief complaint: – Non-Vitamin K Oral Anticoagulant • Presents to clinic today for INR check, post-hospital discharge follow- up • TSOAC – Past medical history: • Hypertension, hyperlipidemia, osteoarthritis, erectile dysfunction, – Target Specific Oral Anticoagulant BPH, type 2 diabetes, peripheral artery disease – Home medications • DOAC • Acetaminophen 650mg po every 6 hours PRN – Direct Oral Anticoagulant • Diazepam 5mg po at bedtime PRN anxiety -

Sulfhydryl Reduction of Methylene Blue with Reference to Alterations in Malignant Neoplastic Disease
Sulfhydryl Reduction of Methylene Blue With Reference to Alterations in Malignant Neoplastic Disease Maurice M. Black, M. D. (From the Department of Biochemistry, New York Medical College, New York 29, N. t;., and the Brooklyn Cancer Institute, Brooklyn 9, N. Y.) (Received for publication May 8, 1947) A significant decrease in methylene blue re- reactivity is less than half that of the cysteine. It is ducing power of plasma from patients with malig- noteworthy also that the resultant leuco mixture nant neoplastic disease was previously reported did not revert back to colored methylene blue on (1). At that time it was suggested that change in a cooling, as was the case with methylene blue re- reducing group of the albumin molecule was a duction by plasma. likely source of this alteration. Similar conclusions Similar relationships were investigated between were reported also by Savignac and associates (7) cysteine and different concentrations of methylene as the result of analogous studies. blue. As seen in Fig. 2, similar curves are obtained, In an attempt to evaluate the effect of the sulf- but the position of the curve on the graph varies hydryl group on the reduction of methylene blue, a with the concentration of the methylene blue used. study was undertaken with various compounds of It should be noted that there is no appreciable known -SH and S-S structures. In addition, an difference in the reducing time of methylene blue attempt was made to establish a standard method on varying the concentrations between 0.10 per of calibration of various lots of methylene blue, so cent and 0.2 per cent, although 0.08 per cent shows that more uniform results would be possible in the a decided difference. -

Guideline on Antidote Availability for Emergency Departments January 2017
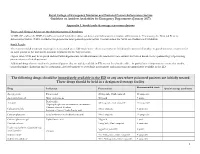
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments January 2017 TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration and, if necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide dinitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated. These drugs should be held in a designated storage facility* The stock held should be sufficient to initiate treatment (stocking guidance is in Appendix 1). Drug Indication Acetylcysteine Paracetamol Activated charcoal Many oral poisons Atropine Organophosphorus or carbamate insecticides Bradycardia Calcium chloride Calcium channel blockers Systemic effects of hydrofluoric acid Calcium gluconate Local infiltration for hydrofluoric acid Calcium gluconate gel Hydrofluoric acid Cyanide antidotes Cyanide Dicobalt edetate The choice of antidote depends on the severity of poisoning, certainty of diagnosis and cause Hydroxocobalamin (Cyanokit®) of poisoning/source of cyanide. Sodium nitrite - Dicobalt edetate is the antidote of choice in severe cases when there is a high clinical Sodium thiosulphate suspicion of cyanide poisoning e.g. after cyanide salt exposure. - Hydroxocobalamin (Cyanokit®) should be considered in smoke inhalation victims who have a severe lactic acidosis, are comatose, in cardiac arrest or have significant cardiovascular compromise - Sodium nitrite may be used if dicobalt edetate is not available. -

Geisinger Lewistown Hospital Published: March 25, 2019
Geisinger Lewistown Hospital Published: March 25, 2019 DESCRIPTION CHARGE Fine needle aspiration; without imaging guidance $ 607.00 Fine needle aspiration; without imaging guidance $ 286.00 Fine needle aspiration; with imaging guidance $ 2,218.00 Fine needle aspiration; with imaging guidance $ 1,691.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; first lesion $ 1,979.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; each $ 1,385.00 additional lesion (List separately in addition to code for primary procedure) Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); simple or single $ 657.00 Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); complicated or $ 986.00 multiple Incision and drainage of pilonidal cyst; simple $ 657.00 Incision and drainage of pilonidal cyst; complicated $ 3,726.00 Incision and removal of foreign body, subcutaneous tissues; simple $ 1,694.00 Incision and removal of foreign body, subcutaneous tissues; complicated $ 4,710.00 Incision and drainage of hematoma, seroma or fluid collection $ 3,470.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 1,272.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 657.00 Incision -

The Neosartorya Fischeri Antifungal Protein 2 (NFAP2)
International Journal of Molecular Sciences Article The Neosartorya fischeri Antifungal Protein 2 (NFAP2): A New Potential Weapon against Multidrug-Resistant Candida auris Biofilms Renátó Kovács 1,2,3,* , Fruzsina Nagy 1,4, Zoltán Tóth 1,4,5, Lajos Forgács 1,4, Liliána Tóth 6,7, Györgyi Váradi 8, Gábor K. Tóth 8,9, Karina Vadászi 1, Andrew M. Borman 10,11 ,László Majoros 1 and László Galgóczy 6,7 1 Department of Medical Microbiology, Faculty of Medicine, University of Debrecen, Nagyerdei krt. 98, 4032 Debrecen, Hungary; [email protected] (F.N.); [email protected] (Z.T.); [email protected] (L.F.); [email protected] (K.V.); [email protected] (L.M.) 2 Faculty of Pharmacy, University of Debrecen, Nagyerdei krt. 98, 4032 Debrecen, Hungary 3 Department of Metagenomics, University of Debrecen, Nagyerdei krt. 98, 4032 Debrecen, Hungary 4 Doctoral School of Pharmaceutical Sciences, University of Debrecen, Nagyerdei krt. 98, 4032 Debrecen, Hungary 5 Department of Pharmacology and Pharmacotherapy, Faculty of Medicine, University of Debrecen, Nagyerdei krt. 98, 4032 Debrecen, Hungary 6 Institute of Plant Biology, Biological Research Centre, Temesvári krt. 62, 6726 Szeged, Hungary; [email protected] (L.T.); [email protected] (L.G.) 7 Department of Biotechnology, Faculty of Science and Informatics, University of Szeged, Közép fasor 52, 6726 Szeged, Hungary 8 Department of Medical Chemistry, Faculty of Medicine, University of Szeged, Dóm tér 8, 6720 Szeged, Hungary; [email protected] (G.V.); [email protected] -
RCEM NPIS Antidote Guideline Appx 1
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions -

Revista Brasileira De Anestesiologia
Rev BrasBras Anestesiol. Anestesiol. 2013;63(1):163–164 2013;63(1):163-166 REVISTA BRASILEIRA DE ANESTESIOLOGIA Offi cial Publication of the Brazilian Society of Anesthesiology www.sba.com.br/rba/index.asp LETTER TO THE EDITOR Precipitation in Gallipoli: Sugammadex / Amiodarone & Sugammadex / Dobutamine & Sugammadex / Protamine Dear Editor, furosemide (10 mg.mL-1), gentamicin (40 mg.mL-1), glyceryl Sugammadex is a modifi ed gamma cyclodextrin 1-3. Cyclodextrins trinitrate (5 mg.mL-1), heparin (1,000 IU.mL-1), hydrocor- are water soluble cyclic oligosaccharides with a lipophilic tisone (250 mg.mL-1), crystallized insulin (100 IU.mL-1), core. Sugammadex has quickly found a place in clinical use Calcium (Calcium Gluconate Monohydrate 225 mg.10 mL-1 for selective antagonism of neuromuscular blockade with ro- + Calcium levulinate dihitrate 572 mg.10 mL-1), ketamine curonium 1-3. Sugammadex quickly encapsulates steroidal neu- (50 mg.mL-1), levobupivacaine (7.5 mg.mL-1), magnesium romuscular blockers, increasing the amount of encapsulated sulphate (1.2 mEq.mL-1), metamizol sodium (0.5 g.mL-1), steroidal neuromuscular blockers in plasma and separating the methylergobasin maleate (0.2 mg.mL-1), metoclopramide blockers from the nicotinic acetylcholine receptors 1-3. (5 mg.mL-1), metoprolol (1 mg.mL-1), morphine (0.01 g.mL-1), Apart from its use with steroidal neuromuscular block- midazolam (5 mg.mL-1), n-acetylcysteine (100 mg.mL-1), ers, it is known that sugammadex interacts with over 40 naloxone (0.4 mg.mL-1), neostigmine (0.5 mg.mL-1), nitroprus- lipophilic, steroidal and non-steroidal drugs. -

76. Which of the Following Is Incorrect Based on the 2018 ASRA Checklist for Managing Local Anesthetic Systemic Toxicity?
76. Which of the following is incorrect based on the 2018 ASRA Checklist for managing Local Anesthetic Systemic Toxicity? A. The upper limit of lipid emulsion dosing is 12mL/kg B. Monitoring should be at least 4-6 hours after a cardiovascular event or at least 2 hours after a limited CNS event C. 20% lipid emulsion should be used as the initial drug at the first sign of a serious LAST Event D. Epinephrine doses of > 1mcg/kg are recommended 77. Which of the following statements is NOT true with regard to the management of new oral anticoagulants? A. Rivaroxaban (Xarelto) and Apixaban (Eliquis) should be held for at least 72 hours prior to neuraxial block B. Dabigatran (Pradaxa) should be held for 24 to 48 hours prior to neuraxial block in a patient with a compromised GFR C. Dabigatran can be reversed by the monoclonal antibody idarucizumab D. Factor Xa inhibitors, Rivaroxaban and Apixaban, can be effectivelY reversed with andexanet alfa 78. Which answer the correct spread of local anesthetic for an Erector Spinae Plane Block performed at the T5 level? A. Spread between the erector spinae muscle and rhomboid muscle B. Spread lateral to the transverse process, superficial to the erector spinae muscle C. Spread deep to the erector spinae muscle at the transverse process D. Spread deep to the costotransverse ligament, pushing the pleura ventrallY 79. When assessing the lungs with ultrasound, which of the following signs are suggestive a pneumothorax: A. Absence of lung sliding B. Presence of “comet tails” C. Absence of a “lung point” D.