Anesthetic Considerations for the Parturient with Idiopathic Intracranial Hypertension Levi G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evidence Based Answers to Clinical Questions for Busy Clinicians
Evidence-Based Answers to Clinical Questions for Busy Clinicians Workbook Harris C & Turner T 2011 Updated 2018 This publication should be cited as: Harris C & Turner T. Evidence-Based Answers to Clinical Questions for Busy Clinicians. (2011) The Centre for Clinical Effectiveness, Monash Health, Melbourne, Australia. Copyright © This publication is the copyright of Monash Health. Other than for the purposes and subject to the conditions prescribed under the Copyright Act 1968 as amended, no part of this publication may, in any form or by any means (electric, mechanical, microcopying, photocopying, recording or otherwise), be reproduced, stored in a retrieval system or transmitted without prior written permission. Inquiries should be addressed to Centre for Clinical Effectiveness. Acknowledgements The authors would like to acknowledge past and present staff of the Centre for Clinical Effectiveness at Monash Health for their contributions towards the development of this resource. Centre for Clinical Effectiveness Monash Health Phone: +61 3 9594 7575 Fax: +61 3 9594 6018 Email: [email protected] Web : www.monashhealth.org/cce Evidence-Based Answers to Clinical Questions for Busy Clinicians Workbook 2 Objectives This workbook aims to help you to find the best available evidence to answer your clinical questions, in the shortest possible time. It will introduce the principles of evidence-based practice and provide a foundation of understanding and skills in: o Developing questions that are answerable from the literature o Searching for and identifying evidence to answer your question o Appraising the evidence identified for quality, reliability, accuracy and relevance Contents page 1. What is evidence-based practice? 4 2. -

Geisinger Lewistown Hospital Published: March 25, 2019
Geisinger Lewistown Hospital Published: March 25, 2019 DESCRIPTION CHARGE Fine needle aspiration; without imaging guidance $ 607.00 Fine needle aspiration; without imaging guidance $ 286.00 Fine needle aspiration; with imaging guidance $ 2,218.00 Fine needle aspiration; with imaging guidance $ 1,691.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; first lesion $ 1,979.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; each $ 1,385.00 additional lesion (List separately in addition to code for primary procedure) Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); simple or single $ 657.00 Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); complicated or $ 986.00 multiple Incision and drainage of pilonidal cyst; simple $ 657.00 Incision and drainage of pilonidal cyst; complicated $ 3,726.00 Incision and removal of foreign body, subcutaneous tissues; simple $ 1,694.00 Incision and removal of foreign body, subcutaneous tissues; complicated $ 4,710.00 Incision and drainage of hematoma, seroma or fluid collection $ 3,470.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 1,272.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 657.00 Incision -
Application of the PICO Process to Plan Treatment for a Child with a Co-Occurring Stuttering and Phonological Disorder
Volume 8, Issue 6 March 2014 EBP briefs A scholarly forum for guiding evidence-based practices in speech-language pathology Application of the PICO Process to Plan Treatment for a Child With a Co-occurring Stuttering and Phonological Disorder Keegan M. Koehlinger Linda Louko Patricia Zebrowski EBP Briefs Editor Laura Justice The Ohio State University Associate Editor Mary Beth Schmitt The Ohio State University Editorial Review Board Tim Brackenbury Lisa Milman Bowling Green State University Utah State University Jayne Brandel Cynthia O’Donoghue Fort Hays State University James Madison University Kathy Clapsaddle Amy Pratt Private Practice (Texas) The Ohio State University Lynn Flahive Nicole Sparapani Texas Christian University Florida State University Managing Director Tina Eichstadt Pearson 5601 Green Valley Drive Bloomington, MN 55437 Cite this document as: Koehlinger, K. M., Louko, L., & Zebrowski, P. (2014). Application of the PICO process to plan treatment for a child with a co-occurring stuttering and phonological disorder. EBP Briefs, 8(6), 1–9. Bloomington, MN: Pearson. Copyright © 2014 NCS Pearson, Inc. All rights reserved. Warning: No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without the express written permission of the copyright owner. Pearson, PSI design, and PsychCorp are trademarks, in the US and/or other countries, of Pearson Education, Inc., or its affiliate(s). NCS Pearson, Inc. 5601 Green Valley Drive Bloomington, MN 55437 800.627.7271 www.PearsonClinical.com Produced in the United States of America. 1 2 3 4 5 6 7 8 9 10 11 12 A B C D E Application of the PICO Process to Plan Treatment for a Child With a Co-occurring Stuttering and Phonological Disorder Keegan M. -
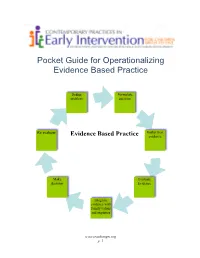
Pocket Guide for Operationalizing Evidence Based Practice
Pocket Guide for Operationalizing Evidence Based Practice Define Formulate problem question Re evaluate Gather best Evidence Based Practice evidence Make Evaluate decision Evidence Integrate evidence with family values and expertise www.teachinngei.org p. 1 Define the Problem When a service provider is attempting to understand a new problem, often their questions are broad making it difficult to gather information to inform decisions. Narrowing the problem to certain element gives the best starting point in a search for evidence. Formulate the Question A well constructed question makes the search for evidence easier and more efficient. A good question should contain the specific group or population, the intervention or issue being addressed/ compared and the desired outcome. Gathering the Best Evidence Many sources of evidence come together to inform decisions made about practice. It is important to have the skills and strategies to make timely and effective decisions. Sources of best evidence include • Information sources: publications, databases, web sites, laws and policies • Service provider experience and expertise • Family values, beliefs, priorities and concerns Information Sources: 1. Publications There are a wide range of publications available with information about practice across disciplines in early childhood. Scholarly publications are the most likely to yield accurate information needed to make decisions. These sources include: o Peer-reviewed journals o Research articles o Guidelines and recommended practices o Systematic reviews and Meta-analysis o Books o Reports o Magazines, non- peer reviewed journals 1a. Peer Reviewed Information Information from peer-reviewed or refereed publications is considered high quality because the process to publish requires the scrutiny of experts in the field as well as scientific methods. -

This Electronic Thesis Or Dissertation Has Been Downloaded from the King’S Research Portal At
This electronic thesis or dissertation has been downloaded from the King’s Research Portal at https://kclpure.kcl.ac.uk/portal/ Clinical Judgement in the era of Evidence Based Medicine Flores Sepulveda, Luis Jose Awarding institution: King's College London The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without proper acknowledgement. END USER LICENCE AGREEMENT This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International licence. https://creativecommons.org/licenses/by-nc-nd/4.0/ You are free to: Share: to copy, distribute and transmit the work Under the following conditions: Attribution: You must attribute the work in the manner specified by the author (but not in any way that suggests that they endorse you or your use of the work). Non Commercial: You may not use this work for commercial purposes. No Derivative Works - You may not alter, transform, or build upon this work. Any of these conditions can be waived if you receive permission from the author. Your fair dealings and other rights are in no way affected by the above. Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 06. Nov. 2017 Clinical judgment in the era of Evidence Based Medicine Submitted to the Department of Philosophy of King’s College London, in partial fulfilment of the requirements for the degree of Doctor of philosophy Luis Flores MD. -

This Is the Title of My Thesis
A Systematic Review of the Effectiveness of Interventions (Pharmaceutical and Psychosocial) for Cognitive and Learning Impairments in Children Diagnosed with a Brain Tumour Lisa-Jane Keegan Submitted in accordance with the requirements for the degree of Doctor of Clinical Psychology (D. Clin. Psychol.) The University of Leeds School of Medicine Academic Unit of Psychiatry and Behavioural Sciences September 2014 The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. © 2014 The University of Leeds and Lisa-Jane Keegan (Optional) The right of Lisa-Jane Keegan to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988 2 ACKNOWLEDGEMENTS I am sincerely grateful for the help of Professor Stephen Morley and Dr Matthew Morrall, without their support, time and patience this thesis would never have been possible. A big thank you to Miss Rosa Reed-Berendt (Research Assistant), Mr Paul Farrington (Psychologist in Forensic Training), Miss Elizabeth Neilly – Health Faculty Team Librarian, Ms Janet Morton – Education Faculty Team Librarian, Drs Picton, Wilkins and Elliott - Consultant Paediatric Oncologists, Dr Livingston - Consultant Paediatric Neurologist at The Leeds Teaching Hospitals NHS Trust, Miss Helen Stocks, Miss Kate Ablett and Dr Stanley, Consultant Child & Adolescent Psychiatrist, Leeds Community Healthcare NHS Trust, Suzanne Donald (Honorary Research Assistant) and Michael Ferriter- Lead for Research, Forensic Division, Nottinghamshire Healthcare NHS Trust; who have supported me to achieve my goal. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Sugammadex Reversal of Rocuronium-Induced Neuromuscular Blockade: a Comparison with Neostigmine–Glycopyrrolate and Edrophonium–Atropine
Sugammadex Reversal of Rocuronium-Induced Neuromuscular Blockade: A Comparison with Neostigmine–Glycopyrrolate and Edrophonium–Atropine Ozlem Sacan, MD BACKGROUND: Sugammadex is a modified ␥ cyclodextrin compound, which encap- sulates rocuronium to provide for a rapid reversal of residual neuromuscular Paul F. White, MD, PhD blockade. We tested the hypothesis that sugammadex would provide for a more rapid reversal of a moderately profound residual rocuronium-induced blockade Burcu Tufanogullari, MD than the commonly used cholinesterase inhibitors, edrophonium and neostigmine. METHODS: Sixty patients undergoing elective surgery procedures with a standard- ized desflurane–remifentanil–rocuronium anesthetic technique received either Kevin Klein, MD sugammadex, 4 mg/kg IV (n ϭ 20), edrophonium, 1 mg/kg IV and atropine, 10 g/kg IV (n ϭ 20), or neostigmine, 70 g/kg IV and glycopyrrolate, 14 g/kg IV (n ϭ 20) for reversal of neuromuscular blockade at 15 min or longer after the last dose of rocuronium using acceleromyography to record the train-of-four (TOF) responses. Mean arterial blood pressure and heart rate values were recorded immediately before and for 30 min after reversal drug administration. Side effects were noted at discharge from the postanesthesia care unit. RESULTS: The three groups were similar with respect to their demographic character- istics and total dosages of rocuronium prior to administering the study medication. Although the initial twitch heights (T1) at the time of reversal were similar in all three groups, the time to achieve TOF ratios of 0.7 and 0.9 were significantly shorter with sugammadex (71 Ϯ 25 and 107 Ϯ 61 s) than edrophonium (202 Ϯ 171 and 331 Ϯ 27 s) or neostigmine (625 Ϯ 341 and 1044 Ϯ 590 s). -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD May 2016 CONTENTS General Toxicology 8 Metals 33 Management 16 Pesticides 35 Drugs 19 Chemical Warfare 37 Chemical Incidents & 28 Plants 37 Pollution Chemicals 29 Animals 38 CURRENT AWARENESS PAPERS OF THE MONTH Efficacy and effectiveness of anti-digoxin antibodies in chronic digoxin poisonings from the DORA study (ATOM-1) Chan BS, Isbister GK, O'Leary M, Chiew A, Buckley NA. Clin Toxicol 2016; online early: doi: 10.1080/15563650.2016.1175620: Context We hypothesized that in chronic digoxin toxicity, anti-digoxin antibodies (Fab) would be efficacious in binding digoxin, but this may not translate into improved clinical outcomes. Objective This study aims to investigate changes in free digoxin concentrations and clinical effects on heart rate and potassium concentrations in chronic digoxin poisoning when anti-digoxin Fab are given. Materials and methods This is a prospective observational study. Patients were recruited if they have been treated with anti-digoxin Fab for chronic digoxin poisoning. Data was entered into a standardised prospective form, supplemented with medical records. Their serum or plasma was collected, analysed for free and bound digoxin and free anti-digoxin Fab concentrations. Results From September 2013 to February 2015, 36 patients (median age, 78 years; 22 females) Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England 2 were recruited from 18 hospitals. -

Evidence-Based Practice Special Interest Group Section on Research
EVIDENCE-BASED PRACTICE SPECIAL INTEREST GROUP SECTION ON RESEARCH AMERICAN PHYSICAL THERAPY ASSOCIATION DOCTOR OF PHYSICAL THERAPY EDUCATION EVIDENCE-BASED PRACTICE CURRICULUM GUIDELINES March 2014 Task Force Chairs: David Levine, PT, PhD, DPT, OCS Julie K. Tilson, PT, DPT, MS, NCS Professor and Walter M. Cline Chair Associate Professor of Clinical Physical Therapy of Excellence in Physical Therapy University of Southern California, The University of Tennessee at Chattanooga, Los Angeles, CA Chattanooga, TN Task Force Members: Deanne Fay, PT, DPT, MS, PCS Dianne Jewell, PT, DPT, PhD, FAACVPR Associate Professor and Director of Founder and CEO Curriculum The Rehab Intel Network, Consulting Physical Therapy Program Services, Ruther Glen, VA Arizona School of Health Sciences A.T. Still University, Mesa, AZ Sandra Kaplan PT, DPT, PhD Professor and Director of Post Professional Steven George PT, PhD Education Associate Professor and Assistant Doctoral Programs in Physical Therapy, Department Chair Newark Campus Director, Doctor of Physical Therapy Rutgers University, Newark, NJ Program Director, Brooks-PHHP Research Randy Richter, PT, PhD Collaboration Professor, Program in Physical Therapy University of Florida, Gainesville FL Saint Louis University, Saint Louis, MO Laurita Hack, PT, DPT, MBA, PhD, Robert Wainner, PT, PhD FAPTA Associate Professor, Dept. of Physical Professor Emeritus, Therapy Department of Physical Therapy Texas State University, TX Temple University, Bryn Mawr, PA Evidence Based Practice Special Interest Group, American -

Effects of Sugammadex on Post-Operative Pulmonary
Journal of Clinical Medicine Article Effects of Sugammadex on Post-Operative Pulmonary Complications in Laparoscopic Gastrectomy: A Retrospective Cohort Study Jiwon Han 1, Jung-Hee Ryu 1,2 , Bon-Wook Koo 1, Sun Woo Nam 1, Sang-Il Cho 1 and Ah-Young Oh 1,2,* 1 Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, 82, Gumi-ro, Bundang-gu, Seongnam-si, Gyeonggi-do 13620, Korea; [email protected] (J.H.); [email protected] (J.-H.R.); [email protected] (B.-W.K.); [email protected] (S.W.N.); [email protected] (S.-I.C.) 2 Department of Anesthesiology and Pain Medicine, Seoul National University College of Medicine, 103, Daehak-ro, Jongno-gu, Seoul 03080, Korea * Correspondence: [email protected]; Tel.: +82-31-787-7506 Received: 10 April 2020; Accepted: 23 April 2020; Published: 24 April 2020 Abstract: The use of sugammadex can reduce post-operative residual neuromuscular blockade, which is known to increase the risk of post-operative respiratory events. However, its effect on post-operative pulmonary complications is not obvious. This study was performed to evaluate the effects of sugammadex on post-operative pulmonary complications in patients undergoing laparoscopic gastrectomy between 2013 and 2017. We performed propensity score matching to correct for selection bias. Post-operative pulmonary complications (i.e., pneumonia, respiratory failure, pleural effusion, atelectasis, pneumothorax, and aspiration pneumonitis) were evaluated from the radiological and laboratory findings. We also evaluated admission to the intensive care unit after surgery, re-admission or an emergency room visit within 30 days after discharge, length of hospital stay, re-operation, and mortality within 90 days post-operatively as secondary outcomes. -

Queensland Health List of Approved Medicines
Queensland Health List of Approved Medicines Drug Form Strength Restriction abacavir * For use in accord with PBS Section 100 indications * oral liquid See above 20 mg/mL See above tablet See above 300 mg See above abacavir + lamivudine * For use in accord with PBS Section 100 indications * tablet See above 600 mg + 300 mg See above abacavir + lamivudine + * For use in accord with PBS Section 100 indications * zidovudine tablet See above 300 mg + 150 mg + 300 mg See above abatacept injection 250 mg * For use in accord with PBS Section 100 indications * abciximab (a) Interventional Cardiologists for complex angioplasty (b) Interventional and Neuro-interventional Radiologists for rescue treatment of thromboembolic events that occur during neuroendovascular procedures. * Where a medicine is not TGA approved, patients should be made fully aware of the status of the medicine and appropriate consent obtained * injection See above 10 mg/5 mL See above abiraterone For use by medical oncologists as per the PBS indications for outpatient and discharge use only tablet See above 250 mg See above 500 mg See above acamprosate Drug and alcohol treatment physicians for use with a comprehensive treatment program for alcohol dependence with the goal of maintaining abstinence. enteric tablet See above 333 mg See above acarbose For non-insulin dependent diabetics with inadequate control despite diet; exercise and maximal tolerated doses of other anti-diabetic agents tablet See above 50 mg See above 100 mg See above acetazolamide injection 500 mg tablet 250 mg acetic acid ear drops 3% 15mL solution 2% 100mL green 3% 1 litre 6% 1 Litre 6% 200mL Generated on: 30-Aug-2021 Page 1 of 142 Drug Form Strength Restriction acetylcysteine injection For management of paracetamol overdose 2 g/10 mL See above 6 g/30 mL See above aciclovir cream Infectious disease physicians, haematologists and oncologists 5% See above eye ointment For use on the advice of Ophthalmologists only.