Effect of Targeting Inflammation with Salsalate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Salsalate Tablets, USP 500 Mg and 750 Mg Rx Only
SALSALATE RX- salsalate tablet, film coated ANDAPharm LLC Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here. ---------- Salsalate Tablets, USP 500 mg and 750 mg Rx Only Cardiovascular Risk NSAIDs may cause an increase risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (See WARNINGS and CLINICAL TRIALS). Salsalate tablets, USP is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery (See WARNINGS). Gastrointestinal Risk NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS). DESCRIPTION Salsalate, is a nonsteroidal anti-inflammatory agent for oral administration. Chemically, salsalate (salicylsalicylic acid or 2-hydroxybenzoic acid, 2-carboxyphenyl ester) is a dimer of salicylic acid; its structural formula is shown below. Chemical Structure: Inactive Ingredients: Colloidal Silicon Dioxide, D&C Yellow #10 Aluminum Lake, Hypromellose, Microcrystalline Cellulose, Sodium Starch Glycolate, Stearic Acid, Talc, Titanium Dioxide, Triacetin. CLINICAL PHARMACOLOGY Salsalate is insoluble in acid gastric fluids (<0.1 mg/mL at pH 1.0), but readily soluble in the small intestine where it is partially hydrolyzed to two molecules of salicylic acid. -
Download Product Insert (PDF)
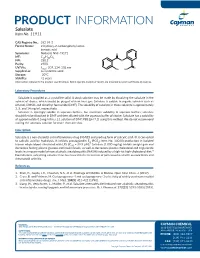
PRODUCT INFORMATION Salsalate Item No. 11911 CAS Registry No.: 552-94-3 Formal Name: 2-hydroxy-2-carboxyphenyl ester- benzoic acid Synonyms: Nobacid, NSC 49171 O MF: C14H10O5 FW: 258.2 O Purity: ≥98% UV/Vis.: λ: 207, 234, 308 nm O max OH HO Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Salsalate is supplied as a crystalline solid. A stock solution may be made by dissolving the salsalate in the solvent of choice, which should be purged with an inert gas. Salsalate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of salsalate in these solvents is approximately 3, 5, and 14 mg/ml, respectively. Salsalate is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, salsalate should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Salsalate has a solubility of approximately 0.5 mg/ml in a 1:1 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description Salsalate is a non-steroidal anti-inflammatory drug (NSAID) and prodrug form of salicylic acid.1 It is converted to salicylic acid by hydrolysis. It inhibits prostaglandin E2 (PGE2; Item No. 14010) production in isolated 2 human whole blood stimulated with LPS (IC50 = 39.9 µM). Salsalate (1,000 mg/kg) inhibits weight gain and decreases fasting plasma glucose and insulin levels, as well as decreases plasma cholesterol and triglyceride levels in a mouse model of non-alcoholic steatohepatitis (NASH) induced by a high-fat high-cholesterol diet.3 Formulations containing salsalate have been used in the treatment of pain associated with osteoarthritis and rheumatoid arthritis. -

Salicylate, Diflunisal and Their Metabolites Inhibit CBP/P300 and Exhibit Anticancer Activity
RESEARCH ARTICLE Salicylate, diflunisal and their metabolites inhibit CBP/p300 and exhibit anticancer activity Kotaro Shirakawa1,2,3,4, Lan Wang5,6, Na Man5,6, Jasna Maksimoska7,8, Alexander W Sorum9, Hyung W Lim1,2, Intelly S Lee1,2, Tadahiro Shimazu1,2, John C Newman1,2, Sebastian Schro¨ der1,2, Melanie Ott1,2, Ronen Marmorstein7,8, Jordan Meier9, Stephen Nimer5,6, Eric Verdin1,2* 1Gladstone Institutes, University of California, San Francisco, United States; 2Department of Medicine, University of California, San Francisco, United States; 3Department of Hematology and Oncology, Kyoto University, Kyoto, Japan; 4Graduate School of Medicine, Kyoto University, Kyoto, Japan; 5University of Miami, Gables, United States; 6Sylvester Comprehensive Cancer Center, Miami, United States; 7Perelman School of Medicine, University of Pennsylvania, Philadelphia, United States; 8Department of Biochemistry and Biophysics, Abramson Family Cancer Research Institute, Philadelphia, United States; 9Chemical Biology Laboratory, National Cancer Institute, Frederick, United States Abstract Salicylate and acetylsalicylic acid are potent and widely used anti-inflammatory drugs. They are thought to exert their therapeutic effects through multiple mechanisms, including the inhibition of cyclo-oxygenases, modulation of NF-kB activity, and direct activation of AMPK. However, the full spectrum of their activities is incompletely understood. Here we show that salicylate specifically inhibits CBP and p300 lysine acetyltransferase activity in vitro by direct *For correspondence: everdin@ competition with acetyl-Coenzyme A at the catalytic site. We used a chemical structure-similarity gladstone.ucsf.edu search to identify another anti-inflammatory drug, diflunisal, that inhibits p300 more potently than salicylate. At concentrations attainable in human plasma after oral administration, both salicylate Competing interests: The and diflunisal blocked the acetylation of lysine residues on histone and non-histone proteins in cells. -

Medications & Supplements to Avoid Before Procedures
Medications & Supplements to Avoid Before Procedures Do not ingest any brand of aspirin, or any aspirin-containing medication, any MAO inhibiting, or any serotonin medications, for 14 prior to and 14 days after surgery. Disclose every medication, supplement, etc. With Dr. Rau and your anesthesiologist. Aspirin and aspirin-containing products, as well as some supplements and herbals, may inhibit blood clotting and cause difficulties during and after surgery. If you need an aspirin-free fever reducer and pain reliever, take Tylenol. Also, if you smoke, you must refrain for at least a month prior to a month after your surgery date. Smoking significantly reduces your body’s circulation and vascularity, meaning that your tissues won’t receive all the oxygen needed for proper healing. DIET PILLS, FAT LOSS SUPPLEMENTS AND STACKERS: Please stop taking these pills at least 2 weeks before surgery. Many of these pills contain anticoagulants and can seriously impede your body's ability to clot sufficiently, resulting in hemorrhaging. Many of them also contain ephedra and caffeine, which can affect your anesthetic medications. Remember: if you take antibiotics or if you stop oral contraceptive pills for surgery, use an alternative method of birth control. A Aspirin, Advil, Actifed, Acuprin, Addaprin, Alka Seltzer, Alpha Omega (fish oil), Aluprin, Amitriptyline, Anacin, Ansaid, Anodynos, Analval, Anodynos, Ansaid, Argesic, Arthra-G, Arthralgen, Arthropan, Ascodeen, Ascriptin, Aspir-lox, Asperi-mox, Aspirbuf, Aspercin, Aspergum, Axotal, Azdone, -

Arthritis Treatment Comparison Arthritis Treatment Comparison
ARTHRITIS TREATMENT COMPARISON ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA CHELATING AGENTS Penicillamine Cap: 250mg ✓ (Cuprimine) Penicillamine Tab: 250mg ✓ (Depen) CYCLIC POLYPEPTIDE IMMUNOSUPPRESSANTS Cyclosporine Cap: 25mg, 100mg; ✓ (Gengraf, Neoral) Sol: 100mg/mL CYCLOOXYGENASE-2 INHIBITORS Celecoxib Cap: 50mg, 100mg, ✓ ✓ ✓ ✓ (Celebrex) 200mg, 400mg DIHYDROFOLIC ACID REDUCTASE INHIBITORS Methotrexate Inj: 25mg/mL; ✓ ✓ Tab: 2.5mg Methotrexate Tab: 5mg, 7.5mg, ✓ ✓ (Trexall) 10mg, 15mg INTERLEUKIN RECEPTOR ANTAGONISTS Anakinra Inj: 100mg/0.67mL ✓ (Kineret) Tocilizumab Inj: 20mg/mL, ✓ ✓ (Actemra) 162mg/0.9mL GOLD COMPOUNDS Auranofin Cap: 3mg ✓ (Ridaura) Gold sodium thiomalate Inj: 50mg/mL ✓ ✓ (Myochrysine) HYALURONAN AND DERIVATIVES Hyaluronan Inj: 30mg/2mL ✓ (Orthovisc) Sodium hyaluronate Inj: 1% ✓ (Euflexxa) Sodium hyaluronate Inj: 10mg/mL ✓ (Hyalgan) Sodium hyaluronate Inj: 2.5mL ✓ (Supartz) HYLAN POLYMERS Hylan G-F 20 Inj: 8mg/mL ✓ (Synvisc, Synvisc One) KINASE INHIBITORS Tofacitinib Tab: 5mg ✓ (Xeljanz) MONOCLONAL ANTIBODIES Ustekinumab Inj: 45mg/0.5mL, ✓ (Stelara) 90mg/mL MONOCLONAL ANTIBODIES/CD20-BLOCKERS Rituximab Inj: 100mg/10mL, ✓ (Rituxan) 500mg/50mL (Continued) ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA MONOCLONAL ANTIBODIES/TNF-BLOCKERS Adalimumab Inj: 20mg/0.4mL, ✓ ✓ ✓ ✓ (Humira) 40mg/0.8mL Golimumab Inj: 50mg/0.5mL, ✓ ✓ ✓ (Simponi) 100mg/mL Infliximab Inj: 100mg ✓ ✓ ✓ (Remicade) NON-STEROIDAL ANTI-INFLAMMATORY DRUGS -

List of a FEW of MANY Aspirin-Like Or Herbal Supplement Products To
1809 E 13th St. Suite 100 -300 Tulsa, OK 74104 (918)582-6800 MEDICATION AND PRODUCTS TO BE AVOIDED PRIOR TO SURGERY **Do not stop taking blood pressure, diabetic, or prescribed medications that are not blood thinners. You will be advised at your pre-op when to stop these medications prior to surgery. If you have any question as to whether it is safe to stop a medication, please check with the prescribing physician. Aspirin and other non-steroidal anti-inflammatory drugs (NSAID’s), such as Motrin are strong anti-coagulants which can cause bleeding problems in normal individuals. In addition to these Aspirin- like medications, Vitamins and many herbal supplements (such as Garlic, Ginkgo, Ginseng, Flaxseed, Ginger, Feverfew, Bilberry, Chamomile, Selenium) can cause bleeding or adverse physiologic effects during surgery. If you are on a blood thinner or antiplatelet medication such as Eliquis, Coumadin (warfarin), Plavix (clopidogrel), Pletal (cilostazol)Pradaxa or Xarelto, you must stop these medications prior to surgery. Please follow the prescribing physician’s recommendation for stopping the medications. Do not restart blood thinners until your physician advises. Patients preparing for surgery must stop all sources of Aspirin, Aspirin like products, Vitamins and all Herbal Supplements or Diet Pills for 7 days prior to surgery and 5 days after surgery. Below are a FEW OF MANY Aspirin-like or Herbal Supplement products to be avoided prior to surgery. Advil Congesprin Chewable Fish Oil Nabumetone Selenium Aggrenox Compounded Creams Flaxseed Nalfon Sine – Aid Aleve Contac Flurbiprofen Naprelan Sine – Off Sinus Alka – Seltzers Cope Four Way Cold Tabs Naprosyn Sinutab Anacin Coricidin Gaysal-S Naproxen SK – 65 Anaprox Cosprin Garlic (Allium Sativum) Neocylate Soma Anadynos Coumadin Gelprin Norgesic Stanback Ansaid Damason P Gemnisin Novnaproxen Stendin APC Darvon Ginger Novodipiradrol St. -

S Salsalate Tablets
SALSALATE TABLETS CARDIOVASCULAR EFFECTS renal disease. If SALSALATE TABLETS therapy must be initiated, Rx Only Cardiovascular Thrombotic Events close monitoring of the patient’s renal function is advisable. Cardiovascular Risk Clinical trials of several COX-2 selective and nonselective NSAIDs Anaphylactoid Reactions • NSAIDs may cause an increased risk of serious cardiovascular of up to three years duration have shown an increased risk of As with other NSAIDs, anaphylactoid reactions may occur in thrombotic events, myocardial infarction, and stroke, which can serious cardiovascular (CV) thrombotic events, myocardial patients without known prior exposure to SALSALATE TABLETS. be fatal. This risk may increase with duration of use. Patients infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 SALSALATE TABLETS should not be given to patients with the with cardiovascular disease or risk factors for cardiovascular selective and nonselective, may have a similar risk. Patients with aspirin triad. This symptom complex typically occurs in asthmatic disease may be at greater risk. (See WARNINGS and CLINICAL known CV disease or risk factors for CV disease may be at greater patients who experience rhinitis with or without nasal polyps, or TRIALS). risk. To minimize the potential risk for an adverse CV event in who exhibit severe, potentially fatal bronchospasm after taking • SALSALATE TABLETS is contraindicated for the treatment of patients treated with an NSAID, the lowest effective dose should be aspirin or other NSAIDs (see CONTRAINDICATIONS and perioperative pain in the setting of coronary artery bypass graft used for the shortest duration possible. Physicians and patients PRECAUTIONS - Preexisting Asthma). Emergency help should be (CABG) surgery (see WARNINGS Gastrointestinal Risk) should remain alert for the development of such events, even in sought in cases where an anaphylactoid reaction occurs. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM LIDADRONICUM 63132-38-7 ABAFUNGIN 129639-79-8 ACIDUM SALCAPROZICUM 183990-46-7 ABAMECTIN 65195-55-3 ACIDUM SALCLOBUZICUM 387825-03-8 ABANOQUIL 90402-40-7 ACIFRAN 72420-38-3 ABAPERIDONUM 183849-43-6 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABATACEPTUM 332348-12-6 ACITEMATE 101197-99-3 ABCIXIMAB 143653-53-6 ACITRETIN 55079-83-9 ABECARNIL 111841-85-1 ACIVICIN 42228-92-2 ABETIMUSUM 167362-48-3 ACLANTATE 39633-62-0 ABIRATERONE 154229-19-3 ACLARUBICIN 57576-44-0 ABITESARTAN 137882-98-5 ACLATONIUM NAPADISILATE 55077-30-0 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURINUM 178535-93-8 ACOLBIFENUM 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDUM 185106-16-5 ACAMPROSATE 77337-76-9 -

Effect of Targeting Inflammation with Salsalate
Supplementary Online Content Hauser TH, Salastekar N, Schaefer EJ, et al; Effect of targeting inflammation with salsalate: the TINSAL-CVD randomized clinical trial on progression of coronary plaque in overweight and obese patients using statins. JAMA Cardiol. Published online May 25, 2016. doi:10.1001/jamacardio.2016.0605. eAppendix 1. Supplemental Background eAppendix 2. Additional TINSAL-CVD Study Team in Alphabetical Order Providing Current Contact Information eFigure. Coronary Artery Segment Plaque Assessment Demonstrating [A] Progression and [B] Regression Over 30-Months eTable 1. Primary Endpoint Plaque Volume in Salsalate Versus Placebo Results for the Intention to Treat (ITT) Population (Per Plaque Analysis) eTable 2. Secondary Analysis Plaque Density in Salsalate Versus Placebo Results for the Intention to Treat (ITT) Population (Per Plaque Analysis) eTable 3. Plaque Volume and Plaque Density in Salsalate Versus Placebo Results for the Intention to Treat (ITT) Population (Per Subject Analysis) eTable 4. Plaque Volume and Plaque Density in Salsalate Versus Placebo Results for the Per Protocol Analyses eTable 5. Plaque Volume and Plaque Density in Salsalate Versus Placebo Results for the Participants With Type 2 Diabetes eTable 6. Sensitivity Analyses Using Markov Chain Monte Carlo Method eTable 7. Baseline and Change From Baseline of Clinical and Laboratory Parameters by Treatment Group (SI Units) eTable 8. Serious Adverse Events Occurring After Randomization by Treatment Assignment eTable 9. Cardiac Events by Treatment Assignment eTable 10. Adverse Events Reported by 5% of Total Cohort and Numerically More in Salsalate Than Placebo Treated Group This supplementary material has been provided by the authors to give readers additional information about their work. -

Multiple Targets of Salicylic Acid and Its Derivatives in Plants and Animals
REVIEW published: 26 May 2016 doi: 10.3389/fimmu.2016.00206 Multiple Targets of Salicylic Acid and Its Derivatives in Plants and Animals Daniel F. Klessig1*, Miaoying Tian2 and Hyong Woo Choi1 1 Boyce Thompson Institute, Cornell University, Ithaca, NY, USA, 2 Department of Plant and Environmental Protection Sciences, University of Hawaii at Manoa, Honolulu, HI, USA Salicylic acid (SA) is a critical plant hormone that is involved in many processes, includ- ing seed germination, root initiation, stomatal closure, floral induction, thermogenesis, and response to abiotic and biotic stresses. Its central role in plant immunity, although extensively studied, is still only partially understood. Classical biochemical approaches and, more recently, genome-wide high-throughput screens have identified more than two dozen plant SA-binding proteins (SABPs), as well as multiple candidates that have yet to be characterized. Some of these proteins bind SA with high affinity, while the affinity of others exhibit is low. Given that SA levels vary greatly even within a particular plant species depending on subcellular location, tissue type, developmental stage, and with respect to both time and location after an environmental stimulus such as infection, the presence of SABPs exhibiting a wide range of affinities for SA may provide great Edited by: flexibility and multiple mechanisms through which SA can act. SA and its derivatives, Brigitte Mauch-Mani, Université de Neuchâtel, Switzerland both natural and synthetic, also have multiple targets in animals/humans. Interestingly, Reviewed by: many of these proteins, like their plant counterparts, are associated with immunity or Robin Katrina Cameron, disease development. Two recently identified SABPs, high mobility group box protein McMaster University, Canada and glyceraldehyde 3-phosphate dehydrogenase, are critical proteins that not only serve Taras P. -

Nsaids: Friend Or Foe in the Battle Against Pain?
NSAIDs: Friend or Foe in the Battle against Pain? Presented by June E. Oliver, MSN, CCNS, AP-PMN, APRN/CNS NO Conflicts of Interest to Declare Old & Natural! 1763 fever Rx- bark/leaves of willow/myrtle (salicylic acid) 1859-chemical structure discovered & synthesized in Germany 1914- Bayer Co. started manufacturing ASA Current sales 11 billion ( 2014) Early 20 th Century- NSAIDs discovered 1971- discovered mechanism of action of NSAIDs by John R. Vane 1990s-COX-2 isoenzyme successfully identified & cloned Current- script & OTC use = > 30 billion doses/yr of NSAIDs In US Numbers increase every year Prostaglandin (PG) Mechanism of Action Prostaglandins( PG) - lipids derived from acids: i.e. arachidonic (AA), lineolic, others PGs have Variety of functions Constitutive GI mucosal protection Kidney function Trauma response Cell membrane trauma- releases AA & COX enzyme converts to PGs inflammation Peripheral & central sensitization of nociceptors to mechanical & chemical stimuli Pyretic response PGs rise in CSF w/ pyrogen introduction Although not an NSAID, acetaminophen blocks brain PG synthetase (COX3 inhibition ) Cyclo-oxygenase (COX): “The Convertors” Cyclo-oxygenase 1&2 = isoenzymes that convert AA to PGs (i.e. prostacyclin, & thromboxanes) COX-1 Expressed regularly- provides gastric & duodenal mucosal protection Stimulates production mucin/bicarbonate/phospholipid that covers surface of stomach Enhances GI mucosal blood flow w/ local vasodilation Enhanced epithelial cell reproduction & migration towards lumen Can be induced -

Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act
Updated June 07, 2021 Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act Three categories of bulk drug substances: • Category 1: Bulk Drug Substances Under Evaluation • Category 2: Bulk Drug Substances that Raise Significant Safety Risks • Category 3: Bulk Drug Substances Nominated Without Adequate Support Updates to Categories of Substances Nominated for the 503B Bulk Drug Substances List1 • Add the following entry to category 2 due to serious safety concerns of mutagenicity, cytotoxicity, and possible carcinogenicity when quinacrine hydrochloride is used for intrauterine administration for non- surgical female sterilization: 2,3 o Quinacrine Hydrochloride for intrauterine administration • Revision to category 1 for clarity: o Modify the entry for “Quinacrine Hydrochloride” to “Quinacrine Hydrochloride (except for intrauterine administration).” • Revision to category 1 to correct a substance name error: o Correct the error in the substance name “DHEA (dehydroepiandosterone)” to “DHEA (dehydroepiandrosterone).” 1 For the purposes of the substance names in the categories, hydrated forms of the substance are included in the scope of the substance name. 2 Quinacrine HCl was previously reviewed in 2016 as part of FDA’s consideration of this bulk drug substance for inclusion on the 503A Bulks List. As part of this review, the Division of Bone, Reproductive and Urologic Products (DBRUP), now the Division of Urology, Obstetrics and Gynecology (DUOG), evaluated the nomination of quinacrine for intrauterine administration for non-surgical female sterilization and recommended that quinacrine should not be included on the 503A Bulks List for this use. This recommendation was based on the lack of information on efficacy comparable to other available methods of female sterilization and serious safety concerns of mutagenicity, cytotoxicity and possible carcinogenicity in use of quinacrine for this indication and route of administration.