Gastroduodenal Mucosal Damage with Salsalate Versus Aspirin: Results of Experimental Models and Endoscopic Studies in Humans
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep
animals Article Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep Shashwati Mathurkar 1,*, Preet Singh 2 ID , Kavitha Kongara 2 and Paul Chambers 2 1 1B, He Awa Crescent, Waikanae 5036, New Zealand 2 School of Veterinary Sciences, College of Sciences, Massey University, Palmerston North 4474, New Zealand; [email protected] (P.S.); [email protected] (K.K.); [email protected] (P.C.) * Correspondence: [email protected]; Tel.: +64-221-678-035 Received: 13 June 2018; Accepted: 16 July 2018; Published: 18 July 2018 Simple Summary: Scarcity of non-steroidal anti-inflammatory drugs (NSAID) to minimise the pain in sheep instigated the current study. The aim of this study was to know the pharmacokinetic parameters of salicylic acid in New Zealand sheep after administration of multiple intravenous and oral doses of sodium salicylate (sodium salt of salicylic acid). Results of the study suggest that the half-life of the drug was shorter and clearance was faster after intravenous administration as compared to that of the oral administration. The minimum effective concentration required to produce analgesia in humans (16.8 µL) was achieved in sheep for about 0.17 h in the current study after intravenous administration of 100 and 200 mg/kg body weight of sodium salicylate. However, oral administration of these doses failed to achieve the minimum effective concentration as mentioned above. This study is of significance as it adds valuable information on pharmacokinetics and its variation due to breed, species, age, gender and environmental conditions. -

Salsalate Tablets, USP 500 Mg and 750 Mg Rx Only
SALSALATE RX- salsalate tablet, film coated ANDAPharm LLC Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here. ---------- Salsalate Tablets, USP 500 mg and 750 mg Rx Only Cardiovascular Risk NSAIDs may cause an increase risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (See WARNINGS and CLINICAL TRIALS). Salsalate tablets, USP is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery (See WARNINGS). Gastrointestinal Risk NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS). DESCRIPTION Salsalate, is a nonsteroidal anti-inflammatory agent for oral administration. Chemically, salsalate (salicylsalicylic acid or 2-hydroxybenzoic acid, 2-carboxyphenyl ester) is a dimer of salicylic acid; its structural formula is shown below. Chemical Structure: Inactive Ingredients: Colloidal Silicon Dioxide, D&C Yellow #10 Aluminum Lake, Hypromellose, Microcrystalline Cellulose, Sodium Starch Glycolate, Stearic Acid, Talc, Titanium Dioxide, Triacetin. CLINICAL PHARMACOLOGY Salsalate is insoluble in acid gastric fluids (<0.1 mg/mL at pH 1.0), but readily soluble in the small intestine where it is partially hydrolyzed to two molecules of salicylic acid. -
Download Product Insert (PDF)
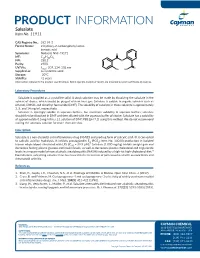
PRODUCT INFORMATION Salsalate Item No. 11911 CAS Registry No.: 552-94-3 Formal Name: 2-hydroxy-2-carboxyphenyl ester- benzoic acid Synonyms: Nobacid, NSC 49171 O MF: C14H10O5 FW: 258.2 O Purity: ≥98% UV/Vis.: λ: 207, 234, 308 nm O max OH HO Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Salsalate is supplied as a crystalline solid. A stock solution may be made by dissolving the salsalate in the solvent of choice, which should be purged with an inert gas. Salsalate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of salsalate in these solvents is approximately 3, 5, and 14 mg/ml, respectively. Salsalate is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, salsalate should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Salsalate has a solubility of approximately 0.5 mg/ml in a 1:1 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description Salsalate is a non-steroidal anti-inflammatory drug (NSAID) and prodrug form of salicylic acid.1 It is converted to salicylic acid by hydrolysis. It inhibits prostaglandin E2 (PGE2; Item No. 14010) production in isolated 2 human whole blood stimulated with LPS (IC50 = 39.9 µM). Salsalate (1,000 mg/kg) inhibits weight gain and decreases fasting plasma glucose and insulin levels, as well as decreases plasma cholesterol and triglyceride levels in a mouse model of non-alcoholic steatohepatitis (NASH) induced by a high-fat high-cholesterol diet.3 Formulations containing salsalate have been used in the treatment of pain associated with osteoarthritis and rheumatoid arthritis. -

Sodium-Salicylate-European-Public-Mrl-Assessment-Report-Epmar-Committee-Veterinary
27 October 2010 EMA/CVMP/562066/2007 Veterinary Medicines and Product Data Management Committee for Medicinal Products for Veterinary Use European public MRL assessment report (EPMAR) Sodium salicylate (turkeys) On 12 October 2010 the European Commission adopted a Regulation1 establishing provisional maximum residue limits for sodium salicylate in turkeys, valid throughout the European Union. These provisional maximum residue limits were based on the favourable opinion and the assessment report adopted by the Committee for Medicinal Products for Veterinary Use. In turkeys, sodium salicylate is intended for use orally as an antipyretic in the treatment of acute respiratory diseases. Sodium salicylate was previously assessed for the purpose of establishing maximum residue limits and was entered in Annex II of Regulation (EEC) No 2377/902 (no MRL required) for topical use in all food producing species except fish and for oral use in bovine and porcine species. Chevita Tierarzneimittel GmbH submitted to the European Medicines Agency on 4 January 2007 an application for the extension of existing entry in Annex II of Regulation (EEC) No 2377/90 for sodium salicylates to turkeys. On 12 December 2007 the Committee for Medicinal Products for Veterinary Use adopted an opinion recommending the amendment of the entry in Annex II of Regulation (EEC) No 2377/90 to include sodium salicylate for oral use in turkeys. The European Commission subsequently returned the opinion to the Committee to consider whether its opinion should be reviewed to take into account issues raised during the Commission’s inter service consultation and in particular to consider whether establishment of maximum residue limits for sodium salicylate in turkeys should be established. -

Nsaids: Dare to Compare 1997
NSAIDs TheRxFiles DARE TO COMPARE Produced by the Community Drug Utilization Program, a Saskatoon District Health/St. Paul's Hospital program July 1997 funded by Saskatchewan Health. For more information check v our website www.sdh.sk.ca/RxFiles or, contact Loren Regier C/O Pharmacy Department, Saskatoon City Hospital, 701 Queen St. Saskatoon, SK S7K 0M7, Ph (306)655-8506, Fax (306)655-8804; Email [email protected] We have come a long way from the days of willow Highlights bark. Today salicylates and non-steroidal anti- • All NSAIDs have similar efficacy and side inflammatory drugs (NSAIDs) comprise one of the effect profiles largest and most commonly prescribed groups of • In low risk patients, Ibuprofen and naproxen drugs worldwide.1 In Saskatchewan, over 20 may be first choice agents because they are different agents are available, accounting for more effective, well tolerated and inexpensive than 300,000 prescriptions and over $7 million in • Acetaminophen is the recommended first line sales each year (Saskatchewan Health-Drug Plan agent for osteoarthritis data 1996). Despite the wide selection, NSAIDs • are more alike than different. Although they do Misoprostol is the only approved agent for differ in chemical structure, pharmacokinetics, and prophylaxis of NSAID-induced ulcers and is to some degree pharmacodynamics, they share recommended in high risk patients if NSAIDS similar mechanisms of action, efficacy, and adverse cannot be avoided. effects. week or more to become established. For this EFFICACY reason, an adequate trial of 1-2 weeks should be NSAIDs work by inhibiting cyclooxygenase (COX) allowed before increasing the dose or changing to and subsequent prostaglandin synthesis as well as another NSAID. -

Food and Drug Administration, HHS § 201.323
Food and Drug Administration, HHS § 201.323 liver damage or gastrointestinal bleed- calcium, choline salicylate, magnesium ing). OTC drug products containing in- salicylate, or sodium salicylate] or ternal analgesic/antipyretic active in- other pain relievers/fever reducers. [Ac- gredients may cause similar adverse ef- etaminophen and (insert one nonste- fects. FDA concludes that the labeling roidal anti-inflammatory analgesic/ of OTC drug products containing inter- antipyretic ingredient—including, but nal analgesic/antipyretic active ingre- not limited to aspirin, carbaspirin cal- dients should advise consumers with a cium, choline salicylate, magnesium history of heavy alcohol use to consult salicylate, or sodium salicylate] may a physician. Accordingly, any OTC cause liver damage and stomach bleed- drug product, labeled for adult use, ing.’’ containing any internal analgesic/anti- (b) Requirements to supplement ap- pyretic active ingredients (including, proved application. Holders of approved but not limited to, acetaminophen, as- applications for OTC drug products pirin, carbaspirin calcium, choline sa- that contain internal analgesic/anti- licylate, ibuprofen, ketoprofen, magne- pyretic active ingredients that are sub- sium salicylate, naproxen sodium, and ject to the requirements of paragraph sodium salicylate) alone or in combina- (a) of this section must submit supple- tion shall bear an alcohol warning ments under § 314.70(c) of this chapter statement in its labeling as follows: to include the required warning in the (1) Acetaminophen. ‘‘Alcohol Warn- product’s labeling. Such labeling may ing’’ [heading in boldface type]: ‘‘If you be put into use without advance ap- consume 3 or more alcoholic drinks proval of FDA provided it includes the every day, ask your doctor whether exact information included in para- you should take acetaminophen or graph (a) of this section. -

New Zealand Data Sheet 1
New Zealand Data Sheet 1. PRODUCT NAME NAXEN® 250 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each NAXEN 250 mg tablet contains 250 mg of Naproxen For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM NAXEN 250 mg tablets are yellow, biconvex, round tablet of 11 mm diameter with one face engraved NX250 and having a bisecting score. The score line is only to facilitate breaking for ease of swallowing and not to divide into equal doses. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications NAXEN is indicated in adults for the relief of symptoms associated with rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, tendonitis and bursitis, acute gout and primary dysmenorrhoea. NAXEN is indicated in children for juvenile arthritis. 4.2. Dose and method of administration After assessing the risk/benefit ratio in each individual patient, the lowest effective dose for the shortest possible duration should be used (see Section 4.4). During long-term administration the dose of naproxen may be adjusted up or down depending on the clinical response of the patient. A lower daily dose may suffice for long-term administration. In patients who tolerate lower doses well, the dose may be increased to 1000 mg per day when a higher level of anti-inflammatory/analgesic 1 | P a g e activity is required. When treating patients with naproxen 1000 mg/day, the physician should observe sufficient increased clinical benefit to offset the potential increased risk. Dose Adults For rheumatoid arthritis, osteoarthritis and ankylosing spondylitis Initial therapy: The usual dose is 500-1000 mg per day taken in two doses at 12 hour intervals. -

Colonoscopy Instructions
Colonoscopy Checklist Five days before your colonoscopy: Stop any medications that thin the blood (see list below) Discuss the discontinuation of these medications with your primary care physician to ensure that it is safe to stop them Three days before your colonoscopy: Stop eating high fiber foods including nuts, corn, popcorn, raw fruits, vegetables, and bran Stop fiber supplements The day before your colonoscopy: Have a normal breakfast If your colonoscopy is scheduled before noon the following day, do not have any lunch If your colonoscopy is scheduled after noon, have a light lunch Have clear liquids for the rest of the day (see below) Start prep as instructed by your physician Do not have anything to eat or drink after midnight The day of your colonoscopy: Take your blood pressure medications with a sip of water Make sure you bring your driver’s license or photo ID and leave valuables and jewelry at home Clear Liquid Diet Water Any kind of soft drink (ginger ale, cola, tonic, etc) Gatorade Apple Juice Orange Juice without pulp Lemonade Tea/Coffee (without milk) Dietary supplements (Ensure, Boost, Enlive, etc) Clear broth (vegetable, chicken, or beef) Jell‐O (stay away from red, blue, or purple colors) Ice pops without milk or fruit bits Honey or sugar NO DAIRY PRODUCTS Medications to stop prior to colonoscopy Below is a list of many medications (but not all) that fall into these categories. It is important to remember that there are hundreds of over‐the‐counter medications that contain NSAIDs or aspirin, so it is important to carefully read the label of any medication that you are taking (prescription or over‐the‐counter). -

Salicylate, Diflunisal and Their Metabolites Inhibit CBP/P300 and Exhibit Anticancer Activity
RESEARCH ARTICLE Salicylate, diflunisal and their metabolites inhibit CBP/p300 and exhibit anticancer activity Kotaro Shirakawa1,2,3,4, Lan Wang5,6, Na Man5,6, Jasna Maksimoska7,8, Alexander W Sorum9, Hyung W Lim1,2, Intelly S Lee1,2, Tadahiro Shimazu1,2, John C Newman1,2, Sebastian Schro¨ der1,2, Melanie Ott1,2, Ronen Marmorstein7,8, Jordan Meier9, Stephen Nimer5,6, Eric Verdin1,2* 1Gladstone Institutes, University of California, San Francisco, United States; 2Department of Medicine, University of California, San Francisco, United States; 3Department of Hematology and Oncology, Kyoto University, Kyoto, Japan; 4Graduate School of Medicine, Kyoto University, Kyoto, Japan; 5University of Miami, Gables, United States; 6Sylvester Comprehensive Cancer Center, Miami, United States; 7Perelman School of Medicine, University of Pennsylvania, Philadelphia, United States; 8Department of Biochemistry and Biophysics, Abramson Family Cancer Research Institute, Philadelphia, United States; 9Chemical Biology Laboratory, National Cancer Institute, Frederick, United States Abstract Salicylate and acetylsalicylic acid are potent and widely used anti-inflammatory drugs. They are thought to exert their therapeutic effects through multiple mechanisms, including the inhibition of cyclo-oxygenases, modulation of NF-kB activity, and direct activation of AMPK. However, the full spectrum of their activities is incompletely understood. Here we show that salicylate specifically inhibits CBP and p300 lysine acetyltransferase activity in vitro by direct *For correspondence: everdin@ competition with acetyl-Coenzyme A at the catalytic site. We used a chemical structure-similarity gladstone.ucsf.edu search to identify another anti-inflammatory drug, diflunisal, that inhibits p300 more potently than salicylate. At concentrations attainable in human plasma after oral administration, both salicylate Competing interests: The and diflunisal blocked the acetylation of lysine residues on histone and non-histone proteins in cells. -

(Ketorolac Tromethamine Tablets) Rx Only WARNING TORADOL
TORADOL ORAL (ketorolac tromethamine tablets) Rx only WARNING TORADOLORAL (ketorolac tromethamine), a nonsteroidal anti-inflammatory drug (NSAID), is indicated for the short-term (up to 5 days in adults), management of moderately severe acute pain that requires analgesia at the opioid level and only as continuation treatment following IV or IM dosing of ketorolac tromethamine, if necessary. The total combined duration of use of TORADOLORAL and ketorolac tromethamine should not exceed 5 days. TORADOLORAL is not indicated for use in pediatric patients and it is NOT indicated for minor or chronic painful conditions. Increasing the dose of TORADOLORAL beyond a daily maximum of 40 mg in adults will not provide better efficacy but will increase the risk of developing serious adverse events. GASTROINTESTINAL RISK Ketorolac tromethamine, including TORADOL can cause peptic ulcers, gastrointestinal bleeding and/or perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Therefore, TORADOL is CONTRAINDICATED in patients with active peptic ulcer disease, in patients with recent gastrointestinal bleeding or perforation, and in patients with a history of peptic ulcer disease or gastrointestinal bleeding. Elderly patients are at greater risk for serious gastrointestinal events (see WARNINGS). CARDIOVASCULAR RISK NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk (see WARNINGS and CLINICAL STUDIES). TORADOL is CONTRAINDICATED for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS). -

Medications & Supplements to Avoid Before Procedures
Medications & Supplements to Avoid Before Procedures Do not ingest any brand of aspirin, or any aspirin-containing medication, any MAO inhibiting, or any serotonin medications, for 14 prior to and 14 days after surgery. Disclose every medication, supplement, etc. With Dr. Rau and your anesthesiologist. Aspirin and aspirin-containing products, as well as some supplements and herbals, may inhibit blood clotting and cause difficulties during and after surgery. If you need an aspirin-free fever reducer and pain reliever, take Tylenol. Also, if you smoke, you must refrain for at least a month prior to a month after your surgery date. Smoking significantly reduces your body’s circulation and vascularity, meaning that your tissues won’t receive all the oxygen needed for proper healing. DIET PILLS, FAT LOSS SUPPLEMENTS AND STACKERS: Please stop taking these pills at least 2 weeks before surgery. Many of these pills contain anticoagulants and can seriously impede your body's ability to clot sufficiently, resulting in hemorrhaging. Many of them also contain ephedra and caffeine, which can affect your anesthetic medications. Remember: if you take antibiotics or if you stop oral contraceptive pills for surgery, use an alternative method of birth control. A Aspirin, Advil, Actifed, Acuprin, Addaprin, Alka Seltzer, Alpha Omega (fish oil), Aluprin, Amitriptyline, Anacin, Ansaid, Anodynos, Analval, Anodynos, Ansaid, Argesic, Arthra-G, Arthralgen, Arthropan, Ascodeen, Ascriptin, Aspir-lox, Asperi-mox, Aspirbuf, Aspercin, Aspergum, Axotal, Azdone, -

Arthritis Treatment Comparison Arthritis Treatment Comparison
ARTHRITIS TREATMENT COMPARISON ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA CHELATING AGENTS Penicillamine Cap: 250mg ✓ (Cuprimine) Penicillamine Tab: 250mg ✓ (Depen) CYCLIC POLYPEPTIDE IMMUNOSUPPRESSANTS Cyclosporine Cap: 25mg, 100mg; ✓ (Gengraf, Neoral) Sol: 100mg/mL CYCLOOXYGENASE-2 INHIBITORS Celecoxib Cap: 50mg, 100mg, ✓ ✓ ✓ ✓ (Celebrex) 200mg, 400mg DIHYDROFOLIC ACID REDUCTASE INHIBITORS Methotrexate Inj: 25mg/mL; ✓ ✓ Tab: 2.5mg Methotrexate Tab: 5mg, 7.5mg, ✓ ✓ (Trexall) 10mg, 15mg INTERLEUKIN RECEPTOR ANTAGONISTS Anakinra Inj: 100mg/0.67mL ✓ (Kineret) Tocilizumab Inj: 20mg/mL, ✓ ✓ (Actemra) 162mg/0.9mL GOLD COMPOUNDS Auranofin Cap: 3mg ✓ (Ridaura) Gold sodium thiomalate Inj: 50mg/mL ✓ ✓ (Myochrysine) HYALURONAN AND DERIVATIVES Hyaluronan Inj: 30mg/2mL ✓ (Orthovisc) Sodium hyaluronate Inj: 1% ✓ (Euflexxa) Sodium hyaluronate Inj: 10mg/mL ✓ (Hyalgan) Sodium hyaluronate Inj: 2.5mL ✓ (Supartz) HYLAN POLYMERS Hylan G-F 20 Inj: 8mg/mL ✓ (Synvisc, Synvisc One) KINASE INHIBITORS Tofacitinib Tab: 5mg ✓ (Xeljanz) MONOCLONAL ANTIBODIES Ustekinumab Inj: 45mg/0.5mL, ✓ (Stelara) 90mg/mL MONOCLONAL ANTIBODIES/CD20-BLOCKERS Rituximab Inj: 100mg/10mL, ✓ (Rituxan) 500mg/50mL (Continued) ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA MONOCLONAL ANTIBODIES/TNF-BLOCKERS Adalimumab Inj: 20mg/0.4mL, ✓ ✓ ✓ ✓ (Humira) 40mg/0.8mL Golimumab Inj: 50mg/0.5mL, ✓ ✓ ✓ (Simponi) 100mg/mL Infliximab Inj: 100mg ✓ ✓ ✓ (Remicade) NON-STEROIDAL ANTI-INFLAMMATORY DRUGS