Natural Salicylates and Their Roles in Human Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Methyl Salicylate and Menthol | Memorial Sloan Kettering Cancer Center
PATIENT & CAREGIVER EDUCATION Methyl Salicylate and Menthol This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US AMPlify Relief MM [OTC]; BenGay [OTC]; Calypxo HP [OTC]; Capasil [OTC]; Icy Hot [OTC]; Kwan Loong Pain Relieving [OTC]; Precise [OTC]; Salonpas Arthritis Pain [OTC]; Salonpas Jet Spray [OTC]; Salonpas Massage Foam [OTC]; Salonpas Pain Relief Patch [OTC]; Thera-Gesic Plus [OTC]; Thera-Gesic [OTC] What is this drug used for? It is used to ease muscle and joint aches and pain. What do I need to tell my doctor BEFORE I take this drug? If you have an allergy to aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen. If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If your skin is damaged or has open wounds. Do not put on damaged skin or open wounds. If you are taking any other NSAID. If you are taking a salicylate drug like aspirin. If you are pregnant, plan to become pregnant, or get pregnant while taking this drug. This drug may cause harm to an unborn baby if taken at 20 weeks or later Methyl Salicylate and Menthol 1/7 in pregnancy. If you are between 20 to 30 weeks of pregnancy, only take this drug if your doctor has told you to. Do not take this drug if you are more than 30 weeks pregnant. -

Synthesis of Aspirin
SYNTHESIS OF ASPIRIN I. OBJECTIVES AND BACKGROUND You will: synthesize acetylsalicylic acid (aspirin) by carrying out a simple organic reaction, separate your product from the reaction mixture by vacuum filtration, purify your product by recrystallization, perform a chemical test to identify the change in functional group from reactant to product, and determine the success of your synthesis by calculating the percentage yield of your product. INTRODUCTION Aspirin is one of the most widely used medications in the world. It is employed as an analgesic (pain relief), an anti-pyretic (fever control) and an anti-inflammatory. More recently, studies have indicated that daily intake of small doses of aspirin can lower the risk of heart attack and stroke in high-risk patients. The history of aspirin and its precursor dates back to ancient times. Documents attributed to Hippocrates, the father of modern medicine, from the 4th century B.C. refer to the alleviation of pain by chewing on the bark of a willow tree or ingesting a powder made from the bark and leaves of the willow. This remedy was passed on from generation to generation. Fast forward now to the 19th century, where the field of organic chemistry began to experience tremendous growth. By 1838, chemists had managed to isolate, purify and identify the component of willow bark that provided the analgesic benefit. The compound was named salicylic acid, which was based on the genus name of the willow. Efforts to market salicylic acid met with failure, due to an unfortunate side effect-- prolonged ingestion of salicylic acid led to stomach pain, and in some cases, ulcers. -

Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep
animals Article Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep Shashwati Mathurkar 1,*, Preet Singh 2 ID , Kavitha Kongara 2 and Paul Chambers 2 1 1B, He Awa Crescent, Waikanae 5036, New Zealand 2 School of Veterinary Sciences, College of Sciences, Massey University, Palmerston North 4474, New Zealand; [email protected] (P.S.); [email protected] (K.K.); [email protected] (P.C.) * Correspondence: [email protected]; Tel.: +64-221-678-035 Received: 13 June 2018; Accepted: 16 July 2018; Published: 18 July 2018 Simple Summary: Scarcity of non-steroidal anti-inflammatory drugs (NSAID) to minimise the pain in sheep instigated the current study. The aim of this study was to know the pharmacokinetic parameters of salicylic acid in New Zealand sheep after administration of multiple intravenous and oral doses of sodium salicylate (sodium salt of salicylic acid). Results of the study suggest that the half-life of the drug was shorter and clearance was faster after intravenous administration as compared to that of the oral administration. The minimum effective concentration required to produce analgesia in humans (16.8 µL) was achieved in sheep for about 0.17 h in the current study after intravenous administration of 100 and 200 mg/kg body weight of sodium salicylate. However, oral administration of these doses failed to achieve the minimum effective concentration as mentioned above. This study is of significance as it adds valuable information on pharmacokinetics and its variation due to breed, species, age, gender and environmental conditions. -

Table S1: Sensitivity, Specificity, PPV, NPV, and F1 Score of NLP Vs. ICD for Identification of Symptoms for (A) Biome Developm
Table S1: Sensitivity, specificity, PPV, NPV, and F1 score of NLP vs. ICD for identification of symptoms for (A) BioMe development cohort; (B) BioMe validation cohort; (C) MIMIC-III; (D) 1 year of notes from patients in BioMe calculated using manual chart review. A) Fatigue Nausea and/or vomiting Anxiety Depression NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.99 (0.93- 0.59 (0.43- <0.00 0.25 (0.12- <0.00 <0.00 0.54 (0.33- Sensitivity 0.99 (0.9 – 1) 0.98 (0.88 -1) 0.3 (0.15-0.5) 0.85 (0.65-96) 0.02 1) 0.73) 1 0.42) 1 1 0.73) 0.57 (0.29- 0.9 (0.68- Specificity 0.89 (0.4-1) 0.75 (0.19-1) 0.68 0.97 (0.77-1) 0.03 0.98 (0.83-1) 0.22 0.81 (0.53-0.9) 0.96 (0.79-1) 0.06 0.82) 0.99) 0.99 (0.92- 0.86 (0.71- 0.94 (0.79- 0.79 (0.59- PPV 0.96 (0.82-1) 0.3 0.95 (0.66-1) 0.02 0.95 (0.66-1) 0.16 0.93 (0.68-1) 0.12 1) 0.95) 0.99) 0.92) 0.13 (0.03- <0.00 0.49 (0.33- <0.00 0.66 (0.48- NPV 0.89 (0.4-1) 0.007 0.94 (0.63-1) 0.34 (0.2-0.51) 0.97 (0.81-1) 0.86 (0.6-0.95) 0.04 0.35) 1 0.65) 1 0.81) <0.00 <0.00 <0.00 F1 Score 0.99 0.83 0.88 0.57 0.95 0.63 0.82 0.79 0.002 1 1 1 Itching Cramp Pain NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.98 (0.86- 0.24 (0.09- <0.00 0.09 (0.01- <0.00 0.52 (0.37- <0.00 Sensitivity 0.98 (0.85-1) 0.99 (0.93-1) 1) 0.45) 1 0.29) 1 0.66) 1 0.89 (0.72- 0.5 (0.37- Specificity 0.96 (0.8-1) 0.98 (0.86-1) 0.68 0.98 (0.88-1) 0.18 0.5 (0-1) 1 0.98) 0.66) 0.88 (0.69- PPV 0.96 (0.8-1) 0.8 (0.54-1) 0.32 0.8 (0.16-1) 0.22 0.99 (0.93-1) 0.98 (0.87-1) NA* 0.97) 0.98 (0.85- 0.57 (0.41- <0.00 0.58 (0.43- <0.00 NPV 0.98 (0.86-1) 0.5 (0-1) 0.02 (0-0.08) NA* 1) 0.72) 1 0.72) 1 <0.00 <0.00 <0.00 F1 Score 0.97 0.56 0.91 0.28 0.99 0.68 1 1 1 *Denotes 95% confidence intervals and P values that could not be calculated due to insufficient cells in 2x2 tables. -

The Role of Organic Small Molecules in Pain Management
molecules Review The Role of Organic Small Molecules in Pain Management Sebastián A. Cuesta and Lorena Meneses * Laboratorio de Química Computacional, Facultad de Ciencias Exactas y Naturales, Escuela de Ciencias Químicas, Pontificia Universidad Católica del Ecuador, Av. 12 de Octubre 1076 Apartado, Quito 17-01-2184, Ecuador; [email protected] * Correspondence: [email protected]; Tel.: +593-2-2991700 (ext. 1854) Abstract: In this review, a timeline starting at the willow bark and ending in the latest discoveries of analgesic and anti-inflammatory drugs will be discussed. Furthermore, the chemical features of the different small organic molecules that have been used in pain management will be studied. Then, the mechanism of different types of pain will be assessed, including neuropathic pain, inflammatory pain, and the relationship found between oxidative stress and pain. This will include obtaining insights into the cyclooxygenase action mechanism of nonsteroidal anti-inflammatory drugs (NSAID) such as ibuprofen and etoricoxib and the structural difference between the two cyclooxygenase isoforms leading to a selective inhibition, the action mechanism of pregabalin and its use in chronic neuropathic pain, new theories and studies on the analgesic action mechanism of paracetamol and how changes in its structure can lead to better characteristics of this drug, and cannabinoid action mechanism in managing pain through a cannabinoid receptor mechanism. Finally, an overview of the different approaches science is taking to develop more efficient molecules for pain treatment will be presented. Keywords: anti-inflammatory drugs; QSAR; pain management; cyclooxygenase; multitarget drug; Citation: Cuesta, S.A.; Meneses, L. cannabinoid; neuropathic pain The Role of Organic Small Molecules in Pain Management. -

Chemical Composition and Product Quality Control of Turmeric
Stephen F. Austin State University SFA ScholarWorks Faculty Publications Agriculture 2011 Chemical composition and product quality control of turmeric (Curcuma longa L.) Shiyou Li Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Wei Yuan Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Guangrui Deng Ping Wang Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Peiying Yang See next page for additional authors Follow this and additional works at: http://scholarworks.sfasu.edu/agriculture_facultypubs Part of the Natural Products Chemistry and Pharmacognosy Commons, and the Pharmaceutical Preparations Commons Tell us how this article helped you. Recommended Citation Li, Shiyou; Yuan, Wei; Deng, Guangrui; Wang, Ping; Yang, Peiying; and Aggarwal, Bharat, "Chemical composition and product quality control of turmeric (Curcuma longa L.)" (2011). Faculty Publications. Paper 1. http://scholarworks.sfasu.edu/agriculture_facultypubs/1 This Article is brought to you for free and open access by the Agriculture at SFA ScholarWorks. It has been accepted for inclusion in Faculty Publications by an authorized administrator of SFA ScholarWorks. For more information, please contact [email protected]. Authors Shiyou Li, Wei Yuan, Guangrui Deng, Ping Wang, Peiying Yang, and Bharat Aggarwal This article is available at SFA ScholarWorks: http://scholarworks.sfasu.edu/agriculture_facultypubs/1 28 Pharmaceutical Crops, 2011, 2, 28-54 Open Access Chemical Composition and Product Quality Control of Turmeric (Curcuma longa L.) ,1 1 1 1 2 3 Shiyou Li* , Wei Yuan , Guangrui Deng , Ping Wang , Peiying Yang and Bharat B. Aggarwal 1National Center for Pharmaceutical Crops, Arthur Temple College of Forestry and Agriculture, Stephen F. -

Poison Prevention Packaging: a Guide for Healthcare Professionals
PPooiissoonn PPrreevveennttiioonn PPaacckkaaggiinngg:: AA GGuuiiddee FFoorr HHeeaalltthhccaarree PPrrooffeessssiioonnaallss REVISED 2005 CPSC 384 US. CONSUMER PRODUCT SAFETY COMMISSION, WASHINGTON, D.C. 20207 THIS BROCHURE BROUGHT TO YOU BY: U.S. CONSUMER PRODUCT SAFETY COMMISSION Washington, DC 20207 Web site: www.cpsc.gov Toll-free hotline: 1-800-638-2772 The U.S. Consumer Product Safety Commission (CPSC) is a federal agency that helps keep families and children safe in and around their homes. For more information, call the CPSC’s toll-free hotline at 1-800-638-2772 or visit its website at http://www.cpsc.gov. Poison Prevention Packaging: A Guide For Healthcare Professionals (revised 2005) Preface The U.S. Consumer Product Safety Commission (CPSC) administers the Poison Prevention Packaging Act of 1970 (PPPA), 15 U.S.C. §§ 1471-1476. The PPPA requires special (child-resistant and adult-friendly) packaging of a wide range of hazardous household products including most oral prescription drugs. Healthcare professionals are more directly involved with the regulations dealing with drug products than household chemical products. Over the years that the regulations have been in effect, there have been remarkable declines in reported deaths from ingestions by children of toxic household substances including medications. Despite this reduction in deaths, many children are poisoned or have "near-misses" with medicines and household chemicals each year. Annually, there are about 30 deaths of children under 5 years of age who are unintentionally poisoned. Data from the National Electronic Injury Surveillance System (a CPSC database of emergency room visits) indicate that in 2003, an estimated 78,000 children under 5 years of age were treated for poisonings in hospital emergency rooms in the United States. -

PRODUCT INFORMATION Mefenamic Acid Item No
PRODUCT INFORMATION Mefenamic Acid Item No. 23650 CAS Registry No.: 61-68-7 OH Formal Name: 2-[(2,3-dimethylphenyl)amino]-benzoic acid O Synonyms: C.I. 473, CN 35355, NSC 94437 H C H NO MF: 15 15 2 N FW: 241.3 Purity: ≥98% Supplied as: A solid Storage: 4°C Stability: ≥1 year Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Mefenamic acid is supplied as a solid. A stock solution may be made by dissolving the mefenamic acid in the solvent of choice, which should be purged with an inert gas. Mefenamic acid is slightly soluble in DMSO and methanol. Description Mefenamic acid is a non-steroidal anti-inflammatory drug (NSAID) and a COX-2 inhibitor.1 It binds to COX-2 (Kd = 4 nM) and inhibits COX-2-dependent oxygenation of arachidonic acid (Item Nos. 90010 | 90010.1 | 10006607) in vitro (Ki = 10 µM). Mefenamic acid (30 mg/kg) reduces acetic acid-induced writhing in rats.2 It inhibits increases in skin thickness in a mouse model of delayed-type hypersensitivity induced by dinitrochlorobenzene (DNBC).2 Mefenamic acid also reduces the antibody response to sheep red blood cells in mice. References 1. Prusakiewicz, J.J., Duggan, K.C., Rouzer, C.A., et al. Differential sensitivity and mechanism of inhibition of COX-2 oxygenation of arachidonic acid and 2-arachidonoylglycerol by ibuprofen and mefenamic acid. Biochemistry 48(31), 7353-7355 (2009). 2. Roszkowski, A.P., Rooks, W.H., Tomolonis, A.J., et al. Anti-inflammatory and analgetic properties of d-2-(6’-methoxy-2’-naphthyl)-propionic acid (naproxen). -

Salsalate Tablets, USP 500 Mg and 750 Mg Rx Only
SALSALATE RX- salsalate tablet, film coated ANDAPharm LLC Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here. ---------- Salsalate Tablets, USP 500 mg and 750 mg Rx Only Cardiovascular Risk NSAIDs may cause an increase risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (See WARNINGS and CLINICAL TRIALS). Salsalate tablets, USP is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery (See WARNINGS). Gastrointestinal Risk NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS). DESCRIPTION Salsalate, is a nonsteroidal anti-inflammatory agent for oral administration. Chemically, salsalate (salicylsalicylic acid or 2-hydroxybenzoic acid, 2-carboxyphenyl ester) is a dimer of salicylic acid; its structural formula is shown below. Chemical Structure: Inactive Ingredients: Colloidal Silicon Dioxide, D&C Yellow #10 Aluminum Lake, Hypromellose, Microcrystalline Cellulose, Sodium Starch Glycolate, Stearic Acid, Talc, Titanium Dioxide, Triacetin. CLINICAL PHARMACOLOGY Salsalate is insoluble in acid gastric fluids (<0.1 mg/mL at pH 1.0), but readily soluble in the small intestine where it is partially hydrolyzed to two molecules of salicylic acid. -

In Vitro Immunopharmacological Profiling of Ginger (Zingiber Officinale Roscoe)
Research Collection Doctoral Thesis In vitro immunopharmacological profiling of ginger (Zingiber officinale Roscoe) Author(s): Nievergelt, Andreas Publication Date: 2011 Permanent Link: https://doi.org/10.3929/ethz-a-006717482 Rights / License: In Copyright - Non-Commercial Use Permitted This page was generated automatically upon download from the ETH Zurich Research Collection. For more information please consult the Terms of use. ETH Library DISS. ETH Nr. 19591 In Vitro Immunopharmacological Profiling of Ginger (Zingiber officinale Roscoe) ABHANDLUNG zur Erlangung des Titels DOKTOR DER WISSENSCHAFTEN der ETH ZÜRICH vorgelegt von Andreas Nievergelt Eidg. Dipl. Apotheker, ETH Zürich geboren am 18.12.1978 von Schleitheim, SH Angenommen auf Antrag von Prof. Dr. Karl-Heinz Altmann, Referent Prof. Dr. Jürg Gertsch, Korreferent Prof. Dr. Michael Detmar, Korreferent 2011 Table of Contents Summary 6 Zusammenfassung 7 Acknowledgements 8 List of Abbreviations 9 1. Introduction 13 1.1 Ginger (Zingiber officinale) 13 1.1.1 Origin 14 1.1.2 Description 14 1.1.3 Chemical Constituents 15 1.1.4 Traditional and Modern Pharmaceutical Use of Ginger 17 1.1.5 Reported In Vitro Effects 20 1.2 Immune System and Inflammation 23 1.2.1 Innate and Adaptive Immunity 24 1.2.2 Cytokines in Inflammation 25 1.2.3 Pattern Recognition Receptors 29 1.2.4 Toll-Like Receptors 30 1.2.5 Serotonin 1A and 3 Receptors 32 1.2.6 Phospholipases A2 33 1.2.7 MAP Kinases 36 1.2.8 Fighting Inflammation, An Ongoing Task 36 1.2.9 Inflammation Assays Using Whole Blood 38 1.3 Arabinogalactan-Proteins 39 1.3.1 Origin and Biological Function of AGPs 40 1.3.2 Effects on Animals 41 1.3.3 The ‘Immunostimulation’ Theory 42 1/188 2. -
Download Product Insert (PDF)
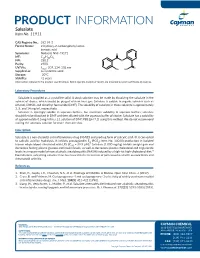
PRODUCT INFORMATION Salsalate Item No. 11911 CAS Registry No.: 552-94-3 Formal Name: 2-hydroxy-2-carboxyphenyl ester- benzoic acid Synonyms: Nobacid, NSC 49171 O MF: C14H10O5 FW: 258.2 O Purity: ≥98% UV/Vis.: λ: 207, 234, 308 nm O max OH HO Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Salsalate is supplied as a crystalline solid. A stock solution may be made by dissolving the salsalate in the solvent of choice, which should be purged with an inert gas. Salsalate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of salsalate in these solvents is approximately 3, 5, and 14 mg/ml, respectively. Salsalate is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, salsalate should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Salsalate has a solubility of approximately 0.5 mg/ml in a 1:1 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description Salsalate is a non-steroidal anti-inflammatory drug (NSAID) and prodrug form of salicylic acid.1 It is converted to salicylic acid by hydrolysis. It inhibits prostaglandin E2 (PGE2; Item No. 14010) production in isolated 2 human whole blood stimulated with LPS (IC50 = 39.9 µM). Salsalate (1,000 mg/kg) inhibits weight gain and decreases fasting plasma glucose and insulin levels, as well as decreases plasma cholesterol and triglyceride levels in a mouse model of non-alcoholic steatohepatitis (NASH) induced by a high-fat high-cholesterol diet.3 Formulations containing salsalate have been used in the treatment of pain associated with osteoarthritis and rheumatoid arthritis. -

Sodium-Salicylate-European-Public-Mrl-Assessment-Report-Epmar-Committee-Veterinary
27 October 2010 EMA/CVMP/562066/2007 Veterinary Medicines and Product Data Management Committee for Medicinal Products for Veterinary Use European public MRL assessment report (EPMAR) Sodium salicylate (turkeys) On 12 October 2010 the European Commission adopted a Regulation1 establishing provisional maximum residue limits for sodium salicylate in turkeys, valid throughout the European Union. These provisional maximum residue limits were based on the favourable opinion and the assessment report adopted by the Committee for Medicinal Products for Veterinary Use. In turkeys, sodium salicylate is intended for use orally as an antipyretic in the treatment of acute respiratory diseases. Sodium salicylate was previously assessed for the purpose of establishing maximum residue limits and was entered in Annex II of Regulation (EEC) No 2377/902 (no MRL required) for topical use in all food producing species except fish and for oral use in bovine and porcine species. Chevita Tierarzneimittel GmbH submitted to the European Medicines Agency on 4 January 2007 an application for the extension of existing entry in Annex II of Regulation (EEC) No 2377/90 for sodium salicylates to turkeys. On 12 December 2007 the Committee for Medicinal Products for Veterinary Use adopted an opinion recommending the amendment of the entry in Annex II of Regulation (EEC) No 2377/90 to include sodium salicylate for oral use in turkeys. The European Commission subsequently returned the opinion to the Committee to consider whether its opinion should be reviewed to take into account issues raised during the Commission’s inter service consultation and in particular to consider whether establishment of maximum residue limits for sodium salicylate in turkeys should be established.