Comparative Effectiveness Review Number 4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Associations of Regular Glucosamine Use with All-Cause and Cause
Epidemiology Ann Rheum Dis: first published as 10.1136/annrheumdis-2020-217176 on 6 April 2020. Downloaded from EPIDEMIOLOGICAL SCIENCE Associations of regular glucosamine use with all- cause and cause- specific mortality: a large prospective cohort study Zhi- Hao Li,1 Xiang Gao,2 Vincent CH Chung,3 Wen- Fang Zhong,1 Qi Fu,3 Yue- Bin Lv,4 Zheng- He Wang,1 Dong Shen,1 Xi- Ru Zhang,1 Pei-Dong Zhang,1 Fu- Rong Li,1 Qing- Mei Huang,1 Qing Chen,1 Wei- Qi Song,1 Xian- Bo Wu,1 Xiao-Ming Shi,4 Virginia Byers Kraus,5 Xingfen Yang,6 Chen Mao 1 Handling editor Josef S ABSTRact Key messages Smolen Objectives To evaluate the associations of regular glucosamine use with all-cause and cause-specific ► Additional material is What is already known about this subject? published online only. To view mortality in a large prospective cohort. ► Although several epidemiological investigations please visit the journal online Methods This population- based prospective cohort indicated that glucosamine use might play a (http:// dx. doi. org/ 10. 1136/ study included 495 077 women and men (mean (SD) role in prevention of cancer, cardiovascular annrheumdis- 2020- 217176). age, 56.6 (8.1) years) from the UK Biobank study. disease (CVD), and other diseases, only a Participants were recruited from 2006 to 2010 and For numbered affiliations see few studies have evaluated the associations were followed up through 2018. We evaluated all-cause end of article. between glucosamine use and mortality mortality and mortality due to cardiovascular disease outcomes, especially for cause- specific Correspondence to (CVD), cancer, respiratory and digestive disease. -

Osteoarthritis (OA) Is a Pain
R OBE 201 CT 1 O Managing Osteoarthritis With Nutritional Supplements Containing Glucosamine, Chondroitin Sulfate, and Avocado/Soybean Unsaponifiables steoarthritis (OA) is a pain- successfully recommending OJHSs treatment algorithm exists for man- ful, progressive degeneration containing a combination of glu- aging patients with OA, acetamin- O of the joint characterized by cosamine, chondroitin sulfate (CS), ophen is a first-line drug recom- progressive cartilage loss, subchon- and avocado/soybean unsaponifi- mended to help control pain and dral bone remodeling, formation of ables (ASU) for the management increase mobility. Acetaminophen periarticular osteophytes, and mild of OA. It will briefly review the is associated with both hepatic and to moderate synovitis accompanied available pharmacokinetics/phar- renal damage, particularly in patients by an increase in pro-inflammatory macodynamics and safety profile who exceed the recommended daily cytokines, chemokines, and a vari- of OJHSs containing a mixture of dose or use it in combination with ety of inflammatory mediators.1 glucosamine, CS, and ASU, outline moderate amounts of alcohol. 6 There is no cure for OA; therefore, strategies to identify appropriate Worsening pain, disease progression, once an individual is diagnosed, patients for OJHSs containing these and inefficacy of acetaminophen managing OA becomes a lifelong ingredients, and provide web-based often necessitate initiating prescrip- process. Although a physician ini- resources (TABLE 1) that will assist tion NSAIDs (such as COX-2 tially diagnoses OA, pharmacists are pharmacists in educating and coun- inhibitors), which carry the risk of the most accessible health care pro- seling patients. gastrointestinal effects (e.g., gas- fessional and play an integral role tropathy), renal toxicities, and seri- in managing each patient’s joint CURRENT RECOMMENDATIONS ous cardiovascular events. -

Salsalate Tablets, USP 500 Mg and 750 Mg Rx Only
SALSALATE RX- salsalate tablet, film coated ANDAPharm LLC Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here. ---------- Salsalate Tablets, USP 500 mg and 750 mg Rx Only Cardiovascular Risk NSAIDs may cause an increase risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (See WARNINGS and CLINICAL TRIALS). Salsalate tablets, USP is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery (See WARNINGS). Gastrointestinal Risk NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS). DESCRIPTION Salsalate, is a nonsteroidal anti-inflammatory agent for oral administration. Chemically, salsalate (salicylsalicylic acid or 2-hydroxybenzoic acid, 2-carboxyphenyl ester) is a dimer of salicylic acid; its structural formula is shown below. Chemical Structure: Inactive Ingredients: Colloidal Silicon Dioxide, D&C Yellow #10 Aluminum Lake, Hypromellose, Microcrystalline Cellulose, Sodium Starch Glycolate, Stearic Acid, Talc, Titanium Dioxide, Triacetin. CLINICAL PHARMACOLOGY Salsalate is insoluble in acid gastric fluids (<0.1 mg/mL at pH 1.0), but readily soluble in the small intestine where it is partially hydrolyzed to two molecules of salicylic acid. -
Download Product Insert (PDF)
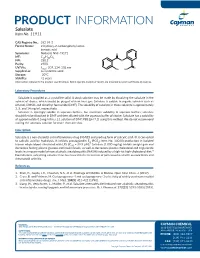
PRODUCT INFORMATION Salsalate Item No. 11911 CAS Registry No.: 552-94-3 Formal Name: 2-hydroxy-2-carboxyphenyl ester- benzoic acid Synonyms: Nobacid, NSC 49171 O MF: C14H10O5 FW: 258.2 O Purity: ≥98% UV/Vis.: λ: 207, 234, 308 nm O max OH HO Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Salsalate is supplied as a crystalline solid. A stock solution may be made by dissolving the salsalate in the solvent of choice, which should be purged with an inert gas. Salsalate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of salsalate in these solvents is approximately 3, 5, and 14 mg/ml, respectively. Salsalate is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, salsalate should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Salsalate has a solubility of approximately 0.5 mg/ml in a 1:1 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description Salsalate is a non-steroidal anti-inflammatory drug (NSAID) and prodrug form of salicylic acid.1 It is converted to salicylic acid by hydrolysis. It inhibits prostaglandin E2 (PGE2; Item No. 14010) production in isolated 2 human whole blood stimulated with LPS (IC50 = 39.9 µM). Salsalate (1,000 mg/kg) inhibits weight gain and decreases fasting plasma glucose and insulin levels, as well as decreases plasma cholesterol and triglyceride levels in a mouse model of non-alcoholic steatohepatitis (NASH) induced by a high-fat high-cholesterol diet.3 Formulations containing salsalate have been used in the treatment of pain associated with osteoarthritis and rheumatoid arthritis. -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

Salicylate, Diflunisal and Their Metabolites Inhibit CBP/P300 and Exhibit Anticancer Activity
RESEARCH ARTICLE Salicylate, diflunisal and their metabolites inhibit CBP/p300 and exhibit anticancer activity Kotaro Shirakawa1,2,3,4, Lan Wang5,6, Na Man5,6, Jasna Maksimoska7,8, Alexander W Sorum9, Hyung W Lim1,2, Intelly S Lee1,2, Tadahiro Shimazu1,2, John C Newman1,2, Sebastian Schro¨ der1,2, Melanie Ott1,2, Ronen Marmorstein7,8, Jordan Meier9, Stephen Nimer5,6, Eric Verdin1,2* 1Gladstone Institutes, University of California, San Francisco, United States; 2Department of Medicine, University of California, San Francisco, United States; 3Department of Hematology and Oncology, Kyoto University, Kyoto, Japan; 4Graduate School of Medicine, Kyoto University, Kyoto, Japan; 5University of Miami, Gables, United States; 6Sylvester Comprehensive Cancer Center, Miami, United States; 7Perelman School of Medicine, University of Pennsylvania, Philadelphia, United States; 8Department of Biochemistry and Biophysics, Abramson Family Cancer Research Institute, Philadelphia, United States; 9Chemical Biology Laboratory, National Cancer Institute, Frederick, United States Abstract Salicylate and acetylsalicylic acid are potent and widely used anti-inflammatory drugs. They are thought to exert their therapeutic effects through multiple mechanisms, including the inhibition of cyclo-oxygenases, modulation of NF-kB activity, and direct activation of AMPK. However, the full spectrum of their activities is incompletely understood. Here we show that salicylate specifically inhibits CBP and p300 lysine acetyltransferase activity in vitro by direct *For correspondence: everdin@ competition with acetyl-Coenzyme A at the catalytic site. We used a chemical structure-similarity gladstone.ucsf.edu search to identify another anti-inflammatory drug, diflunisal, that inhibits p300 more potently than salicylate. At concentrations attainable in human plasma after oral administration, both salicylate Competing interests: The and diflunisal blocked the acetylation of lysine residues on histone and non-histone proteins in cells. -

Identification of Glucosamine Hydrochloride Diclofenac Sodium Interaction Products by Chromatography-Mass Spectrometry
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2014, 6(5):761-767 ISSN : 0975-7384 Research Article CODEN(USA) : JCPRC5 Identification of glucosamine hydrochloride diclofenac sodium interaction products by chromatography-mass spectrometry А. А. Sichkar Industrial Pharmacy Department, National University of Pharmacy, Kharkiv, Ukraine _____________________________________________________________________________________________ ABSTRACT Researches of chemical transformation products of diclofenac sodium and glucosamine hydrochloride at their joint presence have been carried out by means of the gas chromatography-mass spectrometry. Mechanical mixes of substances were investigated before and after technological operations of humidifying and drying. It has been proven that one medicinal substance influences another. The formation of several reaction products during the chemical interaction between diclofenac sodium and glucosamine hydrochloride has been shown. Key words: diclofenac sodium, glucosamine hydrochloride, chemical transformation products, gas chromatography-mass spectrometry. _____________________________________________________________________________________________ INTRODUCTION Diclofenac sodium is in the first line of nonsteroidal anti-inflammatory drugs (NSAID) for the pain relief and reduction of an inflammatory process activity in most diseases of connective tissue and joints over decades. However, along with pronounced therapeutic effect the use of this NSAID is associated with several side effects, including lesions of the gastrointestinal tract and inhibition of the metabolism of articular cartilage [1, 2, 3, 4]. Creation of new combined drugs with NSAIDs and other medicinal substances is one of the major direction of NSAIDs pharmacological properties spectrum spread and reduce their toxicity [5, 6, 7, 8]. Thus, in the National University of Pharmacy at the Department of Clinical Pharmacology and Clinical Pharmacy under the supervision of prof. Zupanets I.A. -

ACPA Guide to Pain Management
[Document title] [Document subtitle] Abstract [Draw your reader in with an engaging abstract. It is typically a short summary of the document. When you’re ready to add your content, just click here and start typing.] ACPA [Email address] 1 ACPA Resource Guide To Chronic Pain Management An Integrated Guide to Medical, Interventional, Behavioral, Pharmacologic and Rehabilitation Therapies 2019 Edition American Chronic Pain Association P.O. Box 850 Rocklin, CA 95677 Tel 800-533-3231 Fax 916-652-8190 E-mail [email protected] Web Site http://www.theacpa.org Copyright 2019 American Chronic Pain Association, Inc. All rights reserved. No portion of this book may be reproduced without permission of the American Chronic Pain Association, Inc. 2 Table of Contents A STATEMENT FROM THE ACPA BOARD OF DIRECTORS ...........................................................................................................................5 INTRODUCTION ........................................................................................................................................................................................................6 OVERVIEW OF CHRONIC PAIN TREATMENT ..................................................................................................................................................8 WHAT DOES SUCCESSFUL PAIN TREATMENT LOOK LIKE? .......................................................................................................................8 PAIN TYPES, SOURCES & CLASSIFICATION .....................................................................................................................................................9 -

Treatment on Gouty Arthritis Animal Model
Journal of Applied Pharmaceutical Science Vol. 7 (07), pp. 202-207, July, 2017 Available online at http://www.japsonline.com DOI: 10.7324/JAPS.2017.70729 ISSN 2231-3354 Anti-inflammatory and anti-hyperuricemia properties of chicken feet cartilage: treatment on gouty arthritis animal model Tri Dewanti Widyaningsih*, Widya Dwi Rukmi Putri, Erni Sofia Murtini, Nia Rochmawati, Debora Nangin Department of Agricultural Product Technology, Faculty of Agricultural Technology, Brawijaya University, Malang 65145, Indonesia. ABSTRACT ARTICLE INFO Article history: Gout is a form of inflammatory arthritis caused by the deposition of uric acid. The therapeutic approach to gout Received on: 22/03/2017 is mainly divided by the treatment of inflammation and the management of serum urate level. This study aim to Accepted on: 13/05/2017 investigate whether chondroitin sulfate (CS) and glucosamine in chicken feet cartilage powder (CFE) and Available online: 30/07/2017 aqueous extract (AE) are able to decrease serum urate level and inflammation in animal model of gouty arthritis. CFE and AE were evaluated in vitro for xanthine oxidase (XO) inhibition. The anti-hyperuricemic activity and Key words: liver XO inhibition were evaluated in vivo on oxonate-induced hyperuricemia rats. Anti-inflammatory property Chicken feet cartilage, gout, was also determined on monosodium urate (MSU) crystal-induced paw edema model. CFE and AE hyperuricemia, monosodium supplementation showed urate-lowering activity. However, both treatments were not able to inhibit in vitro and urate, inflammation. in vivo XO activity. In MSU crystal-induced mice, the levels of paw swelling and lipid peroxidation were increased; in addition, a decrease in the activities of SOD and changes in the expression of CD11b+TNF-α and CD11b+IL-6 of the spleen were demonstrated. -

Medications & Supplements to Avoid Before Procedures
Medications & Supplements to Avoid Before Procedures Do not ingest any brand of aspirin, or any aspirin-containing medication, any MAO inhibiting, or any serotonin medications, for 14 prior to and 14 days after surgery. Disclose every medication, supplement, etc. With Dr. Rau and your anesthesiologist. Aspirin and aspirin-containing products, as well as some supplements and herbals, may inhibit blood clotting and cause difficulties during and after surgery. If you need an aspirin-free fever reducer and pain reliever, take Tylenol. Also, if you smoke, you must refrain for at least a month prior to a month after your surgery date. Smoking significantly reduces your body’s circulation and vascularity, meaning that your tissues won’t receive all the oxygen needed for proper healing. DIET PILLS, FAT LOSS SUPPLEMENTS AND STACKERS: Please stop taking these pills at least 2 weeks before surgery. Many of these pills contain anticoagulants and can seriously impede your body's ability to clot sufficiently, resulting in hemorrhaging. Many of them also contain ephedra and caffeine, which can affect your anesthetic medications. Remember: if you take antibiotics or if you stop oral contraceptive pills for surgery, use an alternative method of birth control. A Aspirin, Advil, Actifed, Acuprin, Addaprin, Alka Seltzer, Alpha Omega (fish oil), Aluprin, Amitriptyline, Anacin, Ansaid, Anodynos, Analval, Anodynos, Ansaid, Argesic, Arthra-G, Arthralgen, Arthropan, Ascodeen, Ascriptin, Aspir-lox, Asperi-mox, Aspirbuf, Aspercin, Aspergum, Axotal, Azdone, -

Arthritis Treatment Comparison Arthritis Treatment Comparison
ARTHRITIS TREATMENT COMPARISON ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA CHELATING AGENTS Penicillamine Cap: 250mg ✓ (Cuprimine) Penicillamine Tab: 250mg ✓ (Depen) CYCLIC POLYPEPTIDE IMMUNOSUPPRESSANTS Cyclosporine Cap: 25mg, 100mg; ✓ (Gengraf, Neoral) Sol: 100mg/mL CYCLOOXYGENASE-2 INHIBITORS Celecoxib Cap: 50mg, 100mg, ✓ ✓ ✓ ✓ (Celebrex) 200mg, 400mg DIHYDROFOLIC ACID REDUCTASE INHIBITORS Methotrexate Inj: 25mg/mL; ✓ ✓ Tab: 2.5mg Methotrexate Tab: 5mg, 7.5mg, ✓ ✓ (Trexall) 10mg, 15mg INTERLEUKIN RECEPTOR ANTAGONISTS Anakinra Inj: 100mg/0.67mL ✓ (Kineret) Tocilizumab Inj: 20mg/mL, ✓ ✓ (Actemra) 162mg/0.9mL GOLD COMPOUNDS Auranofin Cap: 3mg ✓ (Ridaura) Gold sodium thiomalate Inj: 50mg/mL ✓ ✓ (Myochrysine) HYALURONAN AND DERIVATIVES Hyaluronan Inj: 30mg/2mL ✓ (Orthovisc) Sodium hyaluronate Inj: 1% ✓ (Euflexxa) Sodium hyaluronate Inj: 10mg/mL ✓ (Hyalgan) Sodium hyaluronate Inj: 2.5mL ✓ (Supartz) HYLAN POLYMERS Hylan G-F 20 Inj: 8mg/mL ✓ (Synvisc, Synvisc One) KINASE INHIBITORS Tofacitinib Tab: 5mg ✓ (Xeljanz) MONOCLONAL ANTIBODIES Ustekinumab Inj: 45mg/0.5mL, ✓ (Stelara) 90mg/mL MONOCLONAL ANTIBODIES/CD20-BLOCKERS Rituximab Inj: 100mg/10mL, ✓ (Rituxan) 500mg/50mL (Continued) ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA MONOCLONAL ANTIBODIES/TNF-BLOCKERS Adalimumab Inj: 20mg/0.4mL, ✓ ✓ ✓ ✓ (Humira) 40mg/0.8mL Golimumab Inj: 50mg/0.5mL, ✓ ✓ ✓ (Simponi) 100mg/mL Infliximab Inj: 100mg ✓ ✓ ✓ (Remicade) NON-STEROIDAL ANTI-INFLAMMATORY DRUGS -

List of a FEW of MANY Aspirin-Like Or Herbal Supplement Products To
1809 E 13th St. Suite 100 -300 Tulsa, OK 74104 (918)582-6800 MEDICATION AND PRODUCTS TO BE AVOIDED PRIOR TO SURGERY **Do not stop taking blood pressure, diabetic, or prescribed medications that are not blood thinners. You will be advised at your pre-op when to stop these medications prior to surgery. If you have any question as to whether it is safe to stop a medication, please check with the prescribing physician. Aspirin and other non-steroidal anti-inflammatory drugs (NSAID’s), such as Motrin are strong anti-coagulants which can cause bleeding problems in normal individuals. In addition to these Aspirin- like medications, Vitamins and many herbal supplements (such as Garlic, Ginkgo, Ginseng, Flaxseed, Ginger, Feverfew, Bilberry, Chamomile, Selenium) can cause bleeding or adverse physiologic effects during surgery. If you are on a blood thinner or antiplatelet medication such as Eliquis, Coumadin (warfarin), Plavix (clopidogrel), Pletal (cilostazol)Pradaxa or Xarelto, you must stop these medications prior to surgery. Please follow the prescribing physician’s recommendation for stopping the medications. Do not restart blood thinners until your physician advises. Patients preparing for surgery must stop all sources of Aspirin, Aspirin like products, Vitamins and all Herbal Supplements or Diet Pills for 7 days prior to surgery and 5 days after surgery. Below are a FEW OF MANY Aspirin-like or Herbal Supplement products to be avoided prior to surgery. Advil Congesprin Chewable Fish Oil Nabumetone Selenium Aggrenox Compounded Creams Flaxseed Nalfon Sine – Aid Aleve Contac Flurbiprofen Naprelan Sine – Off Sinus Alka – Seltzers Cope Four Way Cold Tabs Naprosyn Sinutab Anacin Coricidin Gaysal-S Naproxen SK – 65 Anaprox Cosprin Garlic (Allium Sativum) Neocylate Soma Anadynos Coumadin Gelprin Norgesic Stanback Ansaid Damason P Gemnisin Novnaproxen Stendin APC Darvon Ginger Novodipiradrol St.