PRIMA1 Mutation: a New Cause of Nocturnal Frontal Lobe Epilepsy Michael S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Investigation of the Underlying Hub Genes and Molexular Pathogensis in Gastric Cancer by Integrated Bioinformatic Analyses
bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Investigation of the underlying hub genes and molexular pathogensis in gastric cancer by integrated bioinformatic analyses Basavaraj Vastrad1, Chanabasayya Vastrad*2 1. Department of Biochemistry, Basaveshwar College of Pharmacy, Gadag, Karnataka 582103, India. 2. Biostatistics and Bioinformatics, Chanabasava Nilaya, Bharthinagar, Dharwad 580001, Karanataka, India. * Chanabasayya Vastrad [email protected] Ph: +919480073398 Chanabasava Nilaya, Bharthinagar, Dharwad 580001 , Karanataka, India bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract The high mortality rate of gastric cancer (GC) is in part due to the absence of initial disclosure of its biomarkers. The recognition of important genes associated in GC is therefore recommended to advance clinical prognosis, diagnosis and and treatment outcomes. The current investigation used the microarray dataset GSE113255 RNA seq data from the Gene Expression Omnibus database to diagnose differentially expressed genes (DEGs). Pathway and gene ontology enrichment analyses were performed, and a proteinprotein interaction network, modules, target genes - miRNA regulatory network and target genes - TF regulatory network were constructed and analyzed. Finally, validation of hub genes was performed. The 1008 DEGs identified consisted of 505 up regulated genes and 503 down regulated genes. -

Neurological Disorders, Genetic Correlations, and the Role of Exome Sequencing
Journal of Translational Science Review Article ISSN: 2059-268X Neurological disorders, genetic correlations, and the role of exome sequencing Tony L Brown1* and Theresa M Meloche2 1Columbia University, USA 2Advanced Research and Human Development Institute, USA Abstract Genomic information access and utilization by researchers and clinicians have barely begun the journey for fulfillment of their full potential in the research and clinical arenas. Exciting is the potential depth and breadth of research, clinical applications, and more personalized medicine, that remain on the horizon. Exome sequencing has clarified the responsibilities of over 130 genes, greatly expanding the medical genetics database and enabling the development of orphan disease- based pharmaceuticals. The focus of our research efforts was to review several literature sources related to rare genomic disease research and exome sequencing, as well as to review the new research and diagnostic strategies that were utilized. Using a systems approach, under discussion are neurology, neuropathy, and the central nervous and musculoskeletal systems. Also discussed will be the topics of inborn errors of metabolism, and the genetic targets related to developmental delay. Recommendations for future research will also be discussed. Exome sequencing neuronal ceroid lipofuscinoses the most common group of inherited neurological degenerative disorders [6]. Whether examining the A review of new strategies for rare genomic disease research mitochondrial defect implicated in prenatal ventriculomegaly -

Gene Promoter and Exon DNA Methylation Changes in Colon
Molnár et al. BMC Cancer (2018) 18:695 https://doi.org/10.1186/s12885-018-4609-x RESEARCH ARTICLE Open Access Gene promoter and exon DNA methylation changes in colon cancer development – mRNA expression and tumor mutation alterations Béla Molnár1,2*†, Orsolya Galamb1†, Bálint Péterfia2, Barnabás Wichmann1, István Csabai3, András Bodor3,4, Alexandra Kalmár1, Krisztina Andrea Szigeti2, Barbara Kinga Barták2, Zsófia Brigitta Nagy2, Gábor Valcz1, Árpád V. Patai2, Péter Igaz1,2 and Zsolt Tulassay1,2 Abstract Background: DNA mutations occur randomly and sporadically in growth-related genes, mostly on cytosines. Demethylation of cytosines may lead to genetic instability through spontaneous deamination. Aims were whole genome methylation and targeted mutation analysis of colorectal cancer (CRC)-related genes and mRNA expression analysis of TP53 pathway genes. Methods: Long interspersed nuclear element-1 (LINE-1) BS-PCR followed by pyrosequencing was performed for the estimation of global DNA metlyation levels along the colorectal normal-adenoma-carcinoma sequence. Methyl capture sequencing was done on 6 normal adjacent (NAT), 15 adenomatous (AD) and 9 CRC tissues. Overall quantitative methylation analysis, selection of top hyper/hypomethylated genes, methylation analysis on mutation regions and TP53 pathway gene promoters were performed. Mutations of 12 CRC-related genes (APC, BRAF, CTNNB1, EGFR, FBXW7, KRAS, NRAS, MSH6, PIK3CA, SMAD2, SMAD4, TP53) were evaluated. mRNA expression of TP53 pathway genes was also analyzed. Results: According to the LINE-1 methylation results, overall hypomethylation was observed along the normal- adenoma-carcinoma sequence. Within top50 differential methylated regions (DMRs), in AD-N comparison TP73, NGFR, PDGFRA genes were hypermethylated, FMN1, SLC16A7 genes were hypomethylated. -

Nicotinic Receptors in Sleep-Related Hypermotor Epilepsy: Pathophysiology and Pharmacology
brain sciences Review Nicotinic Receptors in Sleep-Related Hypermotor Epilepsy: Pathophysiology and Pharmacology Andrea Becchetti 1,* , Laura Clara Grandi 1 , Giulia Colombo 1 , Simone Meneghini 1 and Alida Amadeo 2 1 Department of Biotechnology and Biosciences, University of Milano-Bicocca, 20126 Milano, Italy; [email protected] (L.C.G.); [email protected] (G.C.); [email protected] (S.M.) 2 Department of Biosciences, University of Milano, 20133 Milano, Italy; [email protected] * Correspondence: [email protected] Received: 13 October 2020; Accepted: 21 November 2020; Published: 25 November 2020 Abstract: Sleep-related hypermotor epilepsy (SHE) is characterized by hyperkinetic focal seizures, mainly arising in the neocortex during non-rapid eye movements (NREM) sleep. The familial form is autosomal dominant SHE (ADSHE), which can be caused by mutations in genes encoding subunits of the neuronal nicotinic acetylcholine receptor (nAChR), Na+-gated K+ channels, as well as non-channel signaling proteins, such as components of the gap activity toward rags 1 (GATOR1) macromolecular complex. The causative genes may have different roles in developing and mature brains. Under this respect, nicotinic receptors are paradigmatic, as different pathophysiological roles are exerted by distinct nAChR subunits in adult and developing brains. The widest evidence concerns α4 and β2 subunits. These participate in heteromeric nAChRs that are major modulators of excitability in mature neocortical circuits as well as regulate postnatal synaptogenesis. However, growing evidence implicates mutant α2 subunits in ADSHE, which poses interpretive difficulties as very little is known about the function of α2-containing (α2*) nAChRs in the human brain. -

Robles JTO Supplemental Digital Content 1
Supplementary Materials An Integrated Prognostic Classifier for Stage I Lung Adenocarcinoma based on mRNA, microRNA and DNA Methylation Biomarkers Ana I. Robles1, Eri Arai2, Ewy A. Mathé1, Hirokazu Okayama1, Aaron Schetter1, Derek Brown1, David Petersen3, Elise D. Bowman1, Rintaro Noro1, Judith A. Welsh1, Daniel C. Edelman3, Holly S. Stevenson3, Yonghong Wang3, Naoto Tsuchiya4, Takashi Kohno4, Vidar Skaug5, Steen Mollerup5, Aage Haugen5, Paul S. Meltzer3, Jun Yokota6, Yae Kanai2 and Curtis C. Harris1 Affiliations: 1Laboratory of Human Carcinogenesis, NCI-CCR, National Institutes of Health, Bethesda, MD 20892, USA. 2Division of Molecular Pathology, National Cancer Center Research Institute, Tokyo 104-0045, Japan. 3Genetics Branch, NCI-CCR, National Institutes of Health, Bethesda, MD 20892, USA. 4Division of Genome Biology, National Cancer Center Research Institute, Tokyo 104-0045, Japan. 5Department of Chemical and Biological Working Environment, National Institute of Occupational Health, NO-0033 Oslo, Norway. 6Genomics and Epigenomics of Cancer Prediction Program, Institute of Predictive and Personalized Medicine of Cancer (IMPPC), 08916 Badalona (Barcelona), Spain. List of Supplementary Materials Supplementary Materials and Methods Fig. S1. Hierarchical clustering of based on CpG sites differentially-methylated in Stage I ADC compared to non-tumor adjacent tissues. Fig. S2. Confirmatory pyrosequencing analysis of DNA methylation at the HOXA9 locus in Stage I ADC from a subset of the NCI microarray cohort. 1 Fig. S3. Methylation Beta-values for HOXA9 probe cg26521404 in Stage I ADC samples from Japan. Fig. S4. Kaplan-Meier analysis of HOXA9 promoter methylation in a published cohort of Stage I lung ADC (J Clin Oncol 2013;31(32):4140-7). Fig. S5. Kaplan-Meier analysis of a combined prognostic biomarker in Stage I lung ADC. -

Content Based Search in Gene Expression Databases and a Meta-Analysis of Host Responses to Infection
Content Based Search in Gene Expression Databases and a Meta-analysis of Host Responses to Infection A Thesis Submitted to the Faculty of Drexel University by Francis X. Bell in partial fulfillment of the requirements for the degree of Doctor of Philosophy November 2015 c Copyright 2015 Francis X. Bell. All Rights Reserved. ii Acknowledgments I would like to acknowledge and thank my advisor, Dr. Ahmet Sacan. Without his advice, support, and patience I would not have been able to accomplish all that I have. I would also like to thank my committee members and the Biomed Faculty that have guided me. I would like to give a special thanks for the members of the bioinformatics lab, in particular the members of the Sacan lab: Rehman Qureshi, Daisy Heng Yang, April Chunyu Zhao, and Yiqian Zhou. Thank you for creating a pleasant and friendly environment in the lab. I give the members of my family my sincerest gratitude for all that they have done for me. I cannot begin to repay my parents for their sacrifices. I am eternally grateful for everything they have done. The support of my sisters and their encouragement gave me the strength to persevere to the end. iii Table of Contents LIST OF TABLES.......................................................................... vii LIST OF FIGURES ........................................................................ xiv ABSTRACT ................................................................................ xvii 1. A BRIEF INTRODUCTION TO GENE EXPRESSION............................. 1 1.1 Central Dogma of Molecular Biology........................................... 1 1.1.1 Basic Transfers .......................................................... 1 1.1.2 Uncommon Transfers ................................................... 3 1.2 Gene Expression ................................................................. 4 1.2.1 Estimating Gene Expression ............................................ 4 1.2.2 DNA Microarrays ...................................................... -

Genome-Wide DNA Methylation Scan in Major Depressive Disorder
Genome-Wide DNA Methylation Scan in Major Depressive Disorder Sarven Sabunciyan1., Martin J. Aryee2,5., Rafael A. Irizarry1,3,5, Michael Rongione9, Maree J. Webster7, Walter E. Kaufman3,6, Peter Murakami3, Andree Lessard8, Robert H. Yolken1, Andrew P. Feinberg3,4, James B. Potash9*, GenRED Consortium" 1 Department of Pediatrics, Stanley Division of Developmental Neurovirology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland, United States of America, 2 Department of Oncology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland, United States of America, 3 Epigenetics Center, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland, United States of America, 4 Division of Molecular Medicine, Department of Medicine, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland, United States of America, 5 Department of Biostatistics, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland, United States of America, 6 Center for Genetic Disorders of Cognition and Behavior, Kennedy Krieger Institute, Baltimore, Maryland, United States of America, 7 Uniformed Services University of the Health Sciences, Bethesda, Maryland, United States of America, 8 Maryland Psychiatric Research Center, University of Maryland School of Medicine, Baltimore, Maryland, United States of America, 9 Department of Psychiatry, University of Iowa, Iowa City, Iowa, United States of America Abstract While genome-wide association studies are ongoing to identify sequence variation influencing susceptibility to major depressive disorder (MDD), epigenetic marks, such as DNA methylation, which can be influenced by environment, might also play a role. Here we present the first genome-wide DNA methylation (DNAm) scan in MDD. We compared 39 postmortem frontal cortex MDD samples to 26 controls. -
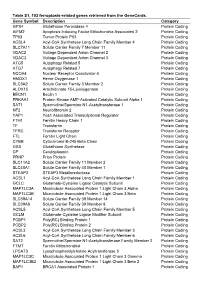
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

Supplementary Figure 1. Sleep Traits Are Phenotypically and Genetically Correlated in Men and Women
Excessive Excessive Insomnia Sleep Insomnia Sleep Daytime Chronotype Daytime Chronotype Symptoms Duration Symptoms Duration Sleepiness Sleepiness a. b. Excessive Daytime Excessive Daytime r= 0.11 r= -0.02 r= -0.01 r= 0.07 r= -0.03 r= -0.02 Sleepiness Sleepiness Insomnia Symptoms p< 0.001 r= -Insomnia0.18 rSymptoms= 0.00 p< 0.001 r= -0.32 r= 0.01 Sleep Sleep p< 0.001 p< 0.001 r= 0.02 p< 0.001 p< 0.001 r= 0.03 Duration Duration Chronotype p= 0.005 p= 0.641 p< 0.001Chronotype p< 0.001 p= 0.176 p< 0.001 Excessive Excessive Insomnia Sleep Insomnia Sleep Daytime Chronotype Daytime Chronotype c. Symptoms Duration d. Symptoms Duration Sleepiness Sleepiness Excessive Daytime Excessive Daytime r = 0.38 r = -0.37 r = 0.01 rg= 0.17 rg= -0.13 rg= -0.11 Sleepiness g g Sleepinessg -6 Insomnia Symptoms p= 8.39x10 rg= -Insomnia0.44 r Symptomsg= 0.12 p= 0.053 rg= -0.52 rg= -0.10 Sleep -5 Sleep -12 p= 0.006 p= 4.91x10 r = -0.02 p= 0.163 p= 1.65x10 rg= 0.11 Duration Durationg Chronotype p= 0.852 p= 0.096 p= 0.872Chronotype p= 0.104 p= 0.113 p= 0.142 Supplementary Figure 1. Sleep traits are phenotypically and genetically correlated in men and women. Phenotypic correlation between the reported sleep traits, using Spearman correlation are shown stratified by sex (a. men, b. women). Color scale represents the strength of the correlation. Genetic correlation between the reported sleep traits shown stratified by sex, as measured by LDSC (c. -

Sheet1 Page 1 Gene Symbol Gene Description Entrez Gene ID
Sheet1 RefSeq ID ProbeSets Gene Symbol Gene Description Entrez Gene ID Sequence annotation Seed matches location(s) Ago-2 binding specific enrichment (replicate 1) Ago-2 binding specific enrichment (replicate 2) OE lysate log2 fold change (replicate 1) OE lysate log2 fold change (replicate 2) Probability NM_022823 218843_at FNDC4 Homo sapiens fibronectin type III domain containing 4 (FNDC4), mRNA. 64838 TR(1..1649)CDS(367..1071) 1523..1530 3.73 1.77 -1.91 -0.39 1 NM_003919 204688_at SGCE Homo sapiens sarcoglycan, epsilon (SGCE), transcript variant 2, mRNA. 8910 TR(1..1709)CDS(112..1425) 1495..1501 3.09 1.56 -1.02 -0.27 1 NM_006982 206837_at ALX1 Homo sapiens ALX homeobox 1 (ALX1), mRNA. 8092 TR(1..1320)CDS(5..985) 916..923 2.99 1.93 -0.19 -0.33 1 NM_019024 233642_s_at HEATR5B Homo sapiens HEAT repeat containing 5B (HEATR5B), mRNA. 54497 TR(1..6792)CDS(97..6312) 5827..5834,4309..4315 3.28 1.51 -0.92 -0.23 1 NM_018366 223431_at CNO Homo sapiens cappuccino homolog (mouse) (CNO), mRNA. 55330 TR(1..1546)CDS(96..749) 1062..1069,925..932 2.89 1.51 -1.2 -0.41 1 NM_032436 226194_at C13orf8 Homo sapiens chromosome 13 open reading frame 8 (C13orf8), mRNA. 283489 TR(1..3782)CDS(283..2721) 1756..1762,3587..3594,1725..1731,3395..3402 2.75 1.72 -1.38 -0.34 1 NM_031450 221534_at C11orf68 Homo sapiens chromosome 11 open reading frame 68 (C11orf68), mRNA. 83638 TR(1..1568)CDS(153..908) 967..973 3.07 1.35 -0.72 -0.06 1 NM_033318 225795_at,225794_s_at C22orf32 Homo sapiens chromosome 22 open reading frame 32 (C22orf32), mRNA. -

Visual Genome-Wide Rnai Screening to Identify Human Host Factors
Visual Genome-Wide RNAi Screening to Identify Human Host Factors Required for Trypanosoma cruzi Infection Auguste Genovesio, Miriam Giardini, Yong-Jun Kwon, Fernando de Macedo Dossin, Seo Yeon Choi, Nam Youl Kim, Hi Chul Kim, Sung Yong Jung, Sergio Schenkman, Igor Almeida, et al. To cite this version: Auguste Genovesio, Miriam Giardini, Yong-Jun Kwon, Fernando de Macedo Dossin, Seo Yeon Choi, et al.. Visual Genome-Wide RNAi Screening to Identify Human Host Factors Required for Try- panosoma cruzi Infection. PLoS ONE, Public Library of Science, 2011, 6 (5), pp.e19733. 10.1371/jour- nal.pone.0019733. hal-02902036 HAL Id: hal-02902036 https://hal.archives-ouvertes.fr/hal-02902036 Submitted on 17 Jul 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Visual Genome-Wide RNAi Screening to Identify Human Host Factors Required for Trypanosoma cruzi Infection Auguste Genovesio1., Miriam A. Giardini2., Yong-Jun Kwon3,4., Fernando de Macedo Dossin2, Seo Yeon Choi3, Nam Youl Kim3, Hi Chul Kim3, Sung Yong Jung3, Sergio Schenkman5, Igor C. Almeida6, Neil Emans7*, -

Gene Modules Associated with Human Diseases Revealed by Network
bioRxiv preprint doi: https://doi.org/10.1101/598151; this version posted June 15, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Gene modules associated with human diseases revealed by network analysis Shisong Ma1,2*, Jiazhen Gong1†, Wanzhu Zuo1†, Haiying Geng1, Yu Zhang1, Meng Wang1, Ershang Han1, Jing Peng1, Yuzhou Wang1, Yifan Wang1, Yanyan Chen1 1. Hefei National Laboratory for Physical Sciences at the Microscale, School of Life Sciences, University of Science and Technology of China, Hefei, Anhui 230027, China 2. School of Data Science, University of Science and Technology of China, Hefei, Anhui 230027, China * To whom correspondence should be addressed. Email: [email protected] † These authors contribute equally. 1 bioRxiv preprint doi: https://doi.org/10.1101/598151; this version posted June 15, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. ABSTRACT Despite many genes associated with human diseases have been identified, disease mechanisms often remain elusive due to the lack of understanding how disease genes are connected functionally at pathways level. Within biological networks, disease genes likely map to modules whose identification facilitates etiology studies but remains challenging. We describe a systematic approach to identify disease-associated gene modules.