Psychedelic Experience Reports Involving Lithium Or Lamotrigine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

4/23/2015 1 •Psychedelics Or Hallucinogens
4/23/2015 Hallucinogens •Psychedelics or This “classic” hallucinogen column The 2 groups below are quite different produce similar effects From the classic hallucinogens Hallucinogens Drugs Stimulating 5HT Receptors Drugs BLOCKING ACH Receptors • aka “psychotomimetics” LSD Nightshade(Datura) Psilocybin Mushrooms Jimsonweed Morning Glory Seeds Atropine Dimethyltryptamine Scopolamine What do the very mixed group of hallucinogens found around the world share in common? •Drugs Resembling NE Drugs BLOCKING Glutamate Receptors •Peyote cactus Phencyclidine (PCP) •Mescaline Ketamine All contain something that resembles a •Methylated amphetamines like MDMA High dose dextromethorphan •Nutmeg neurotransmitter •New synthetic variations (“bath salts”) •5HT-Like Hallucinogens •LSD History • Serotonin • created by Albert Hofmann for Sandoz Pharmaceuticals LSD • was studying vasoconstriction produced by ergot alkaloids LSD • initial exposure was accidental absorption thru skin • so potent ED is in millionths of a gram (25-250 micrograms) & must be delivered on something else (sugar cube, gelatin square, paper) Psilocybin Activate 5HT2 receptors , especially in prefrontal cortex and limbic areas, but is not readily metabolized •Characteristics of LSD & Other “Typical” •Common Effects Hallucinogens • Sensory distortions (color, size, shape, movement), • Autonomic (mostly sympathetic) changes occur first constantly changing (relatively mild) • Vivid closed eye imagery • Sensory/perceptual changes follow • Synesthesia (crossing of senses – e.g. hearing music -

Hallucinogens - LSD, Peyote, Psilocybin, and PCP
Information for Behavioral Health Providers in Primary Care Hallucinogens - LSD, Peyote, Psilocybin, and PCP What are Hallucinogens? Hallucinogenic compounds found in some plants and mushrooms (or their extracts) have been used— mostly during religious rituals—for centuries. Almost all hallucinogens contain nitrogen and are classified as alkaloids. Many hallucinogens have chemical structures similar to those of natural neurotransmitters (e.g., acetylcholine-, serotonin-, or catecholamine-like). While the exact mechanisms by which hallucinogens exert their effects remain unclear, research suggests that these drugs work, at least partially, by temporarily interfering with neurotransmitter action or by binding to their receptor sites. This InfoFacts will discuss four common types of hallucinogens: LSD (d-lysergic acid diethylamide) is one of the most potent mood-changing chemicals. It was discovered in 1938 and is manufactured from lysergic acid, which is found in ergot, a fungus that grows on rye and other grains. Peyote is a small, spineless cactus in which the principal active ingredient is mescaline. This plant has been used by natives in northern Mexico and the southwestern United States as a part of religious ceremonies. Mescaline can also be produced through chemical synthesis. Psilocybin (4-phosphoryloxy-N, N-dimethyltryptamine) is obtained from certain types of mushrooms that are indigenous to tropical and subtropical regions of South America, Mexico, and the United States. These mushrooms typically contain less than 0.5 percent psilocybin plus trace amounts of psilocin, another hallucinogenic substance. PCP (phencyclidine) was developed in the 1950s as an intravenous anesthetic. Its use has since been discontinued due to serious adverse effects. How Are Hallucinogens Abused? The very same characteristics that led to the incorporation of hallucinogens into ritualistic or spiritual traditions have also led to their propagation as drugs of abuse. -

Substance Abuse: the Pharmacy Educator’S Role in Prevention and Recovery
Substance Abuse: The Pharmacy Educator’s Role in Prevention and Recovery Curricular Guidelines for Pharmacy: Substance Abuse and Addictive Disease i Curricular Guidelines for Pharmacy: Substance Abuse and Addictive Disease1,2 BACKGROUND OF THE CURRICULUM DEVELOPMENT PROJECT In 1988, the AACP Special Interest Group (SIG) on Pharmacy Student and Faculty Impairment (renamed Substance Abuse Education and Assistance) undertook the development of curricular guidelines for colleges/schools of pharmacy to facilitate the growth of educational opportunities for student pharmacists. These Curricular Guidelines for Pharmacy Education: Substance Abuse and Addictive Disease were published in 1991 (AJPE. 55:311-16. Winter 1991.) One of the charges of the Special Committee on Substance Abuse and Pharmacy Education was to review and revise the 1991 curricular guidelines. Overall, the didactic and experiential components in the suggested curriculum should prepare the student pharmacist to competently problem-solve issues concerning alcohol and other drug abuse and addictive diseases affecting patients, families, colleagues, themselves, and society. The guidelines provide ten educational goals, while describing four major content areas including: psychosocial aspects of alcohol and other drug use; pharmacology and toxicology of abused substances; identification, intervention, and treatment of people with addictive diseases; and legal/ethical issues. The required curriculum suggested by these guidelines addresses the 1 These guidelines were revised by the AACP Special Committee on Substance Abuse and Pharmacy Education. Members drafting the revised guidelines were Edward M. DeSimone (Creighton University), Julie C. Kissack (Harding University), David M. Scott (North Dakota State University), and Brandon J. Patterson (University of Iowa). Other Committee members were Paul W. Jungnickel, Chair (Auburn University), Lisa A. -

Minimum Laboratory Monitoring for Psychotropic Medications
Minimum Laboratory Monitoring For Psychotropic Medications ANTIPSYCHOTIC MEDICATIONS GENERIC BRAND GENERIC BRAND Aripiprazole Abilify, Abilify Olanzapine Zyprexa, Zyprexa Zydis Maintena, Aristada Asenapine Saphris Paliperidone Invega, Invega Sustenna, Invega Trinza Brexpiprazole Rexulti Perphenazine Trilafon Cariprazine Vraylar Pimozide Orap Chlorpromazine Thorazine Quetiapine Seroquel, Seroquel XR Clozapine Clozaril, Fazaclo Risperidone Risperdal, Risperdal Consta, Risperdal M Tabs Fluphenazine, Fluphenazine D Prolixin, Prolixin D Thioridazine Mellaril Haloperidol, Haloperidol D Haldol, Haldol D Thiothixene Navane Iloperidone Fanapt Trifluoperazine Stelazine Loxapine Loxitane Ziprasidone Geodon Lurasidone Latuda MONITORING ANTIPSYCHOTIC FREQUENCY OF MONITORING AIMS (Abnormal Involuntary Movement Scale) On initiation of any antipsychotic medication and at least every six months thereafter, or more frequently as clinically indicated. ABDOMINAL GIRTH (>18 years old) For individuals at least 18 years old, on initiation of any medication and at least every six months thereafter, or more frequently as clinically indicated. WEIGHT & BODY MASS INDEX (BMI) On initiation of any medication and at least every six months thereafter, or more frequently as clinically indicated. HEART RATE & BLOOD PRESSSURE On initiation of any medication and at least every six months thereafter, or more frequently as clinically indicated. COMPREHENSIVE METABOLIC PANEL (CMP), On initiation of any medication affecting this parameter and at least annually LIPIDS, FASTING -

Lurasidone in Combination with Lithium Or Valproate for the Maintenance Treatment of Bipolar I Disorder$
European Neuropsychopharmacology (]]]]) ], ]]]–]]] www.elsevier.com/locate/euroneuro Lurasidone in combination with lithium or valproate for the maintenance treatment of bipolar I disorder$ Joseph R. Calabresea, Andrei Pikalovb,c, Caroline Streicherb,c, Josephine Cucchiarob,c, Yongcai Maob,c, Antony Loebelb,c,n aUniversity Hospitals Case Medical Center, Case Western Reserve University, Cleveland, United States bSunovion Pharmaceuticals Inc., Marlborough, MA, United States cSunovion Pharmaceuticals Inc., Fort Lee, NJ, United States Received 15 November 2016; received in revised form 7 June 2017; accepted 20 June 2017 KEYWORDS Abstract Bipolar disorder; Lurasidone (DS-RAn) has demonstrated efficacy in the acute treatment of bipolar depression, Recurrence; both as monotherapy, and as combination therapy with lithium or valproate. To evaluate the Atypical antipsycho- recurrence prevention efficacy of lurasidone for the maintenance treatment of bipolar I tic; disorder, patients received up to 20 weeks of open-label lurasidone (20–80 mg/d) combined Lurasidone with lithium or valproate during an initial stabilization phase. A total of 496 patients met stabilization criteria and were randomized to 28 weeks of double-blind treatment with lurasidone (20–80 mg/d) or placebo, in combination with lithium or valproate. Based on a Cox proportional hazard model, treatment with lurasidone reduced the probability of recurrence of any mood episode by 29% (primary endpoint), however, the reduction did not achieve statistical significance. Probability of recurrence on lurasidone was significantly lower in patients with an index episode of depression (HR, 0.57; P=0.039), in patients with any index episode who were not rapid-cycling (HR, 0.69; P=0.046), and when recurrence was based on MADRS, YMRS, or CGI-BP-S severity criteria (HR, 0.53; P=0.025; sensitivity analysis). -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Programme & Abstracts
The 57th Annual Meeting of the International Association of Forensic Toxicologists. 2nd - 6th September 2019 BIRMINGHAM, UK The ICC Birmingham Broad Street, Birmingham B1 2EA Programme & Abstracts 1 Thank You to our Sponsors PlatinUm Gold Silver Bronze 2 3 Contents Welcome message 5 Committees 6 General information 7 iCC maps 8 exhibitors list 10 Exhibition Hall 11 Social Programme 14 opening Ceremony 15 Schedule 16 Oral Programme MONDAY 2 September 19 TUESDAY 3 September 21 THURSDAY 5 September 28 FRIDAY 6 September 35 vendor Seminars 42 Posters 46 oral abstracts 82 Poster abstracts 178 4 Welcome Message It is our great pleasure to welcome you to TIAFT Gala Dinner at the ICC on Friday evening. On the accompanying pages you will see a strong the UK for the 57th Annual Meeting of scientific agenda relevant to modern toxicology and we The International Association of Forensic thank all those who submitted an abstract and the Toxicologists Scientific Committees for making the scientific programme (TIAFT) between 2nd and 6th a success. Starting with a large Young Scientists September 2019. Symposium and Dr Yoo Memorial plenary lecture by Prof Tony Moffat on Monday, there are oral session topics in It has been decades since the Annual Meeting has taken Clinical & Post-Mortem Toxicology on Tuesday, place in the country where TIAFT was founded over 50 years Human Behaviour Toxicology & Drug-Facilitated Crime on ago. The meeting is supported by LTG (London Toxicology Thursday and Toxicology in Sport, New Innovations and Group) and the UKIAFT (UK & Ireland Association of Novel Research & Employment/Occupational Toxicology Forensic Toxicologists) and we thank all our exhibitors and on Friday. -

From Sacred Plants to Psychotherapy
From Sacred Plants to Psychotherapy: The History and Re-Emergence of Psychedelics in Medicine By Dr. Ben Sessa ‘The rejection of any source of evidence is always treason to that ultimate rationalism which urges forward science and philosophy alike’ - Alfred North Whitehead Introduction: What exactly is it that fascinates people about the psychedelic drugs? And how can we best define them? 1. Most psychiatrists will define psychedelics as those drugs that cause an acute confusional state. They bring about profound alterations in consciousness and may induce perceptual distortions as part of an organic psychosis. 2. Another definition for these substances may come from the cross-cultural dimension. In this context psychedelic drugs may be recognised as ceremonial religious tools, used by some non-Western cultures in order to communicate with the spiritual world. 3. For many lay people the psychedelic drugs are little more than illegal and dangerous drugs of abuse – addictive compounds, not to be distinguished from cocaine and heroin, which are only understood to be destructive - the cause of an individual, if not society’s, destruction. 4. But two final definitions for psychedelic drugs – and those that I would like the reader to have considered by the end of this article – is that the class of drugs defined as psychedelic, can be: a) Useful and safe medical treatments. Tools that as adjuncts to psychotherapy can be used to alleviate the symptoms and course of many mental illnesses, and 1 b) Vital research tools with which to better our understanding of the brain and the nature of consciousness. Classifying psychedelic drugs: 1,2 The drugs that are often described as the ‘classical’ psychedelics include LSD-25 (Lysergic Diethylamide), Mescaline (3,4,5- trimethoxyphenylathylamine), Psilocybin (4-hydroxy-N,N-dimethyltryptamine) and DMT (dimethyltryptamine). -

Psilocybin Mushrooms Fact Sheet
Psilocybin Mushrooms Fact Sheet January 2017 What are psilocybin, or “magic,” mushrooms? For the next two decades thousands of doses of psilocybin were administered in clinical experiments. Psilocybin is the main ingredient found in several types Psychiatrists, scientists and mental health of psychoactive mushrooms, making it perhaps the professionals considered psychedelics like psilocybin i best-known naturally-occurring psychedelic drug. to be promising treatments as an aid to therapy for a Although psilocybin is considered active at doses broad range of psychiatric diagnoses, including around 3-4 mg, a common dose used in clinical alcoholism, schizophrenia, autism spectrum disorders, ii,iii,iv research settings ranges from 14-30 mg. Its obsessive-compulsive disorder, and depression.xiii effects on the brain are attributed to its active Many more people were also introduced to psilocybin metabolite, psilocin. Psilocybin is most commonly mushrooms and other psychedelics as part of various found in wild or homegrown mushrooms and sold religious or spiritual practices, for mental and either fresh or dried. The most popular species of emotional exploration, or to enhance wellness and psilocybin mushrooms is Psilocybe cubensis, which is creativity.xiv usually taken orally either by eating dried caps and stems or steeped in hot water and drunk as a tea, with Despite this long history and ongoing research into its v a common dose around 1-2.5 grams. therapeutic and medical benefits,xv since 1970 psilocybin and psilocin have been listed in Schedule I of the Controlled Substances Act, the most heavily Scientists and mental health professionals criminalized category for drugs considered to have a consider psychedelics like psilocybin to be “high potential for abuse” and no currently accepted promising treatments as an aid to therapy for a medical use – though when it comes to psilocybin broad range of psychiatric diagnoses. -
Lithium Sulfate
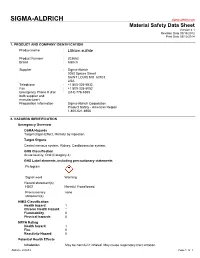
SIGMA-ALDRICH sigma-aldrich.com Material Safety Data Sheet Version 4.1 Revision Date 09/14/2012 Print Date 03/12/2014 1. PRODUCT AND COMPANY IDENTIFICATION Product name : Lithium sulfate Product Number : 203653 Brand : Aldrich Supplier : Sigma-Aldrich 3050 Spruce Street SAINT LOUIS MO 63103 USA Telephone : +1 800-325-5832 Fax : +1 800-325-5052 Emergency Phone # (For : (314) 776-6555 both supplier and manufacturer) Preparation Information : Sigma-Aldrich Corporation Product Safety - Americas Region 1-800-521-8956 2. HAZARDS IDENTIFICATION Emergency Overview OSHA Hazards Target Organ Effect, Harmful by ingestion. Target Organs Central nervous system, Kidney, Cardiovascular system. GHS Classification Acute toxicity, Oral (Category 4) GHS Label elements, including precautionary statements Pictogram Signal word Warning Hazard statement(s) H302 Harmful if swallowed. Precautionary none statement(s) HMIS Classification Health hazard: 1 Chronic Health Hazard: * Flammability: 0 Physical hazards: 0 NFPA Rating Health hazard: 1 Fire: 0 Reactivity Hazard: 0 Potential Health Effects Inhalation May be harmful if inhaled. May cause respiratory tract irritation. Aldrich - 203653 Page 1 of 7 Skin Harmful if absorbed through skin. May cause skin irritation. Eyes May cause eye irritation. Ingestion Harmful if swallowed. 3. COMPOSITION/INFORMATION ON INGREDIENTS Formula : Li2O4S Molecular Weight : 109.94 g/mol Component Concentration Lithium sulphate CAS-No. 10377-48-7 - EC-No. 233-820-4 4. FIRST AID MEASURES General advice Move out of dangerous area.Consult a physician. Show this safety data sheet to the doctor in attendance. If inhaled If breathed in, move person into fresh air. If not breathing, give artificial respiration. Consult a physician. -

Guidance on the Use of Mood Stabilizers for the Treatment of Bipolar Affective Disorder Version 2
Guidance on the use of mood stabilizers for the treatment of bipolar affective disorder Version 2 RATIFYING COMMITTEE DRUGS AND THERAPEUTICS GROUP DATE RATIFIED July 2015 REPLACES Version 1 dated July 2013 NEXT REVIEW DATE July 2017 POLICY AUTHORS Jules Haste, Lead Pharmacist, Brighton and Hove Members of the Pharmacy Team (contributors are listed overleaf) If you require this document in an alternative format, i.e. easy read, large text, audio or Braille please contact the pharmacy team on 01243 623349 Page 1 of 49 Contributors Jed Hewitt, Chief Pharmacist - Governance & Professional Practice James Atkinson, Pharmacist Team Leader Mental Health and Community Services Miguel Gomez, Lead Pharmacist, Worthing. Hilary Garforth, Lead Pharmacist, Chichester. Pauline Daw, Lead Pharmacist (CRHTs & AOT), East Sussex. Iftekhar Khan, Lead Pharmacist (S&F Service), East Sussex. Graham Brown, Lead Pharmacist CAMHS & EIS. Gus Fernandez, Specialist Pharmacist MI and MH Lisa Stanton, Specialist Pharmacist Early Intervention Services & Learning Disabilities. Nana Tomova, Specialist Pharmacist, Crawley. Page 2 of 49 Section Title Page Number Introduction and Key Points 4 1. General principles in the treatment of acute mania 6 2. General principles in the treatment of bipolar depression 8 3. General principles in long term treatment 10 4. Rapid cycling 13 5. Physical health 13 6. Treatment in special situations 6.1 Pregnancy 15 6.2 Breast-feeding 17 6.3 Older adults 19 6.4 Children and adolescents 22 6.5 Learning disabilities 29 6.6 Cardiac dysfunction 30 6.7 Renal dysfunction 34 6.8 Hepatic dysfunction 37 6.9 Epilepsy 41 7. The risk of switching to mania with antidepressants 43 8. -

Microgram Journal, Vol 2, Number 1
Washington, D. C. Office of Science and Education Vol.II,No.1 Division of Laboratory Operations January 1969 INDEXISSUE CORRECTION 11 "Structure Elucidation of 'LBJ' , by Sander W. Bellman, John W. Turczan, James Heagy and Ted M. Hopes, Micro Gram .!., 3, 6-13 (Dec. 1968) Page 7, third and fourth sentences under Discussion: Change to read: "The melting point of the acid moiety found in step (g) was 148-150°c., compared to the litera ture, v~lue of 151°c for the melting point of benzilic acid (2); thus the benzilic acid melting point gives support to the proposed structure for 'LBJ'. Spectral evidence also supports the proposed structure". MICRO-GRAMREVISION Please re-number the pages of your copies of Micro-Gram, Volume I. Re-number pages bearing printing only. Vol ume I will then be numbered from page 1, the front page of issue No. 1, through page 189 the last page of issue No. 12. To help with this task, pages contained within each issue are as follows: Issue Number Page Through 1 1 8 2 9 29 3 30 32 4 33 66 5 67 79 6 80 97 7 98 120 8 121 128 9 129 136 10 137 157 11 158 170 12 171 189 CAUTION: Use of this publication should be restricted to forensic analysts or others having a legitimate need for this material. From the Archive Library of Erowid Center http://erowid.org/library/periodicals/microgram -2- CANNABIS ,·,-...__/' Attached is a copy of 11A Short Rapid Method for the Identification of Cannabis." The method was developed by Mro H.D.