The Biomechanical Effects of Rotator Cuff Taping on Muscle Activity and Throwing Velocity in Fatigued Baseball Players
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MEDIA and LITERARY REPRESENTATIONS of LATINOS in BASEBALL and BASEBALL FICTION by MIHIR D. PAREKH Presented to the Faculty of T
MEDIA AND LITERARY REPRESENTATIONS OF LATINOS IN BASEBALL AND BASEBALL FICTION by MIHIR D. PAREKH Presented to the Faculty of the Graduate School of The University of Texas at Arlington in Partial Fulfillment of the Requirements for the Degree of MASTER OF ARTS IN ENGLISH THE UNIVERSITY OF TEXAS AT ARLINGTON May 2015 Copyright © by Mihir Parekh 2015 All Rights Reserved ii Acknowledgements I would like to express my thanks to my supervisor, Dr. William Arcé, whose knowledge and expertise in Latino studies were vital to this project. I would also like to thank the other members of my committee, Dr. Timothy Morris and Dr. James Warren, for the assistance they provided at all levels of this undertaking. Their wealth of knowledge in the realm of sport literature was invaluable. To my family: the gratitude I have for what you all have provided me cannot be expressed on this page alone. Without your love, encouragement, and support, I would not be where I am today. Thank you for all you have sacrificed for me. April 22, 2015 iii Abstract MEDIA AND LITERARY REPRESENTATIONS OF LATINOS IN BASEBALL AND BASEBALL FICTION Mihir D. Parekh, MA The University of Texas at Arlington, 2015 Supervising Professors: William Arcé, Timothy Morris, James Warren The first chapter of this project looks at media representations of two Mexican- born baseball players—Fernando Valenzuela and Teodoro “Teddy” Higuera—pitchers who made their big league debuts in the 1980s and garnered significant attention due to their stellar play and ethnic backgrounds. Chapter one looks at U.S. media narratives of these Mexican baseball players and their focus on these foreign athletes’ bodies when presenting them the American public, arguing that 1980s U.S. -

Maximising Ball Release Speed in Overhead Throwing Through Optimising Arm Segment Masses
MAXIMISING BALL RELEASE SPEED IN OVERHEAD THROWING THROUGH OPTIMISING ARM SEGMENT MASSES A thesis submitted for the degree of Doctor of Philosophy by Patrick Fasbender Department of Life Sciences, Brunel University London 28 September 2017 Abstract The tapering distribution of segment masses in the human arm helps in the generation of high ball release speeds in overarm throwing. However, the masses of the individual arm segments might not be optimal; arm segment masses could be optimised in order to improve throwing performance. The aim of this project was to identify and understand the optimal upper arm mass that results in the highest ball release speed in overarm throwing. The first study was a theoretical study, using a simple two-segment model of the arm to determine the optimal combination of arm segment masses that maximises ball release speed. This simplified throw was chosen to identify the basic mechanism causing changes in ball release speed with a heavier upper arm mass. The study identified that there is an optimal upper arm mass, but this optimum depends on the forearm mass and the shoulder torque. Furthermore, the study showed that a heavier forearm mass produces a lower ball release speed. An experimental approach was used in the second study to analyse the effect of additional upper arm mass on ball release speed and throwing mechanics in an overarm throw similar to that used by baseball pitchers. However, group analysis of the ball release speed did not reveal an optimal upper arm mass, and most of the kinematic, kinetic, and temporal variables were not affected by additional upper arm mass. -
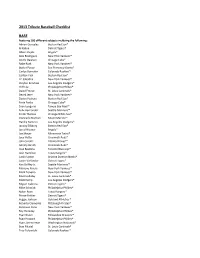
2013 Tribute Baseball Checklist BASE
2013 Tribute Baseball Checklist BASE Featurng 100 different subjects inclduing the following: Adrian Gonzalez Boston Red Sox® Al Kaline Detroit Tigers® Albert Pujols Angels® Alex Rodriguez New York Yankees® Andre Dawson Chicago Cubs® Babe Ruth New York Yankees® Buster Posey San Francisco Giants® Carlos Gonzalez Colorado Rockies™ Carlton Fisk Boston Red Sox® CC Sabathia New York Yankees® Clayton Kershaw Los Angeles Dodgers® Cliff Lee Philadelphia Phillies® David Freese St. Louis Cardinals® Derek Jeter New York Yankees® Dustin Pedroia Boston Red Sox® Ernie Banks Chicago Cubs® Evan Longoria Tampa Bay Rays™ Felix Hernandez Seattle Mariners™ Frank Thomas Chicago White Sox® Giancarlo Stanton Miami Marlins™ Hanley Ramirez Los Angeles Dodgers® Jacoby Ellsbury Boston Red Sox® Jered Weaver Angels® Joe Mauer Minnesota Twins® Joey Votto Cincinnati Reds® John Smoltz Atlanta Braves™ Johnny Bench Cincinnati Reds® Jose Bautista Toronto Blue Jays® Josh Hamilton Texas Rangers® Justin Upton Arizona Diamondbacks® Justin Verlander Detroit Tigers® Ken Griffey Jr. Seattle Mariners™ Mariano Rivera New York Yankees® Mark Teixeira New York Yankees® Matt Holliday St. Louis Cardinals® Matt Kemp Los Angeles Dodgers® Miguel Cabrera Detroit Tigers® Mike Schmidt Philadelphia Phillies® Nolan Ryan Texas Rangers® Prince Fielder Detroit Tigers® Reggie Jackson Oakland Athletics™ Roberto Clemente Pittsburgh Pirates® Robinson Cano New York Yankees® Roy Halladay Philadelphia Phillies® Ryan Braun Milwaukee Brewers™ Ryan Howard Philadelphia Phillies® Ryan Zimmerman Washington Nationals® Stan Musial St. Louis Cardinals® Troy Tulowitzki Colorado Rockies™ Willie Mays San Francisco Giants® AUTOGRAPHS On-Card Autographs At least 150 different cards including the following: Adam Jones Baltimore Orioles® Adrian Gonzalez Boston Red Sox® Albert Pujols Angels® Albert Belle Cleveland Indians® Andre Dawson Chicago Cubs® Andy Pettitte New York Yankees® Bob Gibson St. -

Great Outing, Even Greater People in Sandy
Whether pitching in Wrigley Field or Dodger Stadium, Sandy Koufax almost always got a fight from the Cubs. (Photos courtesy of the Leo Bauby Collection). Great outing, even greater people in Sandy Koufax perfecto against Chicago Cubs By George Castle, CBM Historian Posted Thursday, September 3, 2015 (Second of a two-part series on the 50th anniversary of Sandy Koufax’s perfect game against the Cubs on Sept. 9, 1965 in what may have been the greatest pitching duel in history with Chicago lefty Bob Hendley.) On the surface, the Sandy Koufax perfect game is part of baseball mythology, Koufax’s fastball growing ever faster over the decades, the Cubs’ swings even more futile, the lone run scored even more fluky, the only hit in the game even more shaky. Oral history is the main conduit of its memories, and you know how baseball stories get exaggerated as time progresses. It might as well have taken place in the 19th Century, given how 15 years into the TV era — and with the dramatic expansion of network color telecasts beginning the next week — only three innings of halting home-movie film ex- ists (see accompanying story below). Three network-owned stations and four other inde- pendent VHF stations in Los Angeles, all with regular newscasts, declined to film the game despite the Dodgers’ position in the pennant race. The radio broadcast recordings were cobbled together. www.ChicagoBaseballMuseum.org [email protected] Statistically, the game was the greatest pitching duel Editor's note: in history. Koufax and Hendley took no-hitters into the seventh inning. -

Candle Lighting Time Is 7:50 Sabbath Services Start at 9:30
Candle lighting time is 7:50 Sabbath services start at 9:30 What do Danny Kravitz, Hank Greenberg, John Grabow, and Ike Davis have in common? They are all Jews who played for the Pirates There is a long standing stereotype that says that Jews can’t play sports, that they have brains, but no brawn. In 1907, Harvard president Charles Elliot said, “Jews are definitely inferior in stature and physical development.” A 1998 New York Times article referred to, “that reputedly rare species – the Jewish athlete.” Well, last week I was watching the Bucs play the Tigers at PNC Park, and there, on the Tigers bench, sat Manager Brad Ausmus, a Jew, and out at second base was an All Star by the name of Ian Kinsler, another Jew. And one of the greatest sluggers of all time, a former Tiger, and later in his career a Pittsburgh Pirate, Hank Greenberg, was also a Jew. Current Jewish players in MLB also include Ryan Braun of the Brewers, Ike Davis of the A’s, Scott Feldman of the Astros, Jason Marquis of the Reds, Craig Breslow of the Red Sox, Jason Kipnis of the Indians, Danny Valencia of the Blue Jays, Sam Fuld of the A’s, Ryan Lavarnway of the Orioles, and Joc Pederson of the Dodgers. So who were the best Jewish players ever? Let’s start with Sandy Koufax, perhaps the best left handed pitcher of all time. How good was Koufax? Well, the fans who voted in Baseball’s balloting for the All Century Team picked Koufax as the top lefthander of the century, trailing only Nolan Ryan in the overall voting for pitchers. -

Determinants of Major League Baseball Player Salaries
Syracuse University SURFACE Syracuse University Honors Program Capstone Syracuse University Honors Program Capstone Projects Projects Spring 5-1-2013 Determinants of Major League Baseball Player Salaries Tyler Wasserman Syracuse University Follow this and additional works at: https://surface.syr.edu/honors_capstone Part of the Sports Management Commons Recommended Citation Wasserman, Tyler, "Determinants of Major League Baseball Player Salaries" (2013). Syracuse University Honors Program Capstone Projects. 99. https://surface.syr.edu/honors_capstone/99 This Honors Capstone Project is brought to you for free and open access by the Syracuse University Honors Program Capstone Projects at SURFACE. It has been accepted for inclusion in Syracuse University Honors Program Capstone Projects by an authorized administrator of SURFACE. For more information, please contact [email protected]. Determinants of Major League Baseball Player Salaries A Capstone Project Submitted in Partial Fulfillment of the Requirements of the Renée Crown University Honors Program at Syracuse University Tyler Wasserman Candidate for Bachelor of Science Degree and Renée Crown University Honors December 2013 Honors Capstone in Sport Management Capstone Project Advisor: ______________________________ Rodney Paul, Professor Capstone Project Reader: ______________________________ Michael Veley, Director & Chair Honors Director: ______________________________ Stephen Kuusisto, Director Date: March 6, 2014 © Tyler Wasserman, March 6, 2014 Abstract In 2003, Michael Lewis published Moneyball: The Art of Winning an Unfair Game , which forever changed the finances and economics of baseball. It began a movement towards using advanced statistical analysis to determine the value of baseball players, in order to build a roster that will win the most games at the lowest cost. The Moneyball movement has resulted in a multitude of new statistics to try to drill a player’s value down to one number that represents his marginal revenue product, or his individual contribution to the team’s success. -

The Matthews Sports Exhibit Offers Visitors the Opportunity✡ to Enjoy
Jewish Community Center of Metropolitan Detroit Jews and Baseball – An American Love Story Provides a Dynamic Aspect ✡ ✡ ✡ ✡ ✡ ✡ THE MATTHEWS to the Exhibit ✡ ✡ ✡ ✡ H ✡ TT EW ✡ A In addition to the autographs, photos, helmets, shoes, bats and books, ✡ S ✡ SPORTS EXHIBIT M ✡ the Matthews Sports Exhibit offers visitors the opportunity✡ to enjoy ✡ the award-winning documentary “Jews and Baseball✡ – An American ✡ S Love Story.” ✡ ✡ ✡ p i ✡ JewishJewish HeroesHeroes The film, which plays throughout the exhibit, was narrated✡ by actor o ✡ b ✡ Dustin Hoffman and written by Pulitzer Prize-winning sports columnist ✡ r i ✡ ✡ t ✡ h ✡ ✡ x ✡ E ✡ Ira Berkow. “Jews and Baseball – An American Love Story” provides✡ && OtherOther LegendsLegends a compelling look at the history of Jews and the sport, including an interview with Hall of Fame pitcher Sandy Koufax, who rarely appears in public. It also features Al Rosen, Kevin Youkilis, Shawn Green, Norm Featuring rare and unforgettable autographs, Sherry, Ron Blomberg and such stars as Yogi Berra and Bob Feller in photos, memorabilia and more, interviews and stories that bring the incredible Matthews Collection to life. plus the award-winning documentary “A fascinating and moving film.” ~The Jerusalem Post “A warm and enthusiastic documentary.” ~ The Los Angeles Times Jews and Baseball – An American Love Story “An insightful, moving film that helps to shatter stereotypes and preconceptions, and reminds us of the power of this seemingly simple stickball game to bring us all together.” ~ Ken Burns, Emmy Award- winning filmmaker of “The Civil War,” “Baseball” and “Jazz” The Jewish Community Center of Metropolitan Detroit A DVD of Jews and Baseball – An American Love Story may be ordered at jewsandbaseball.com. -

Baseball Under Glass
Ryno, Rossy going in opposite directions on managing By George Castle, CBM Historian Posted Monday, January 30, 2017 Symbolically, they looked like the ships passing in the night. Or passing off the ba- ton. Whatever old phrase you want to em- ploy. Ryne Sandberg and David Ross sat at op- posite ends of their threesome with Kyle Schwarber on stage in the middle at a charity event in downstate Urbana over the weekend. They definitely were going in different directions. Ryno is easing up on life now. Hard- charging a decade ago into a hoped-for Ryne Sandberg (from left), Kyle Schwarber and eventual big-league managerial career – David Ross entertained a packed house of 400 in Urbana recently. preferably with the Cubs – Hall of Famer Sandberg seems content now to work as a Cubs ambassador, the franchise's big-name former player making appearances around his new year-round home in Chicago. Meanwhile, Ross is the hottest commodity in baseball – literally. Reportedly getting as much as $30,000 for a personal appearance, Grandpa Rossy just added an ESPN base- ball analyst gig to his portfolio, only weeks after chief patron Theo Epstein hired him as a Cubs special assistant. Who’d ever think a backup catcher would be carried off the field by his teammates after Game 7 of the World Series? But that’s the impression Ross made with both Cubs players and fans in his final two years in the majors. He fin- ished well, to be sure. In reality, Ross is just starting a manager’s training program. -

World Series Reflections 2013
What They Said – And What They Didn’t Say Rabbi Carl M. Perkins November 2, 2013 Temple Aliyah Needham, MA Right now, as we are sitting here in shul, thousands of Bostonians are celebrating the victory of the Boston Red Sox in the World Series. As our Torah service began, just as we “pray-ers” began to sing “Vayehi bin’soa ha-aron,” the “play-ers’” parade began on Boston Common. By now, the players have undoubtedly already entered the Charles River on their duck boats. I can’t wait to get the details on the news tonight after Shabbat is over. That last game, on Wednesday night, was a wonderful capstone to a great series, which itself was a wonderful conclusion to a terrific season. (I wouldn’t have minded it if the games had begun an hour earlier each evening, but I’d rather a late World Series game in which the Red Sox are playing than an early one in which they’re not.) I have a few words to say today about the Red Sox. I think there are some lessons we can learn from them, and take to heart. Before doing so, let me just pause to reflect on the phenomenon of speaking about a baseball team in shul. I don’t do that very often. In fact, I’ve never done it. Baseball is, of course, a sport, and while we may value sports and admire great athletes, the question can certainly be asked: What’s Jewish about it? What’s Jewish about athletic competition? What’s Jewish about the World Series? I remember the World Series of 1965, which pitted the Los Angeles Dodgers against the Minnesota Twins. -

Road Scholar Spring Training Adventures Offer a Behind-The-Scenes Look at America's Favorite Pastime BOSTON (February 27
FOR IMMEDIATE RELEASE Contact: Stacie Fasola (617) 457-5418 Despina Gakopoulos (617) 457-5502 [email protected] Road Scholar Spring Training Adventures Offer a Behind-the-Scenes Look at America’s Favorite Pastime BOSTON (February 27, 2013) – Baseball has a special place in the hearts of Americans. For those who just can’t wait for Opening Day, Road Scholar offers baseball learning adventures throughout March for an insider’s look at spring training in Florida and Arizona. As teams file into their spring homes to begin preparation for the regular season, fans of the game can follow them and choose Florida’s Grapefruit League, spanning Fort Myers, Deland, Sarasota and St. Petersburg, or the Cactus League, centered in the Phoenix Valley of the Sun, to experience a five-night adventure that offers opportunities to hear from baseball experts, professional players, coaches, historians and more. Highlights include exploring baseball’s controversies, the rules of the game, how the game impacts American culture and watching your favorite team play at its spring home. Grapefruit League Spring Training: Baseball with the Boston Red Sox and Minnesota Twins Experience and explore America’s pastime and the rich legacy of the Boston Red Sox and Minnesota Twins in sunny Fort Myers, Florida. These rebuilding American League franchises have totaled four World Series championships in the last 24 years. Explore Red Sox history — Ted Williams, Carlton Fisk’s 1975 home run and the 2004 miracle title that ended the 86-year Curse of the Bambino. Revisit the Twins’1960 move to the Twin Cities, Kent Hrbek’s 1987 World Series grand slam and the arrival of $25 million man Joe Mauer. -

2013 Select Baseball Autograph Team Checklist
2013 Select Baseball Autograph Team Checklist Player Set Card # Team Print Run Troy Glaus Signatures + Parallels 80 Angels ?? + 36 Tim Salmon Signatures + Parallels 88 Angels ?? + 36 Andrew Taylor Rookies Autographs + Parallels 185 Angels 875 Nick Maronde Rookies Autographs + Parallels 214 Angels 875 Mark Trumbo Signatures + Parallels 64 Angels ?? + 36 Brandon Barnes Rookies Autographs + Parallels 188 Astros 875 L.J. Hoes Rookies Autographs + Parallels 235 Astros 625 Craig Biggio Signatures + Parallels 22 Astros ?? + 36 Jeff Bagwell Signatures + Parallels 94 Astros ?? + 36 Andrew Werner Rookies Autographs + Parallels 186 Athletics 875 Sonny Gray Rookies Autographs + Parallels 245 Athletics 875 Jarrod Parker Signatures + Parallels 43 Athletics ?? + 36 Josh Reddick Signatures + Parallels 55 Athletics ?? + 36 Rickey Henderson Signatures + Parallels 79 Athletics ?? + 16 Yoenis Cespedes Signatures + Parallels 23 Athletics ?? + 36 Aaron Loup Rookies Autographs + Parallels 178 Blue Jays 875 Chad Jenkins Rookies Autographs + Parallels 198 Blue Jays 875 Tyson Brummett Rookies Autographs + Parallels 218 Blue Jays 875 Colby Rasmus Signatures + Parallels 20 Blue Jays ?? + 36 Edwin Encarnacion Signatures + Parallels 35 Blue Jays ?? + 36 Jose Bautista Signatures + Parallels 53 Blue Jays ?? + 36 Josh Johnson Signatures + Parallels 54 Blue Jays ?? + 36 R.A. Dickey Signatures + Parallels 78 Blue Jays ?? + 36 Evan Gattis Rookies Autographs + Parallels 209 Braves 875 Alex Wood Signatures + Parallels 97 Braves ?? + 36 Chipper Jones Signatures + Parallels -

Cubs Try Hard Enough Vs. Koufax to Make Him Pitch a Game and a Half Twice
Cubs try hard enough vs. Koufax to make him pitch a game and a half twice By George Castle, CBM Historian Posted Friday, October 25th, 2013 Beat Koufax! The Cubs may not have won many games overall, or of- ten defeated a certain Los Angeles Dodgers left-hander who pitched “above” big-league level. But no matter what quality of his other-worldly stuff that day, Sandy Koufax often had to pitch for his life against the second- division Cubs of his era. And in two instances, “Dandy Sandy,” as some of the scribes of the time called him, Koufax had to go the equivalent of double-overtime to even get a decision, win or lose, against the Cubs. The barbaric handling of Koufax in these pair of games by Dodgers manager Walter Alston might have contributed to finger and el- bow problems that afflicted Koufax in the last five sea- sons of his Hall of Fame, but abbreviated, career. Koufax hurled games for the ages against the Cubs. On Sept. 9, 1965, he notched a perfect game – the last of his four no-hitters – against the Chicago visitors at Dodger Stadium. Koufax struck out the final six Cubs to bring his game total to 14. That game started a prodi- gious streak – the Cubs have gone the longest of any present team without being no-hit. They’ve been no-hit into the ninth twice, by Tom Seaver in 1969 and 1975, and by Alex Fernandez in 1997. Somehow, they’ve come up with a well-timed single to keep the post-Koufax perfecto skein intact.