Cellular, Molecular Consequences of Peroxisome Proliferator- Activated
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Aryl Hydrocarbon Receptor: Structural Analysis and Activation Mechanisms
The Aryl Hydrocarbon Receptor: Structural Analysis and Activation Mechanisms This thesis is submitted in fulfilment of the requirements for the degree of Doctor of Philosophy in the School of Molecular and Biomedical Sciences (Biochemistry), The University of Adelaide, Australia Fiona Whelan, B.Sc. (Hons) 2009 2 Table of Contents THESIS SUMMARY................................................................................. 6 DECLARATION....................................................................................... 7 PUBLICATIONS ARISING FROM THIS THESIS.................................... 8 ACKNOWLEDGEMENTS...................................................................... 10 ABBREVIATIONS ................................................................................. 12 CHAPTER 1: INTRODUCTION ............................................................. 17 1.1 BHLH.PAS PROTEINS ............................................................................................17 1.1.1 General background..................................................................................17 1.1.2 bHLH.PAS Class I Proteins.........................................................................18 1.2 THE ARYL HYDROCARBON RECEPTOR......................................................................19 1.2.1 Domain Structure and Ligand Activation ..............................................19 1.2.2 AhR Expression and Developmental Activity .......................................21 1.2.3 Mouse AhR Knockout Phenotype ...........................................................23 -
Non-Homologous Isofunctional Enzymes: a Systematic Analysis Of
Omelchenko et al. Biology Direct 2010, 5:31 http://www.biology-direct.com/content/5/1/31 RESEARCH Open Access Non-homologousResearch isofunctional enzymes: A systematic analysis of alternative solutions in enzyme evolution Marina V Omelchenko, Michael Y Galperin*, Yuri I Wolf and Eugene V Koonin Abstract Background: Evolutionarily unrelated proteins that catalyze the same biochemical reactions are often referred to as analogous - as opposed to homologous - enzymes. The existence of numerous alternative, non-homologous enzyme isoforms presents an interesting evolutionary problem; it also complicates genome-based reconstruction of the metabolic pathways in a variety of organisms. In 1998, a systematic search for analogous enzymes resulted in the identification of 105 Enzyme Commission (EC) numbers that included two or more proteins without detectable sequence similarity to each other, including 34 EC nodes where proteins were known (or predicted) to have distinct structural folds, indicating independent evolutionary origins. In the past 12 years, many putative non-homologous isofunctional enzymes were identified in newly sequenced genomes. In addition, efforts in structural genomics resulted in a vastly improved structural coverage of proteomes, providing for definitive assessment of (non)homologous relationships between proteins. Results: We report the results of a comprehensive search for non-homologous isofunctional enzymes (NISE) that yielded 185 EC nodes with two or more experimentally characterized - or predicted - structurally unrelated proteins. Of these NISE sets, only 74 were from the original 1998 list. Structural assignments of the NISE show over-representation of proteins with the TIM barrel fold and the nucleotide-binding Rossmann fold. From the functional perspective, the set of NISE is enriched in hydrolases, particularly carbohydrate hydrolases, and in enzymes involved in defense against oxidative stress. -

Engineering Zinc-Finger Protein and CRISPR/Cas9 Constructs to Model the Epigenetic and Transcriptional Phenomena That Underlie Cocaine-Related Behaviors
Engineering zinc-finger protein and CRISPR/Cas9 constructs to model the epigenetic and transcriptional phenomena that underlie cocaine-related behaviors Hamilton PJ, Heller EA, Ortiz Torres I, Burek DD, Lombroso SI, Pirpinias ST, Neve RL, Nestler EJ Multiple studies have implicated genome-wide epigenetic remodeling events in brain reward regions following drug exposure. However, only recently has it become possible to target a given type of epigenetic remodeling to a single gene of interest, in order to probe the causal relationship between such regulation and neuropsychiatric disease (Heller et al., Nat Neurosci, 2014). Our group has successfully utilized synthetic zinc- finger proteins (ZFPs), fused to either the transcriptional repressor, G9a, that promotes histone methylation or the transcriptional activator, p65, that promotes histone acetylation, to determine the behavioral effects of targeted in vivo epigenetic reprogramming in a locus-specific and cell-type specific manner. Given the success of our ZFP approaches, we have broadened our technical repertoire to include the more novel and flexible CRISPR/Cas9 technology. We designed guide RNAs to target nuclease-dead Cas9 (dCas9) fused to effector domains to the fosB gene locus, a locus heavily implicated in the pathogenesis of drug abuse. We observe that dCas9 fused to the transcriptional activator, VP64, or the transcriptional repressor, KRAB, and targeted to specific sites in the fosB promoter is sufficient to regulate FosB and ΔFosB mRNA levels, in both cultured cells and in the nucleus accumbens (NAc) of mice receiving viral delivery of CRISPR constructs. Next, we designed a fusion construct linking the dCas9 moiety to a pseudo-phosphorylated isoform of the transcription factor CREB (dCas9 CREB(S133D)). -

Biosynthesis in Vitro of Bacillamide Intermediate-Heterocyclic Alacysthiazole by Heterologous Expression of Nonribosomal Peptide Synthetase (NRPS) T
Journal of Biotechnology 292 (2019) 5–11 Contents lists available at ScienceDirect Journal of Biotechnology journal homepage: www.elsevier.com/locate/jbiotec Biosynthesis in vitro of bacillamide intermediate-heterocyclic AlaCysthiazole by heterologous expression of nonribosomal peptide synthetase (NRPS) T Fengli Zhang, Nayila Mulati, Yukun Wang, Yingxin Li, Sanqiang Gong, Loganathan Karthik, ⁎ Wei Sun, Zhiyong Li Marine Biotechnology Laboratory, State Key Laboratory of Microbial Metabolism and School of Life Sciences & Biotechnology, Shanghai Jiao Tong University, Shanghai, China ARTICLE INFO ABSTRACT Keywords: Bacillamide C, a potential natural antialgae active compound, is produced by Bacillus atrophaeus C89 derived Bacillus atrophaeus from marine sponge Dysidea avara. A nonribosomal peptide synthetase (NRPS) cluster is hypothesized to be Bacillamides involved in the biosynthesis of bacillamide C. The NRPS with a domain string of A1-PCP1-Cy-A2-PCP2-C can be Heterologous expression divided into three functional modules. After heterologous expression and purification of module A1-PCP1 and Nonribosomal peptide synthetase (NRPS) module Cy-A2-PCP2, their catalytic activities were biochemically proven in vitro by the reaction with the apo- Thiazole PCP domain transformed to the holo-PCP domain through a phosphopantetheinyl transferase, ATP, and substrate amino acids. Five– membered heterocyclic AlaCysthiazole with molecular weight of 172.0389 was detected. This proved the formation of the heterocyclic dipeptide AlaCysthiazole, which is considered to be a building block for the biosynthesis of bacillamide. This study provides a basis for further biosynthesis of bacillamides. 1. Introduction et al., 2017). Even though the biosynthesis of bacillamide C was opti- mized, the yield was very low (Jin et al., 2011; Yu et al., 2015). -

Comprehensive Genome-Wide Exploration of C2H2 Zinc Finger Family in Grapevine (Vitis Vinifera L.): Insights Into the Roles in the Pollen Development Regulation
G C A T T A C G G C A T genes Article Comprehensive Genome-Wide Exploration of C2H2 Zinc Finger Family in Grapevine (Vitis vinifera L.): Insights into the Roles in the Pollen Development Regulation Oscar Arrey-Salas 1,* , José Carlos Caris-Maldonado 2, Bairon Hernández-Rojas 3 and Enrique Gonzalez 1 1 Laboratorio de Genómica Funcional, Instituto de Ciencias Biológicas, Universidad de Talca, 3460000 Talca, Chile; [email protected] 2 Center for Research and Innovation (CRI), Viña Concha y Toro, Ruta k-650 km 10, 3550000 Pencahue, Chile; [email protected] 3 Ph.D Program in Sciences Mention in Modeling of Chemical and Biological Systems, Faculty of Engineering, University of Talca, Calle 1 Poniente, 1141, 3462227 Talca, Chile; [email protected] * Correspondence: [email protected] Abstract: Some C2H2 zinc-finger proteins (ZFP) transcription factors are involved in the development of pollen in plants. In grapevine (Vitis vinifera L.), it has been suggested that abnormalities in pollen development lead to the phenomenon called parthenocarpy that occurs in some varieties of this cultivar. At present, a network involving several transcription factors types has been revealed and key roles have been assigned to members of the C2H2 zinc-finger proteins (ZFP) family in model plants. However, particularities of the regulatory mechanisms controlling pollen formation in grapevine Citation: Arrey-Salas, O.; remain unknown. In order to gain insight into the participation of ZFPs in grapevine gametophyte Caris-Maldonado, J.C.; development, we performed a genome-wide identification and characterization of genes encoding Hernández-Rojas, B.; Gonzalez, E. ZFP (VviZFP family). -

A New C2H 2 Zinc Finger Protein and a C2C2 Steroid Receptor-Like Component
Downloaded from genesdev.cshlp.org on October 6, 2021 - Published by Cold Spring Harbor Laboratory Press Proteins that bind to Drosophila chorion cis-regulatory elements: A new C2H 2 zinc finger protein and a C2C2 steroid receptor-like component Martin J. Shea, 1 Dennis L. King, 1 Michael J. Conboy, 2 Brian D. Mariani, 3 and Fotis C. Kafatos 1,3 ~Department of Cellular and Developmental Biology, Harvard University Biological Laboratories, Cambridge, Massachusetts 02138 USA; ZJefferson Institute of Molecular Medicine, Thomas Jefferson University, Philadelphia, Pennsylvania 19107 USA; 3Institute of Molecular Biology and Biotechnology, Research Center of Crete, and Department of Biology, University of Crete, Heraklion 711 10, Crete, Greece Gel mobility-shift assays have been used to identify proteins that bind specifically to the promoter region of the Drosophila s15 chorion gene. These proteins are present in nuclear extracts of ovarian follicles, the tissue where s15 is expressed during development, and bind to specific elements of the promoter that have been shown by transformation analysis to be important for in vivo expression. The DNA binding specificity has been used for molecular cloning of two components from expression cDNA libraries and for their tentative identification with specific DNA-binding proteins of the nuclear extracts. The mRNAs for both of these components, CF1 and CF2, are differentially enriched in the follicles. DNA sequence analysis suggests that both CF1 and CF2 are novel Drosophila transcription factors. CF2 is a member of the C2H2 family of zinc finger proteins, whereas CF1 is a member of the family of steroid hormone receptors. The putative DNA-binding domain of CF1 is highly similar to the corresponding domains of certain vertebrate hormone receptors and recognizes a region of DNA with similar, hyphenated palindromic sequences. -

The Microbiota-Produced N-Formyl Peptide Fmlf Promotes Obesity-Induced Glucose
Page 1 of 230 Diabetes Title: The microbiota-produced N-formyl peptide fMLF promotes obesity-induced glucose intolerance Joshua Wollam1, Matthew Riopel1, Yong-Jiang Xu1,2, Andrew M. F. Johnson1, Jachelle M. Ofrecio1, Wei Ying1, Dalila El Ouarrat1, Luisa S. Chan3, Andrew W. Han3, Nadir A. Mahmood3, Caitlin N. Ryan3, Yun Sok Lee1, Jeramie D. Watrous1,2, Mahendra D. Chordia4, Dongfeng Pan4, Mohit Jain1,2, Jerrold M. Olefsky1 * Affiliations: 1 Division of Endocrinology & Metabolism, Department of Medicine, University of California, San Diego, La Jolla, California, USA. 2 Department of Pharmacology, University of California, San Diego, La Jolla, California, USA. 3 Second Genome, Inc., South San Francisco, California, USA. 4 Department of Radiology and Medical Imaging, University of Virginia, Charlottesville, VA, USA. * Correspondence to: 858-534-2230, [email protected] Word Count: 4749 Figures: 6 Supplemental Figures: 11 Supplemental Tables: 5 1 Diabetes Publish Ahead of Print, published online April 22, 2019 Diabetes Page 2 of 230 ABSTRACT The composition of the gastrointestinal (GI) microbiota and associated metabolites changes dramatically with diet and the development of obesity. Although many correlations have been described, specific mechanistic links between these changes and glucose homeostasis remain to be defined. Here we show that blood and intestinal levels of the microbiota-produced N-formyl peptide, formyl-methionyl-leucyl-phenylalanine (fMLF), are elevated in high fat diet (HFD)- induced obese mice. Genetic or pharmacological inhibition of the N-formyl peptide receptor Fpr1 leads to increased insulin levels and improved glucose tolerance, dependent upon glucagon- like peptide-1 (GLP-1). Obese Fpr1-knockout (Fpr1-KO) mice also display an altered microbiome, exemplifying the dynamic relationship between host metabolism and microbiota. -

Zinc Finger Proteins: Getting a Grip On
Zinc finger proteins: getting a grip on RNA Raymond S Brown C2H2 (Cys-Cys-His-His motif) zinc finger proteins are members others, such as hZFP100 (C2H2) [11] and tristetraprolin of a large superfamily of nucleic-acid-binding proteins in TTP (CCCH) [12], are involved in histone pre-mRNA eukaryotes. On the basis of NMR and X-ray structures, we processing and the degradation of tumor necrosis factor know that DNA sequence recognition involves a short a helix a mRNA, respectively. In addition, there are reports of bound to the major groove. Exactly how some zinc finger dual RNA/DNA-binding proteins, such as the thyroid proteins bind to double-stranded RNA has been a complete hormone receptor (CCCC) [13] and the trypanosome mystery for over two decades. This has been resolved by the poly-zinc finger PZFP1 pre-mRNA processing protein long-awaited crystal structure of part of the TFIIIA–5S RNA (CCHC) [14]. Whether their interactions with RNA are complex. A comparison can be made with identical fingers in a based on the same mechanisms as protein–DNA binding TFIIIA–DNA structure. Additionally, the NMR structure of is an intriguing structural question that has remained TIS11d bound to an AU-rich element reveals the molecular unanswered until now. details of the interaction between CCCH fingers and single-stranded RNA. Together, these results contrast the What follows is an attempt to expose both similarities different ways that zinc finger proteins bind with high and differences between C2H2 zinc finger protein bind- specificity to their RNA targets. ing to RNA and DNA based on recent X-ray structures. -

Harmonization Project Document No. 4
This report contains the collective views of an international group of experts and does not necessarily represent the decisions or the stated policy of the World Health Organization, the International Labour Organization, or the United Nations Environment Programme. Harmonization Project Document No. 4 PART 1: IPCS FRAMEWORK FOR ANALYSING THE RELEVANCE OF A CANCER MODE OF ACTION FOR HUMANS AND CASE-STUDIES PART 2: IPCS FRAMEWORK FOR ANALYSING THE RELEVANCE OF A NON-CANCER MODE OF ACTION FOR HUMANS This project was conducted within the IPCS project on the Harmonization of Approaches to the Assessment of Risk from Exposure to Chemicals. Published under the joint sponsorship of the World Health Organization, the International Labour Organization, and the United Nations Environment Programme, and produced within the framework of the Inter-Organization Programme for the Sound Management of Chemicals. The International Programme on Chemical Safety (IPCS), established in 1980, is a joint venture of the United Nations Environment Programme (UNEP), the International Labour Organization (ILO), and the World Health Organization (WHO). The overall objectives of the IPCS are to establish the scientific basis for assessment of the risk to human health and the environment from exposure to chemicals, through international peer review processes, as a prerequisite for the promotion of chemical safety, and to provide technical assistance in strengthening national capacities for the sound management of chemicals. The Inter-Organization Programme for the Sound Management of Chemicals (IOMC) was established in 1995 by UNEP, ILO, the Food and Agriculture Organization of the United Nations, WHO, the United Nations Industrial Development Organization, the United Nations Institute for Training and Research, and the Organisation for Economic Co-operation and Development (Participating Organizations), following recommendations made by the 1992 UN Conference on Environment and Development to strengthen cooperation and increase coordination in the field of chemical safety. -

Exogenous PPAR 2 but Not PPAR 1 Reactivates Adipogenesis
Downloaded from genesdev.cshlp.org on September 23, 2021 - Published by Cold Spring Harbor Laboratory Press RESEARCH COMMUNICATION ␥ differential isoform function. Rationally engineered PPAR knockdown by transcription factors potentially provide a powerful tool engineered transcription for targeted regulation of endogenous genes by combin- ing a functional transcription regulatory domain with a factors: exogenous PPAR␥2 customized DNA binding domain that can bind to a spe- but not PPAR␥1 cific sequence within the target gene. C2H2 zinc finger proteins (ZFPs) can be engineered to bind with high reactivates adipogenesis specificity to wide a diversity of DNA sequences (Des- jarlais and Berg 1992; Choo and Klug 1994; Jamieson et Delin Ren,1 Trevor N. Collingwood,2 al. 1994; Rebar and Pabo 1994; Greisman and Pabo 1997). Edward J. Rebar,2 Alan P. Wolffe,2 Previous studies have demonstrated the utility of both and Heidi S. Camp1,3 engineered activator- and repressor-ZFPs in the regula- tion of endogenous chromosomal loci (Bartsevich and 1Department of Molecular Science and Technology, Pfizer Juliano 2000; Beerli et al. 2000; Zhang et al. 2000; Liu et Global and Research Development, Ann Arbor, Michigan al. 2001). Our goal for this study was to selectively in- 48105, USA; 2Sangamo BioSciences Inc., Pt. Richmond, hibit expression of the PPAR␥2 isoform in the adipo- California 94804, USA genic mouse 3T3-L1 cell line by utilizing engineered zinc finger repressor proteins. To determine functional differences between the two splice variants of PPAR␥ (␥1 and ␥2), we sought to se- Results and Discussion ␥ lectively repress 2 expression by targeting engineered The mouse PPAR␥ gene spans >105 kb (Zhu et al. -

PARP13 Regulates Cellular Mrna Post-Transcriptionally and Functions As a Pro-Apoptotic Factor by Destabilizing TRAILR4 Transcript
ARTICLE Received 4 Sep 2014 | Accepted 23 Sep 2014 | Published 10 Nov 2014 DOI: 10.1038/ncomms6362 PARP13 regulates cellular mRNA post-transcriptionally and functions as a pro-apoptotic factor by destabilizing TRAILR4 transcript Tanya Todorova1,2, Florian J. Bock2 & Paul Chang1,2 Poly(ADP-ribose) polymerase-13 (PARP13/ZAP/ZC3HAV1) is an antiviral factor, active against specific RNA viruses such as murine leukaemia virus, Sindbis virus and human immunodeficiency virus. During infection, PARP13 binds viral RNA via its four CCCH-type zinc-finger domains and targets it for degradation by recruiting cellular messenger RNA (mRNA) decay factors such as the exosome complex and XRN1. Here we show that PARP13 binds to and regulates cellular mRNAs in the absence of viral infection. Knockdown of PARP13 results in the misregulation of hundreds of transcripts. Among the most upregulated transcripts is TRAILR4 that encodes a decoy receptor for TRAIL—a pro-apoptotic cytokine that is a promising target for the therapeutic inhibition of cancers. PARP13 destabilizes TRAILR4 mRNA post-transcriptionally in an exosome-dependent manner by binding to a region in its 30 untranslated region. As a consequence, PARP13 represses TRAILR4 expression and increases cell sensitivity to TRAIL-mediated apoptosis, acting as a key regulator of the cellular response to TRAIL. 1 Department of Biology, Massachusetts Institute of Technology, 500 Main Street, Cambridge, Massachusetts 02139, USA. 2 Koch Institute for Integrative Cancer Research, Massachusetts Institute of Technology, 500 Main Street, Cambridge, Massachusetts 02139, USA. Correspondence and requests for materials should be addressed to P.C. (email: [email protected]). NATURE COMMUNICATIONS | 5:5362 | DOI: 10.1038/ncomms6362 | www.nature.com/naturecommunications 1 & 2014 Macmillan Publishers Limited. -
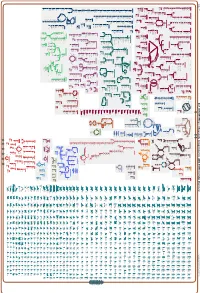
Generate Metabolic Map Poster
Authors: Pallavi Subhraveti Ron Caspi Peter Midford Peter D Karp An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Ingrid Keseler Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. Gcf_003855395Cyc: Shewanella livingstonensis LMG 19866 Cellular Overview Connections between pathways are omitted for legibility.