CHOP Chemotherapy for the Treatment of Canine Multicentric Tcell Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hodgkin Lymphoma Treatment Regimens
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 5) Clinical Trials: The National Comprehensive Cancer Network recommends cancer patient participation in clinical trials as the gold standard for treatment. Cancer therapy selection, dosing, administration, and the management of related adverse events can be a complex process that should be handled by an experienced health care team. Clinicians must choose and verify treatment options based on the individual patient; drug dose modifications and supportive care interventions should be administered accordingly. The cancer treatment regimens below may include both U.S. Food and Drug Administration-approved and unapproved indications/regimens. These regimens are provided only to supplement the latest treatment strategies. These Guidelines are a work in progress that may be refined as often as new significant data become available. The NCCN Guidelines® are a consensus statement of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way. Classical Hodgkin Lymphoma1 Note: All recommendations are Category 2A unless otherwise indicated. Primary Treatment Stage IA, IIA Favorable (No Bulky Disease, <3 Sites of Disease, ESR <50, and No E-lesions) REGIMEN DOSING Doxorubicin + Bleomycin + Days 1 and 15: Doxorubicin 25mg/m2 IV push + bleomycin 10units/m2 IV push + Vinblastine + Dacarbazine vinblastine 6mg/m2 IV over 5–10 minutes + dacarbazine 375mg/m2 IV over (ABVD) (Category 1)2-5 60 minutes. -

HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 2)
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 2) The selection, dosing, and administration of anticancer agents and the management of associated toxicities are complex. Drug dose modifications and schedule and initiation of supportive care interventions are often necessary because of expected toxicities and because of individual patient variability, prior treatment, and comorbidities. Thus, the optimal delivery of anticancer agents requires a healthcare delivery team experienced in the use of such agents and the management of associated toxicities in patients with cancer. The cancer treatment regimens below may include both FDA-approved and unapproved uses/regimens and are provided as references only to the latest treatment strategies. Clinicians must choose and verify treatment options based on the individual patient. NOTE: GREY SHADED BOXES CONTAIN UPDATED REGIMENS. REGIMEN DOSING Classical Hodgkin Lymphoma—First-Line Treatment General treatment note: Routine use of growth factors is not recommended. Leukopenia is not a factor for treatment delay or dose reduction (except for escalated BEACOPP).1 CR=complete response IPS=International Prognostic Score PD=progressive disease PFTs=pulmonary function tests PR=partial response RT=radiation therapy SD=stable disease Stage IA, IIA Favorable ABVD (doxorubicin [Adriamycin] Days 1 and 15: Doxorubicin 25mg/m2 IV + bleomycin 10mg/m2 IV + vinblastine + bleomycin + vinblastine + 6mg/m2 IV + dacarbazine 375mg/m2 IV. dacarbazine [DTIC-Dome]) + Repeat cycle every 4 weeks for 2–4 cycles. involved-field radiotherapy (IFRT)1–4 Follow with IFRT after completion of chemotherapy. Abbreviated Stanford V Weeks 1, 3, 5 and 7: Vinblastine 6mg/m2 IV + doxorubicin 25mg/m2 IV. (doxorubicin + vinblastine + Weeks 1 and 5: Mechlorethamine 6mg/m2. -

(Rituxan®), Rituximab-Abbs (Truxima®), Rituximab-Pvvr (Ruxience®) Prior Authorization Drug Coverage Policy
1 Rituximab Products: Rituximab (Rituxan®), Rituximab-abbs (Truxima®), Rituximab-pvvr (Ruxience®) Prior Authorization Drug Coverage Policy Effective Date: 2/1/2021 Revision Date: n/a Review Date: 7/2/20 Lines of Business: Commercial Policy type: Prior Authorization This Drug Coverage Policy provides parameters for the coverage of rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®). Consideration of medically necessary indications are based upon U.S. Food and Drug Administration (FDA) indications, recommended uses within the Centers of Medicare & Medicaid Services (CMS) five recognized compendia, including the National Comprehensive Cancer Network (NCCN) Drugs & Biologics Compendium (Category 1 or 2A recommendations), and peer-reviewed scientific literature eligible for coverage according to the CMS, Medicare Benefit Policy Manual, Chapter 15, section 50.4.5 titled, “Off- Label Use of Anti-Cancer Drugs and Biologics.” This policy evaluates whether the drug therapy is proven to be effective based on published evidence-based medicine. Drug Description1-3 Rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®) are monoclonal antibodies that target the CD20 antigen expressed on the surface of pre-B and mature B- lymphocytes. Upon binding to cluster of differentiation (CD) 20, rituximab mediates B-cell lysis. Possible mechanisms of cell lysis include complement dependent cytotoxicity (CDC) and antibody dependent cell mediated cytotoxicity (ADCC). B cells are believed to play a role in the pathogenesis of rheumatoid arthritis (RA) and associated chronic synovitis. In this setting, B cells may be acting at multiple sites in the autoimmune/inflammatory process, including through production of rheumatoid factor (RF) and other autoantibodies, antigen presentation, T-cell activation, and/or proinflammatory cytokine production. -
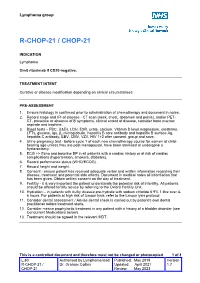
R-Chop-21 / Chop-21
Lymphoma group R-CHOP-21 / CHOP-21 INDICATION Lymphoma Omit rituximab if CD20-negative. TREATMENT INTENT Curative or disease modification depending on clinical circumstances PRE-ASSESSMENT 1. Ensure histology is confirmed prior to administration of chemotherapy and document in notes. 2. Record stage and IPI of disease - CT scan (neck, chest, abdomen and pelvis), and/or PET- CT, presence or absence of B symptoms, clinical extent of disease, consider bone marrow aspirate and trephine. 3. Blood tests – FBC, U&Es, LDH, ESR, urate, calcium, Vitamin D level,magnesium, creatinine, LFTs, glucose, Igs, β2 microglobulin, hepatitis B core antibody and hepatitis B surface Ag, hepatitis C antibody, EBV, CMV, VZV, HIV 1+2 after consent, group and save. 4. Urine pregnancy test • before cycle 1 of each new chemotherapy course for women of child- bearing age unless they are post-menopausal, have been sterilised or undergone a hysterectomy. 5. ECG +/- Echo and baseline BP in all patients with a cardiac history or at risk of cardiac complications (hypertension, smokers, diabetes). 6. Record performance status (WHO/ECOG). 7. Record height and weight. 8. Consent - ensure patient has received adequate verbal and written information regarding their disease, treatment and potential side effects. Document in medical notes all information that has been given. Obtain written consent on the day of treatment. 9. Fertility - it is very important the patient understands the potential risk of infertility. All patients should be offered fertility advice by referring to the Oxford Fertility Unit. 10. Hydration – in patients with bulky disease pre-hydrate with sodium chloride 0.9% 1 litre over 4- 6 hours. -

Anaplastic Large Cell Lymphoma (ALCL)
Helpline (freephone) 0808 808 5555 [email protected] www.lymphoma-action.org.uk Anaplastic large cell lymphoma (ALCL) This page is about anaplastic large-cell lymphoma (ALCL), a type of T-cell lymphoma. On this page What is ALCL? Who gets it? Symptoms Treatment Relapsed and refractory ALCL Research and targeted treatments We have separate information about the topics in bold font. Please get in touch if you’d like to request copies or if you would like further information about any aspect of lymphoma. Phone 0808 808 5555 or email [email protected]. What is ALCL? Anaplastic large cell lymphoma (ALCL) is a type of T-cell lymphoma – a non-Hodgkin lymphoma that develops from white blood cells called T cells. Under a microscope, the cancerous cells in ALCL look large, undeveloped and very abnormal (‘anaplastic’). There are four main types of ALCL. They have complicated names based on their features and the types of proteins they make: • ALK-positive ALCL (also known as ALK+ ALCL) is the most common type. In ALK-positive ALCL, the abnormal T cells have a genetic change (mutation) that means they make a protein called ‘anaplastic lymphoma kinase’ (ALK). In other words, they test positive for ALK. ALK-positive ALCL is a fast-growing (high-grade) lymphoma. Page 1 of 6 © Lymphoma Action • ALK-negative ALCL (also known as ALK- ALCL) is a high-grade lymphoma that accounts for around 3 in every 10 cases of ALCL. The abnormal T cells do not make the ALK protein – they test negative for ALK. -
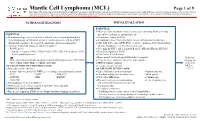
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -

Bendamustine in Combination with Gemcitabine and Vinorelbine Is An
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Archivio istituzionale della ricerca - Università di Modena e Reggio Emilia VOLUME 34 • NUMBER 27 • SEPTEMBER 20, 2016 JOURNAL OF CLINICAL ONCOLOGY ORIGINAL REPORT Bendamustine in Combination With Gemcitabine and Vinorelbine Is an Effective Regimen As Induction Chemotherapy Before Autologous Stem-Cell Transplantation for Relapsed or Refractory Hodgkin Lymphoma: Final Results of a Multicenter Phase II Study Armando Santoro, Rita Mazza, Alessandro Pulsoni, Alessandro Re, Maurizio Bonfichi, Vittorio Ruggero Zilioli, Flavia Salvi, Francesco Merli, Antonella Anastasia, Stefano Luminari, Giorgia Annechini, Manuel Gotti, Annalisa Peli, Anna Marina Liberati, Nicola Di Renzo, Luca Castagna, Laura Giordano, and Carmelo Carlo-Stella Armando Santoro, Rita Mazza, Luca Castagna, Laura Giordano, and Carmelo ABSTRACT Carlo-Stella, Humanitas Cancer Center; Armando Santoro, Humanitas University, Purpose Rozzano; Alessandro Pulsoni and Giorgia This multicenter, open-label, phase II study evaluated the combination of bendamustine, gemci- Annechini, Sapienza University, Rome; tabine, and vinorelbine (BeGEV) as induction therapy before autologous stem-cell transplantation Alessandro Re, Antonella Anastasia, and (ASCT) in patients with relapsed or refractory Hodgkin lymphoma (HL). Annalisa Peli, Spedali Civili, Brescia; Maurizio Bonfichi and Manuel Gotti, Patients and Methods Istituto di Ricovero e Cura a Carattere Patients with HL who were refractory to or had relapsed after one previous chemotherapy line were Scientifico (IRCCS) Policlinico San Matteo, eligible. The primary end point was complete response (CR) rate after four cycles of therapy. Pavia; Vittorio Ruggero Zilioli, Niguarda Ca’ Granda Hospital; Carmelo Carlo-Stella, Secondary end points were: overall response rate, stem-cell mobilization activity, and toxicity. -
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’S Lymphomas Version 2.2015
NCCN Guidelines Index NHL Table of Contents Discussion NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’s Lymphomas Version 2.2015 NCCN.org Continue Version 2.2015, 03/03/15 © National Comprehensive Cancer Network, Inc. 2015, All rights reserved. The NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN® . Peripheral T-Cell Lymphomas NCCN Guidelines Version 2.2015 NCCN Guidelines Index NHL Table of Contents Peripheral T-Cell Lymphomas Discussion DIAGNOSIS SUBTYPES ESSENTIAL: · Review of all slides with at least one paraffin block representative of the tumor should be done by a hematopathologist with expertise in the diagnosis of PTCL. Rebiopsy if consult material is nondiagnostic. · An FNA alone is not sufficient for the initial diagnosis of peripheral T-cell lymphoma. Subtypes included: · Adequate immunophenotyping to establish diagnosisa,b · Peripheral T-cell lymphoma (PTCL), NOS > IHC panel: CD20, CD3, CD10, BCL6, Ki-67, CD5, CD30, CD2, · Angioimmunoblastic T-cell lymphoma (AITL)d See Workup CD4, CD8, CD7, CD56, CD57 CD21, CD23, EBER-ISH, ALK · Anaplastic large cell lymphoma (ALCL), ALK positive (TCEL-2) or · ALCL, ALK negative > Cell surface marker analysis by flow cytometry: · Enteropathy-associated T-cell lymphoma (EATL) kappa/lambda, CD45, CD3, CD5, CD19, CD10, CD20, CD30, CD4, CD8, CD7, CD2; TCRαβ; TCRγ Subtypesnot included: · Primary cutaneous ALCL USEFUL UNDER CERTAIN CIRCUMSTANCES: · All other T-cell lymphomas · Molecular analysis to detect: antigen receptor gene rearrangements; t(2;5) and variants · Additional immunohistochemical studies to establish Extranodal NK/T-cell lymphoma, nasal type (See NKTL-1) lymphoma subtype:βγ F1, TCR-C M1, CD279/PD1, CXCL-13 · Cytogenetics to establish clonality · Assessment of HTLV-1c serology in at-risk populations. -

Analysis Compared with Classical Hodgkin Lymphoma
From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. 2014 123: 3567-3573 doi:10.1182/blood-2013-12-541078 originally published online April 8, 2014 Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. Xing, Joseph M. Connors, Anky Lai, Mubarak Al-Mansour, Laurie H. Sehn, Diego Villa, Richard Klasa, Tamara Shenkier, Randy D. Gascoyne, Brian Skinnider and Kerry J. Savage Updated information and services can be found at: http://bloodjournal.hematologylibrary.org/content/123/23/3567.full.html Articles on similar topics can be found in the following Blood collections Clinical Trials and Observations (3892 articles) Free Research Articles (2531 articles) Lymphoid Neoplasia (1767 articles) Information about reproducing this article in parts or in its entirety may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://bloodjournal.hematologylibrary.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. Regular Article CLINICAL TRIALS AND OBSERVATIONS Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. -

Bendamustine Plus Rituximab: Is It a BRIGHT Idea?
Editorial Commentary Page 1 of 4 Bendamustine plus rituximab: is it a BRIGHT idea? Carlo Visco1, Francesca Maria Quaglia1, Chiara Bovo2, Maria Chiara Tisi3, Mauro Krampera1 1Department of Medicine, Section of Hematology, University of Verona, Verona, Italy; 2Medical Direction, University Hospital of Verona, Verona, Italy; 3Cell Therapy and Hematology, San Bortolo Hospital, Vicenza, Italy Correspondence to: Carlo Visco, MD. Associate Professor of Hematology, Department of Medicine, Section of Hematology, University of Verona, P.le L.A. Scuro 10, 37134 Verona, Italy. Email: [email protected]. Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Xinyi Du (Department of Hematology, Northern Jiangsu People’s Hospital, Yangzhou, China). Comment on: Flinn IW, van der Jagt R, Kahl B, et al. First-Line Treatment of Patients With Indolent Non-Hodgkin Lymphoma or Mantle-Cell Lymphoma With Bendamustine Plus Rituximab Versus R-CHOP or R-CVP: Results of the BRIGHT 5-Year Follow-Up Study. J Clin Oncol 2019;37:984-91. Submitted Sep 20, 2019. Accepted for publication Oct 14, 2019. doi: 10.21037/cco.2019.10.03 View this article at: http://dx.doi.org/10.21037/cco.2019.10.03 Flinn et al. have reported the results of the long-term in the BRIGHT study were eagerly awaited. As the Stil- follow-up for the BRIGHT trial, an international study 1 trial, the BRIGHT study (3) included patients with which compared the efficacy and the safety of bendamustine follicular lymphoma (grade 1 or 2, excluding grade 3A), plus rituximab (BR) with either rituximab plus lymphoplasmacytic lymphoma, splenic marginal zone B-cell cyclophosphamide, doxorubicin, vincristine, and prednisone lymphoma, extranodal marginal zone lymphoma (MZL) (R-CHOP) or rituximab plus cyclophosphamide, vincristine, of mucosa-associated lymphoid tissue type, nodal marginal and prednisone (R-CVP) for treatment-naive patients with zone B-cell lymphoma (371 patients with iNHL), or MCL indolent non-Hodgkin lymphoma (iNHL) or mantle-cell (74 patients). -

Dacarbazine for Injection, USP
DACARBAZINE - dacarbazine injection, powder, for solution Fresenius Kabi USA, LLC ---------- Dacarbazine for Injection, USP WARNING It is recommended that dacarbazine be administered under the supervision of a qualified physician experienced in the use of cancer chemotherapeutic agents. 1. Hemopoietic depression is the most common toxicity with dacarbazine (see WARNINGS). 2. Hepatic necrosis has been reported (see WARNINGS). 3. Studies have demonstrated this agent to have a carcinogenic and teratogenic effect when used in animals. 4. In treatment of each patient, the physician must weigh carefully the possibility of achieving therapeutic benefit against the risk of toxicity. DESCRIPTION Dacarbazine for Injection, USP is a white to pale yellow colored solid which is light sensitive. Each vial contains 100 mg of dacarbazine, or 200 mg of dacarbazine (the active ingredient), anhydrous citric acid and mannitol. Dacarbazine for Injection, USP is reconstituted and administered intravenously (pH 3- 4). Dacarbazine for Injection, USP is an anticancer agent. Chemically, dacarbazine is 5-(3,3-Dimethyl- 1-triazeno) imidazole-4-carboxamide with the following structural formula: M.W. 182.19 C 6H 10N 6O CLINICAL PHARMACOLOGY After intravenous administration of dacarbazine for injection, the volume of distribution exceeds total body water content suggesting localization in some body tissue, probably the liver. Its disappearance from the plasma is biphasic with initial half-life of 19 minutes and a terminal half-life of 5 hours. 1 In a patient with renal and hepatic dysfunctions, the half-lives were lengthened to 55 minutes and 7.2 hours. 1 The average cumulative excretion of unchanged dacarbazine in the urine is 40% of the injected dose in 6 hours. -

Anti Cancer Chemotherapy
Anti Cancer Chemotherapy __/03/2020 BY Miss Isha Talwar Assistant Professor Glocal school of Pharmacy Glocal University • Cancer – Uncontrolled multiplication and spread within the body of abnormal forms of body's own cells • Neoplasm – A mass of tissue formed as a result of • Abnormal • Excessive • Uncoordinated • Autonomous and • purposeless Proliferation of cells Why term chemotherapy • Like infective disease – Some malignant cells can be cultured – Some malignancies can be transmitted by innoculation Cancer chemotherapy not as successful as antimicrobial chemotherapy • Metabolism in parasite differs qualitatively from host cells, while metabolism in cancer cells differ only quantitatively from normal host cells – Hence target selectivity is more difficult in cancer – cancer there is no substantial immune response – Diagnostic complexity: delay in institution of treatment Modalities of treatment in cancer • Surgery 1/3 of patients can be cured, effective • Radiotherapy when tumor has not metastasized • Chemotherapy: 50 % of the patients can be treated with chemotherapy contributing to cure in 15 -20 % of patients Cancer chemotherapy can be curative in • Acute Leukemias • Wilm’s Tumour In children • Ewing’s Sarcoma • Choriocarcinoma • Hodgkin’s Disease • Lymphosarcoma • Burkitts lymphoma • Testicular Teratomas • Seminomas Chemotherapy can have only Palliative effect in • Breast Cancer • Ovarian Cancer • Endometrial Cancer • Prostatic Cancer • Chronic Lymphatic Leukemia • Chronic Myeloid Leukemia • Head & Neck Cancer • Lung (small cell)